2 Protozoa
advertisement
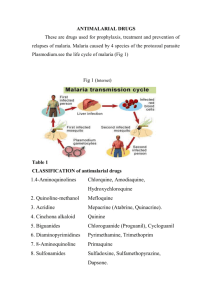
Anti-protozoal drug 1 INTRODUCTION: 2 Humans host a wide variety of protozoal parasites that can be transmitted by insect vectors, directly from other mammalian reservoirs or from one person to another. Because protozoa multiply rapidly in their hosts and effective vaccines are unavailable, chemotherapy has been the only practical way to both treat infected individuals and reduce transmission. Protozoa: 3 Basic Properties of Protozoa – Eukaryotic microorganisms – No cell walls – Most have heterotrophic metabolisms – A few protozoa (eg Euglena) are photosynthetic. – Many are free-living in soil or aquatic environments; a few are parasitic. – Single-celled or simple colonial organization – Classification based predominately on the mechanism of motility Cont.. Basic properties of protozoa “Trophozoite” and “Cyst” – – – – 4 Some protozoa go through different stages in their life cycle. This is especially true of certain parasitic protozoa. Trophozoite: Actively growing and reproducing stage Cyst: A dormant stage, enclosed in a resistant cyst coat Classification of protozoa 5 1)Class- Sarcodina Motile by pseudopodia & amoeboid movement Examples: – Amoeba – Entamoeba histolytica – Naegleria fowleri 3)Class - Ciliophora Motile by cilia Examples: – Paramecium – Balantidium coli 2) Class- Mastigophora Motile by flagella Examples: – Euglena – Giardia lamblia 4)Class -Sporozoa Most have complex life cycles with both sexual & asexual stages Adult forms are nonmotile Examples: – Plasmodium – Toxoplasma gondii Protozoan Diseases A. B. C. D. E. F. G. H. I. 6 Amebiasis Giardiasis Leishmeniasis: Primary Amoebic Meningoencephalitis Trichomoniasis Balantidiasis Malaria Pneumocystosis Toxoplasmosis Amoebiasis: 7 Two morphologically identical but genetically distinct species of Entamoeba (i.e., E. histolytica and E. dispar) have been isolated from infected persons. At the present time ,Entamoeba histolytica, is the causative agent of amebic dysentery and amebic liver abscess. Entamoeba dispar morphologically similar to E. histolytica is considered non-pathogenic at this time. Entamoeba Life Cycle 8 Entamoeba species exist in only two forms. The non-infective trophozoite stage and the ineffective cyst stage. Ineffective cysts are ingested by man. Some time after passing through the stomach and small bowel they excyst to form motile trophozoites. these trophozoites of E. histolytica that can penetrate, invade and colonize intestinal mucosa. As the trophozoite travels down the large bowel at some point when conditions are right , it encysts into the ineffective cyst stage and is excreted with the feces. www.practicalscience.com/introentamoeba.html PATHOLOGY: Flask-shaped ulcers: 9 E. histolytica invades mucosal cells of colonic epithelium, producing the classic flaskshaped ulcer in the submucosa. If the trophozoite gets into the portal circulation, it will be carried to the liver, where it produces abscess and periportal fibrosis. Amoebic ulcerations can affect the perineum and genitalia, and abscess may occur in the lung and brain. Manifestations: Intestinal Disease: Abdominal discomfort, severe abdominal cramps, flatulence, bloody diarrhea with mucus. Amoebic Liver Abscess: High fever, significant leukocytosis with left shift, elevated alkaline phosphatase. Hepatomegaly, and liver tenderness, with referred pain to the left or right shoulder Erosion of liver abscesses also present as peritonitis. 10 Antiamebic drugs: Tissue amoebicides: FOR BOTH INTESTINAL AND EXTRA INTESTINAL AMEBIASIS: Nitroimidzoles: Metronidazole, Tinidazole, Secnidazole,Ornidazole, Satranadazole Alkaloids: Emetine, Dehydroemetine FOR EXTRAINTESTINAL AMOEBIASIS ONLY: Chloroquine Luminal amoebicides: AMIDE: Diloxanide furote 8-HYDROXYQUINOLINES:Quiniodochlor (Iodochlorohydroxyquin,Clioquine), Diiodohydroxyquin (Idoquinol) ANTIBIOTICS: Tetracyclines, paromomycine sulfate. 11 Mechanisms 12 Inhibiting peptidyl-tRNA transposition → inhibiting elongation of peptide chain → inhibiting protein synthesis → interfering cleavage and breeding of trophozoites Treatment of Specific Forms of Amebiasis A. ASYMPTOMATIC INTESTINAL INFECTION: Asymptomatic carriers generally are not treated in endemic areas but in nonendemic areas they are treated with a luminal amebicide. A tissue amebicidal drug is unnecessary. Standard luminal amebicides are diloxanide furoate, iodoquinol, and paromomycin. Each drug eradicates carriage in about 80-90% of patients with a single course of treatment. Therapy with a luminal amebicide is also required in the treatment of all other forms of amebiasis. 13 Cont.. B. AMOEBIC COLITIS 14 Metronidazole + luminal amebicide is the treatment of choice for colitis and dysentery. Tetracyclines and erythromycin are alternative drugs for moderate colitis but are not effective against extraintestinal disease. Dehydroemetine or emetine can also be used, but are best avoided because of toxicity. Cont.. C. EXTRAINTESTINAL INFECTIONS 15 The treatment of choice is metronidazole plus a luminal amebicide. A 10-day course of metronidazole cures over 95% of uncomplicated liver abscesses. For unusual cases in which initial therapy with metronidazole has failed, aspiration of the abscess and the addition of chloroquine to a repeat course of metronidazole should be considered. Dehydroemetine and emetine are toxic alternative drugs. Metronidazole: Metronidazole is selectively toxic to anaerobic microorganisms. Mechanism of action: Metronidazole is a prodrug; it requires reductive activation of the nitro group by susceptible organisms. These anaerobic organisms contain electron transport components such as ferredoxins, small Fe-S proteins that have a sufficiently negative redox potential to donate electrons to metronidazole. The single electron transfer forms a highly reactive nitro radical anion that kills susceptible organisms by radicalmediated mechanisms that target DNA and possibly other vital biomolecules. 