Lower GI Checklist and Referral Final
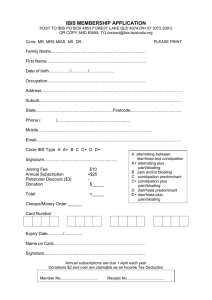
advertisement

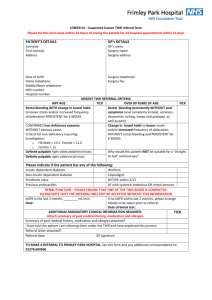
SUSPECTED IRRITABLE BOWEL SYNDROME Onset of Symptoms < age 40 and lasting more than 6 months GSTT Contact details: KCH Other Address Phone Email Referral Date Referring Clinician Practice Details ~[Today...] ~[Free Text:Referring Clinician?] ~[Surgery Address Line 1] ~[Surgery Address Line 2] ~[Surgery Address Line 3] ~[Surgery Address Line 4] ~[Surgery Tel No.] Patient Name DOB ~[Forename] ~[Surname] ~[Date Of Birth] Patient Address ~[Patient Address Block] Patient Tel Mobile NHS Number Hospital Number ~[Telephone Number] ~[Mobile]~[Mobile Number] ~[NHS Number] ~[Hospital Number] Referral Checklist Prior to referral please review this chart below and offer a trial of dietary changes +/- medication according to the dominant symptoms Symptoms Diet Medication Constipation no Bloating/Gas - High-fibre □ Laxative □ Constipation + Bloating/Gas - Low-fibre + Ispaghula Husk □ Mebeverine □ Peppermint oil □ Loperamide □ Diarrhoea (irrespective Gas) Mixed no Bloating/Gas Mixed + Bloating/Gas - Low-fibre □ - Low-FODMAP □ - High-fibre or Ispaghula Husk □ - Low-FODMAP - - Low-fibre + Ispaghula Husk - □ Treatment guided by predominant symptom □ Mebeverine □ □ Peppermint oil □ - Low-FODMAP Please circle the dominant symptoms and tick treatment given. Final Version – February 2013 □ Have you considered the 2 week wait criteria e.g. weight loss, anaemia □ Straining/Rectal Symptoms (If yes, please refer to Pelvic Floor Unit) Lifestyle advice offered □ Dietary advice offered □ Physical exam. (incl PR) done □ Findings: Investigations All cases: Please perform the following diagnostic tests prior to referral FBC, U/Es, eGFr, LFTs, Coeliac Screen, F. Calprotectin* Normal □ + Diarrhoea ± Bloating-Flatus: Stool c/s Normal □ + Constipation: TSH, Calcium Normal □ + Lower Abdo Pain (female): U/S Pelvis Normal □ Normal □ Ca125 Psychological Assessment done* □ CBT □ Information Faecal Calprotectin: Normal upper limit is 100. If result is in between 100-150, please repeat and if normal, then refer along this pathway. History: An exact description of symptoms and associated symptoms with start date, circumstances (travel, BBQ, change life-style/diet), aggravating/relieving factors, systemic symptoms, past medical/family histories. Psychological Assessment: eating habits, symptom timing to life-events, stress/anxiety, and impact of symptoms /remedial actions on lifestyle/psych. Consider GAD7/PHQ9. FODMAP diet information please see: http://www.bda.uk.com/publications/IBSdietary_resource.pdf Final Version – February 2013