Endo 17 Parathyroid Diseases Anatomy & Embryology 4 parathyroid
advertisement
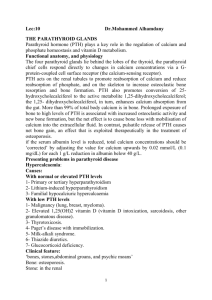
Endo 17 Parathyroid Diseases Anatomy & Embryology 4 parathyroid glands adjacent to the thyroid, Wt. approx 40 mg, very tiny Arise from the 3rd and 4th embryonic branchial pouches; inferior glands arise from the 3rd pouches, superior glands arise from the 4thpouches Sometimes one gland follows the thymus and ends up in the superior mediastinum 12-15% population have a 5th PT gland, makes surgery tricky, surgeon’s experience is important The Chief cell is the predominant epithelial cell. It has a clear cytoplasm The Oxyphil cell is slightly larger and has an eosinophilic granular cytoplasm. Both cells contain PTH and it is not known whether their secretory regulation differs Parathyroid Hormone (PTH) 84-AA peptide with a MWt of 9300, Gene located on Chrom # 11, t1/2 is 2-4 mins Mature or intact PTH(1-84) is cleared by the liver and kidney – it is cleaved into amino and carboxyl terminal fragments thought to have their own receptors and biologic activity Modern iPTH assays: Either a 2-site (NH4- and COO terminal) IRMA (immunoradiometric assay), or 2-site ICMA (immunochemiluminescent assay) Highly specific to the intact PTH, can detect both high and low levels of iPTH (vs older assays) Can easily determine if hypercalcemia is parathyroid driven or not PTH secretion and function: under control by the serum calcium concentration [Ca++]. Has feedback loop system The calcium receptor is a member of the 7-transmembrane-domain, G protein-coupled receptor family, receptors are ubiquitous PTH secretagogues: Primarily serum calcium, Magnesium (less potent), Vitamin D, and Catecholamines PTH 3 target organs: Bone, Intestinal mucosa, Kidney Bones are primary storage for Ca, hold 1 kg of Ca in skeleton, exchange occurs w/ ECM 98% of Ca is reabsorbed by the kidneys Vitamin D is important for Ca absorption PTH increases osteoclastic bone resorption of calcium and phosphate, too much PTH Increases distal convoluted tubular calcium reabsorption and decreases proximal tubular phosphate reabsorption Increases gut absorption of calcium w/ help of Vit D from kidneys Net effect: serum calcium and serum phosphate Renal effects of PTH: Most Calcium absorption occurs in the proximal tubule + bicarbonate and sodium PTH is responsible for fine-tuning of calcium absorption in the distal nephron and inhibits phosphate reabsorption in the proximal tubule. HyperPTH = Bicarbonate reabsorption impaired mild hyperchloremic metabolic acidosis Parathyroid Hormone Abnormalities Increased: Primary, Secondary, or Tertiary Hyperparathyroidism, or Pseudohypoparathyroidism Decreased: Hypoparathyroidism, Hypercalcemia of malignancy/other, Hypomagnesemia Hypercalcemia Causes: Most common in ambulatory pts = hyperPT (70-80%) Hospitalized patients = malignancy (50%) First line test in a hypercalcemic patient should be the PTH level Less common: VITAMINS TRAP: Vit A and D excess, immobilization, thyrotoxicosis, Addison’s disease, Milk-alkali,Multiple Myeloma, Metastatic disease, inflammatory disease, neoplasms, sarcoidosis, thiazides / drugs (lithium,theophylline), rhabdomyolysis, AIDS, Paget’s disease 1° hyper PTH: Common, incidence 1:1000, sporadic or familial, F > M 2-3:1 single parathyroid adenoma (80%), Hyperplasia (15%), Multiple adenomas (5%), parathyroid cancer (rarely) Familial - think MEN (I or IIA) and hyperplasia Clinical features: Mostly asymptomatic, Bones (long bone pain), Stones (kidneys +polyuria, polydipsia), Groans (gastric ulcers), Moans (psychiatric – depression) Labs: [Ca ++] usually mild and present for several years, or Serum phosphate, or iPTH - inappropriately normal (should be ↓), urine [Ca++ ] > 300 mg/24 hrs (if low think other etiologies) X-Rays: Loss of cortical bone (Wrist >> Hip/Spine on DXA bone density scan), Subperiosteal bone resorption (phalanges), “Salt and Pepper” skull, Osteitis fibrosa cystica (fibrous replacement of the resorbed bone = bone pain, tenderness, deformity, fracture), Brown tumors (osteoclasts