الأسبوع الØ..
advertisement
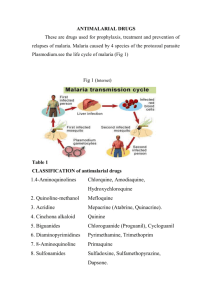
Antiparasitic Drugs References - Rang & Dale’s Pharmacology 6th edition Capter # 49 & 50 - Classroom materials and lectures. Parasitic diseases - - • • Parasitic are a serious health problem worldwide. Malaria 300-500 million infection and one 1-3 million died annually. Most of parasitic infection are common in underdeveloped areas of the world (tropical-subtropical countries) where much poverty is existed and associated with inadequate sanitary conditions, and hygienic practice. Parasitic diseases are infectious diseases caused or transmitted by parasite. Parasitic diseases can affect practically all living organisms, including plants and mammals. Some parasites can cause disease directly, or by the toxins that they produce. Two main routes that used by parasites to invade mammalian host body, the skin and mouth. Four main mechanisms for parasitic transfer: Ingestion of contaminated food or water (egs or larval stages…etc) - Ascaris - Entamoeba The infective stage of the parasite can burrow into the skin of the host - Schistosoma cercaria The larva of the parasite can move from person to person through bug bites (insect vector) - Trypanosomes - Plasmodia Sexual transmission - Trichomonas vaginalis - Pubic lice What are parasites? By definition parasites are organisms that are obligated to live with host to survive. Parasites Include: (1) protozoa: • • • They are a diverse group of single cell eukaryotic organisms, many of which are motile. Classified mainly according to mode of locomotion (They move around with whiplike tails called flagella, hair-like structures called cilia, or foot-like structures called pseudopodia. Others do not move at all) Reproduce by binary fission at some point in life cycle • Examples of human diseases caused by protozoal infections: - Amoebiasis (Entamoeba histolytica) - Giardiasis (Giardia lamblia) - Trichmoniasis (Trichomonas vaginalis) - Trypanosomiasis “Sleeping sickness Africa; Chagas Disease - South America” (Trypanosoma spp.) - Toxoplasmosis (Toxoplasma gondii) - Malaria (Plasmodium spp) (2) Helminths (worms) • • • Multicellular parasites that, live inside their host. They are worm-like organisms that live and feed off living hosts, receiving nourishment and protection while disrupting their hosts' nutrient absorption, causing weakness and disease. They live in a large variety of tissues, though many are specialized to single tissues such as muscle, vein, brain, or intestine. Helminthes are classified into: (a) Cestodes (tapeworms) Examples of tapeworms that infect humans include: 1- Beef tapeworm (Taenia saginata) and Pork tapeworm (Taenia solium) Taeniasis 2- Fish tapeworm (Diphyllobothrium latum) Diphyllobothriasis (b) Trematodes (flukes or flat worms) Example of flukes that infect humans include: 1- Intestinal fluke (Fasciolopsis buski) Fasciolopsiasis 2- Blood fluke (Schistosoma japonicum, Schistosoma mansoni, Schistosoma haematobium) Schistosomiasis 3- Liver fluke (Fasciola hepatica, Fasciola gigantica) Fascioliasis (c) Nematodes (roundworms) Examples of tapeworms that infect humans include: 1- Enterobius vermicularis Enterobiasis (oxiyoriasis) 2- Ascaris lumbricoides Ascariasis 3- Ancylostoma duodenale (hookworm) Ancylostomiasis 4- Wuchereria bancrofti (flaria) Flariasis (elephentiasis) (3) Ectoparasites Organisms that live on the outer surface of another organism, its host, and which does not contribute to the survival of the host Examples of ectoparasites affect human: 1- Human fleas 2- Human lice ( body louse, Head louse, and Pubic or crab louse ) 3- Ticks 4- Mites (Dust mites , Itch mites (Sarcoptes scabiei) that cause the condition known as scabies. Antiprptozoal drugs Anti-Protozoal Drugs are medications used to treat infections or diseases caused by Protozoa. These drugs aim to destroy protozoa or prevent their growth and ability to reproduce. They are available in many pharmaceutical forms (liquid, tablet, and injectable forms). The challenges associated with protozoal infections is that protozoa are eukaryotic organisms which have metabolic processes close to those of human host than procaryotic bacterial pathogens. Thus parasitic diseases are less easily to be treated than bacterial infections and antiprotozoal drugs are more toxic. I-Drugs Used in Treatment of Amoebiasis • • • Amoebiasis (entamoebiasis or amoebic dysentry) is a gastrointestinal pathological condition caused by the proatozoal parasite Entamoeba histolytica (amoeba). This protozoan is distributed throughout the world and is commonly acquired by ingestion of contaminated food