16 Cont.. Pharmacokinetics: 17 Metronidazole is almost completely absorbed from the small intestine: little unabsorbed drug reaches the colon. It is metabolized in liver primarily by oxidation and glucuronide conjugation and excreted in urine. Plasma t1/2 is 8 hrs. Unwanted effects & contraindication 18 GI-anorexia, diahorrea , headache ,abdominal cramp, unpleasant metallic taste , furry tongue. Hematological –leucopenia Renal-darkened urin,dysuria,cystitis Cardiac-t-wave flattening Hypersensitivity reaction- urticaria, erythematous rash, dry mouth Contraindicated in pregnancy Disulfiram like effect with alcohol Increase the action of warfarin Cont…. USES: Amoebiasis: Metronidazole is first line drug for all forms of amoebic infection. It is less effective than many luminal amebiasis in eradicating amoebic cysts from the colon. Giardiasis: It is highly effective. Trichomonas vaginitis; It is the drug of choice; 400mg TDS for 7 days achives nearly 100% cure. Additional intravaginal treatment has been given but only in refractory cases. Anaerobic bacterial infection: Metronidazole is generally used with gentamicin and cephalosporins. Pseudomembranous enterocolitis Ulcerative gingivitis H. pylori gastritis 19 Tinidazole: 20 It is similar to metronidazole in its mechanism of action and unwanted effects, but is eliminated more slowly, having a halflife of 12-14 hours. Emetine: 21 It is an alkaloid from cephalis ipecacunha. Emetine is a potent and directly acting amoebicide-kills tropozoites but has no effects on cysts. It acts by inhibiting protein synthesis in amoebae by arresting intra-rebosomal translocation of tRNA –amino acid complex. Cont… Toxicity: Pain and tenderness in the area of injection are frequent, and sterile abscesses may develop. Diarrhea is common. Other adverse effects are: Nausea, vomiting, muscle weakness and discomfort, and minor electrocardiographic changes Serious toxicities include: cardiac arrhythmias, heart failure, and hypotension. The drugs should not be used in patients with cardiac or renal disease, in young children, or in pregnancy unless absolutely necessary. 22 Cont… Use: 23 Because of toxicity, emetine is now seldom used as a reserve drug in severe intestinal or extra intestinal amoebiasis. It is also used for patients not responding to or not tolerating metronidazole. Dehydroemetine: 24 Semisynthetic derivative of emetine. Equally effective but less cumulative and less toxic to heart. Thus, it is preferred over emetine. Chloroquine: Chloroquine reaches high liver concentrations → treatment of amoebic liver abscess. Amoebae do not develop resistance to chloroquine. Not effective in the treatment of intestinal or other extrahepatic amoebiasis. 25 DILOXANIDE FUROATE: 26 It is an effective luminal amebicide but is not active against tissue trophozoites. The mechanism of action of diloxanide furoate is unknown. Diloxanide furoate does not produce serious adverse effects. Flatulence is common, but nausea and abdominal cramps are infrequent and rashes are rare. The drug is not recommended in pregnancy. It is the drug of choice for mild intestinal/ asymptomatic amoebiasis. 8-HYDROXYQUINOLINES: 27 They are active against Entamoeba, Giardia, Trichomonas. They kill the cyst forming tropozoites in the intestine, but do not have tissue amoebicidal action. They are not very effective in acute amoebic desentry but afford relief in chronic intestinal amoebiasis. They are totally valueless in extraintestnal Amoebiasis. They are widely used for the prophylaxis and treatment of nonspecific diarrheas, traveler's diarrheas. PAROMOMYCIN SULFATE: 28 Paromomycin sulfate is an amino glycoside antibiotic. Paromomycin is an effective luminal amebic idée that appears to have similar efficacy and probably less toxicity than other agents; in a recent study, it was superior to diloxanide furcated in clearing asymptomatic infections. Paromomycin shares the same mechanism of action as neomycin and kanamycin (binding to the 30S ribosomal subunit) and has the same spectrum of antibacterial activity. Paromomycin has become the drug of choice for treating intestinal colonization with E. histolytic. It is used in combination with metronidazole to treat amebic colitis and amebic liver abscess and can be used as a single agent for asymptomatic individuals found to have E. histolytica intestinal colonization. References: 1. 2. 3. 4. 5. 29 Tripathi K D., Essential of medical pharmacology, 2003; 5: 749-758 Rang H P., Dale M M., Ritter JM., flower RJ., Pharmacology, 2007; 6: 698-711 Brunton L L., Lazo J S., Parker K L., Goodman & Gilman's the pharmacological basis of therapeutics, 2006; 11: 1097-1120 Katzung B G., Basic and clinical pharmacology, 2007; 9: 1207-1237 Seth S D.,Seth Vimlesh.,pharmacology,2009;3:xi.20xi32 Thank you 30