or water. It is estimated that about 40 to 50 million people infected with E. histolytica worldwide. Up to 100,000 deaths per year may occur from the most sever forms of amoebiasis. It is considered to be the second leading cause of death from parasitic diseases worldwide. Pathogenesis: • • • • • • • Amoebiasis is usually transmitted by the fecal-oral route through ingestion food or water contaminated with the cyst (entamoeba infective stage) a semi-dormant and hardy structure form of the parasite, found mainly in feces of infected individuals. A gastrointestinal infection that may or may not be asymptomatic (in almost 8090% of cases) and can remain latent in an infected person for several years. When no symptoms are present, the infected individual is still a carrier, able to spread the parasite to others through poor hygienic practices. Symptoms can range from mild diarrhea to dysentery (sever diarrhea with blood and mucus in the stool) in association of abdominal cramps. Severe amoebiasis infections (known as invasive or fulminant amoebiasis) occur in two major forms. Invasion of the intestinal lining causes amoebic dysentery or amoebic colitis due to sloughing of intestinal wall. If the parasite reaches the bloodstream it can spread through the body, most frequently ending up in the liver where it causes amoebic liver abscesses. Liver abscesses can occur without previous development of amoebic dysentery. Lung and brain tissues may also be attached. Treatment of amoebiasis: • • • The use of drugs to treat this condition depends largely on the site and type of infection, as different drugs are differentially effective in acute amoebic dysentery, in chronic intestinal amoebiasis, in extraintestinal infection and in the carrier state. The main drugs currently used are metronidazole, tinidazole , diloxanide. iodoquinol, dehydroemetine and paromomycin. These agents may be used either as monotherapy in combination. For example: -Tissue amoebicides ides like Metronidazole (or a related drug such as tinidazole) followed by luminal amobicides like Iodoquinol or diloxanide for acute invasive intestinal amoebiasis resulting in acute severe amoebic dysentery - Iodoquinol, Paromomycin, or Diloxanide for chronic intestinal amoebiasis (mild symptoms) - Metronidazole (or tinidazole) followed by luminal amobicides like paromomycin, Iodoquinol or diloxanide for hepatic amoebiasis - Diloxanide , or Iodoquinol, Paromomycin for the carrier state (asymptomatic). (1)Nitroimidazole derivatives For examples: and Therapeutic Uses: • • • Nitroimidazole derivatives are group of drugs used for treatment of many parasitic infections like amoebiasis, trichomoniasis and giardiasis in addition to their use for treatment of anaerobic bacterial infections. Metronidazole, or a related drug such as Tinidazole, Secnidazole or Ornidazole have amebicidal activity. Metronidazole and congors kill the trophozoites of E. histolytica but has no effect on the cysts. It is the drug of choice for invasive amoebiasis of the intestine or the liver, but it is less effective against organisms in the lumen of the gut. Mechanism of action • • • • Metronidazole is selectively absorbed by anaerobic bacteria and sensitive protozoa. Once taken up by anaerobes, it is reduced by reacting with reduced ferredoxin to more toxic metabolites that accumulate and attack the protozoal (or bacterial) DNA, and form unstable molecules that leading to parasite apoptosis. This reduction usually happens only in anaerobic cells, it has relatively little effect upon human cells or aerobic bacteria. Tinidazole is chemically similar to metronidazole. It is used treatment for a variety protozoal infections including of amoebiasis. Tinidazole may be a therapeutic alternative in the setting of metronidazole tolerance. Pharmacokinetics: • • • • Metronidazole and tinidazole are usually given orally and are rapidly and completely absorbed, achieving peak plasma concentration in 1-3 hours, with t1/2about 7 hrs (metronidazole) or 12-14 hrs (tinidazole). Rectal and intravenous preparations are also available. They are distributed rapidly throughout the tissues, reaching high concentrations in the body fluids, including the cerebrospinal fluid. Some is metabolized, but most are excreted unchanged in urine (leading to dark urine). Unwanted Effects: • • • • • • Drugs have a metallic, bitter taste in mouth. Common adverse drug reactions (≥1% of patients) including GIT disturbances (nausea, vomiting and mild diarrhea). Some CNS symptoms may be experienced (dizziness, headache, sensory neuropathies). Infrequent adverse effects include: hypersensitivity reactions (rash, itch, flushing, fever and/or paraesthesia) The drug interferes with alcohol metabolism, and concurrent use of the substance thought to be associated with toxicity symptoms nausea, vomiting, flushing of the skin, tachycardia, and shortness of breath. Simultaneous administration should be strictly avoided. Drugs are contraindicated to be used during pregnancy. (2) Dichloroacetate derivatives Example: • • • • • • Both diloxanide and its insoluble ester, diloxanide furoate, are the drugs of choice for treatment of asymptomatic and chronic amoebiasis, and are often given as a follow-up after the disease has been reversed using metronidazole. Both drugs are effective luminal amebicide (parasites just before encystment.) but is not active against tissue trophozoites. In the gut, diloxanide furoate is split into diloxanide and furoic acid; about 90% of the diloxanide is rapidl absorbed and then conjugated to form the glucuronide, which is promptly excreted in the urine. Diloxanide furoate is given orally, the unabsorbed moiety being the amoebicidal agent the mechanism of action of diloxanide furoate is unknown. It is used with a tissue amebicide, usually metronidazole, to treat serious intestinal and extraintestinal infections. Diloxanide furoate has an excellent safety profile. Almost no ADRs , but fatulence may be experienced . The drug is not recommended in pregnancy. (3) Paromomycin Paromomycin is an aminoglycoside antibiotic, first isolated from Streptomyce krestomuceticus. • • • • • • It is designed to fight intestinal parasitic infections including amoebiasis and giardiasis. The main route of administration in case of GI protozoal infection is oral (in form of capsules) to treat mild form of amoebiasiss, and IM for management of severe form of amobiasis. Paromomycin acts by inhibition of protein synthesis by binding to 16S rRNA. Side effects: upon parentral administration ototoxicity and nephrotoxicity are most common. Drug is contraindicated in patients with impaired kidney function. Oral administration is associated with minimal adverse effects like GI distress and diarrhea. Its activity is lower than nitroimidazole derivatives ; however, because it is poorly absorbed by small intestine, a higher concentration of the drug remains in the lumen to combat the organisms. The drug is recommended to treat E. histolytica in resistant infection and during pregnancy (oral route). II- Drugs Used in Treatment of Giardiasis •Giardiasis (beaver fever) is a gastrointestinal pathological condition caused by the proatozoal organism called Giardia lamblia. •Giardiasis occurs worldwide with a prevalence of 20–30% in developing countries. Annually, about 200 million people worldwide are getting infected with giardiasis. •Giardia has a wide range of mammalian and non-mammalian hosts besides humans (e.g. beavers, dogs, cats, horses, cattle and many birds), thus making it very difficult to eradicate. •Giardiasis can be fatal for those patients with immunodeficiency, such as children, elderly and AIDS patients. Pathogenesis: •Giardiasis is usually transmitted by the fecal-oral route through ingestion food or water contaminated with faecal matter containing the cysts (giardia infective stage) that found mainly in feces of infected individuals. As few as 10 cysts can cause disease and up to 900,000,000 cysts can be released by an infected individual in one day. • Symptoms usually begin 1 to 2 weeks (average 7 days) after an individual becomes infected. In otherwise healthy individuals, symptoms may last 2 to 6 weeks. Though symptoms may last longer, medications can help decrease the duration of symptoms. •The trophozoite form of this parasite colonizes the upper part of GIT, and the cysts pass out in the faeces. Symptoms are caused by Giardia organisms coating the inside of the small intestine and blocking nutrient absorption • A range of clinical syndromes may occur, with gastrointestinal syndromes being the most prevalent. •There is no invasion of giardia trophozoites but their attachment to intestinal surface decreased expression of brush-border enzymes, morphological changes to the microvillous, and apoptosis of small intestinal epithelial cells. Gastrointestinal symptoms: •Only about 1/3 of infected people exhibit symptoms, while the major part of patients may last asymptomatic. Infected individuals experience an abrupt onset of abdominal cramps, frothy watery diarrhea, vomiting, flatulence , and fever which may last for 3– 4 days before proceeding into a more sub-acute phase. The majority of infected persons may have recurrent symptoms. •In most cases, stools become greasy and malodorous but do not contain blood or pus because giardiasis does not involve dysenteric symptoms. •Watery diarrhea may cycle with soft stools and constipation. Upper GI symptoms including nausea, early satiety, bloating, substernal burning, and acid indigestion may be exacerbated by eating. •Persistence of diarrhea may lead to chronic debilitation. Constitutional symptoms: • The most common constitutional symptoms are loss of appetite, malaise, and fatigue. Weight loss affects more than 50% of patients. Adults with long lasting malabsorption syndrome and children with failure to thrive may experience chronic illness. • Additional syndromes may include lactose intolerance, biliary tract disease and allergic manifestations such as bronchospasm and urticaria. Treatment : •Nitroimidazole derivatives (e.g. Metronidazole , Tinidazole) are the drugs of choice in treatment of giardiasis. In addition to many other drugs are also used to treat giardiasis like Nitazoxanid, Quinacrine, Furazolidone, Paramomycin, Albendazole, and Mebendazole. •In some cases Giardia parasites may show resistance to the common anti-giardial drugs, such as metronidazole, quinacrine, and albendazole. Treatment for truly resistant strains consists of three options: •Treating with the original drug for a longer period of time or at higher doses; •Using a drug from a different class to treat the resistant infection. This way considered the most efficacious approach. •Using a combination of different classes of drugs, such as metronidazole-albendazole and metronidazole-quinacrine. (1)Nitazoxanid •Nitazoxanideis a synthetic nitrothiazolyl derivative . •Nitazoxanide is a first-line choice for the treatment of infectious diarrhea caused by G. lamblia . It is also effective in treatment of many other protozoal (e.g. C. parvum) and helminthes (e.g. tapeworms) infections. •It is used in patients 1 year of age and older. Mechanism of action: •The anti-protozoal activity of nitazoxanide is assumed to be due to interference with the pyruvate-ferredoxin oxidoreductase (PFOR) enzyme-dependent electron transfer reaction which is essential step in energy metabolism. Pharmacokinetics: •Nitazoxanide is available in two oral dosage forms - tablet and oral suspension. It is a prodrug ; following oral administration, it is rapidly hydrolyzed to its active metabolite, tizoxanide which has the antiprotozoal activity. Tizoxanide is 99% protein bound. Peak concentrations are observed 1–4 hours after administration. It is excreted in the urine, bile and feces. Adverse effects: •Side effects are minimal (~3-6% of casaes) and mostly gastrointestinal (abdominal pain, dyspepsia , and constipation) , headache, dizziness, dry mouth, and yellow discoloration of urine . •The drug should be taken with food to minimize adverse effects. (2) Furazolidone •Furazolidone is a nitrofuran drivative. •It is used to treat diarrhoea and enteritis caused by some bacteria (e.g. salmonellosis) or protozoan (e.g. giardiasis) infections. •It is administered orally and has the ability to reach all body tissues and fluids like saliva, breast milk, semen and vaginal fluid Mechanism of action: •It is believed to work by crosslinking of DNA. Side effects: •Mainly GI symptoms (nausea, vomiting, diarrhea) are observed in 10% of patients. Other side effects include brown discoloration of urine, and hemolysis in G6PDHdeficient patients •Not recommended to treating pregnant patients (3) Quinacrine •Quinacrine is a drug with a number of different medical applications. It is used as an antiprotozoal ,anthelmintic (especially tapeworm infections), and in management of autoimmune disorders (like SLE) . •Antiprotozoal use include targeting malaria and Giardiasis. •Quinacrine is indicated as a primary antigiardiasis agent for patients with metronidazole-resistant giardiasis and patients who can not tolerate metronidazole. Giardiasis that is very resistant may even require a combination of quinacrine and metronidazol Mechanism of action: •Its mechanism of action against protozoa is thought to interference with the protozoan's cell membrane integrity. Side effects: •Bitter taste (less accepted in children patients), nausea , vomiting and yellow/orange discoloration of the skin, sclera, and urine are the most common side effects. •Other side effects include headache, dizziness and fever. •Qinacrine-induced psychosis has been observed in some patients. Dermatitis and drug-induced retinopathy may also observed (uncommon). •Drug is contraindicated in pregnant patients that it can cross placental barrier and cause fetal malformation (proven teratogenic).