intermixed with poorly mineralized woven bone), Renal stones/nephrocalcinosis (Ca deposits throughout kidney tissue), 99mTechnetiumSestaMIBI scan used to identify which gland to remove Therapy: Cure is SURGICAL, ALL PT glands should be examined, Resect an isolated adenoma PT hyperplasia requires subtotal parathyroidectomy – leaving about 50 mg of PT tissue either in situ or transplant in forearm Who needs Surgery : Symptomatic hypercalcemia, Serum calcium > 1 mg/dl upper limits of normal, Creatinine clearance <70% or history of stones, Bone Mineral Density T score < -2.5 SD any site(osteoporosis), Age (< 50 years) 4 Gland Exploration vs Minimally Invasive: Localization procedure prior to surgery(sestaMIBI, CT, US, MRI), Intraoperative PTH levels (should drop by 50% w/in 10 min), Post op hypocalcemia – “hungry bones” Surgical Complications: RLN damage with hoarseness, Hypocalcemia – often mild and transient but could be permanent and very severe (will need long term p.o. calcium and Vitamin D3 replacement), “Hungry Bones” syndrome – in pts with severe preexisting parathyroid bone disease the bones mop up calcium as the parathyroid drive ceases – causes acute hypoclacemia x 48 hrs. Medical therapy: for mild/ inoperable cases Avoid Diuretics (cause dehydration ↑ risk of calcification/crystalization),thiazides could raise serumcalcium, Adequate Hydration, possible estrogen for bone protection, Bisphosphonates – decrease bone turnover, Calcimimetics may become useful, Monitor Se [Ca++ ] every 6 mo and Serum Creat and DXA BMD of wrist, hip and spine q year Variants of Hyperparathyroidism: Secondary – vitamin D deficiency, renal failure, Very common Tertiary Hyperparathyroidism: Continuous parathyroid stimulation in secondary hyperparathyroidism as in ESRD(renal failure) leads to autonomous parathyroid glands Familial Hypocalciuric Hypercalcemia (FHH): Inactivating mutation in calcium sensor/receptor (parathyroids & kidneys) Mild hypercalcemia & normal or elevated iPTH, Low 24 hour urinary calcium (FEca < 1%), Asymptomatic - do not require surgery, medications or follow-up. Clinical Case A 45 year old female comes for her annual physical. Labs shows a serum Ca++ of 11.0 mg/dl (NR 8.3-10.5 mg/dl);Albumin 4.0g/dl, Last year’s Ca: 10.6 mg/dl, She is asymptomatic Results: iPTH level is 50 ng/dl (NR 15-65ng/dl), 24h urine calcium is 280 mg/24 h (NR < 300mg/24h) Diagnosis and plan: Surgery because young age (< 50) Hypo PTH: PTH production or Resistance to PTH PTH production: Surgical excision, Infiltrative process (Wilson’s disease, hemochromatosis), Autoimmune destruction (AI polyglandular syndrome type 1), Congenital (DiGeorge syndrome , thymic aplasia, or defective branchial arch formation), Mg++ impairs PTH secretion and action, Familial Symptoms: Depends on the degree and rapidity of onset of hypocalcemia Paresthesiae, carpopedal spasm, tetany, laryngeal stridor, convulsions, apathy, depression, Calcification of basal ganglia on brain CT and benign intracranial hypertension GI – nausea,vomiting, abd pain, malabsorption Prolonged QT interval on ECG Cataracts,alopecia Mucocutaneaous candidiasis in DiGeorge syndrome Clinical Features: mobilization of Ca++ from bone, renal distal tubular calcium reabsorption, renal phosphate excretion , renal production of 1,25 diOHVitD [Ca++] and [Phosphate] PTH or inappropriately Differential diagnosis: Vitamin D resistance, Vit D deficiency (liver,kidney disease, malabsorption, malnutrition), calcium mobilization from bone, osteoblastic metastases (prostate cancer), hungry-bone syndrome post parathyroid surgery, tissue calcium deposition- acute pancreatitis Diagnostic Approach to hypocalcemia: Always remember to correct for serum albumin to confirm true low calcium. Measure iPTH: PTH = hypoparathyroidism, PTH = Vit D deficiency or pseudo hypoPTH, 25 OH Vit D – GI,liver disease or dietary deficiency, 1,25 di OH Vit D – renal disease, Mg++ Corrected Calcium for serum albumin: For an albumin of 4.0… (Nl[Alb] – Pt[Alb]) x 0.8 + [Ca] Treatment of Hypocalcemia: If symptomatic or has complications, IV calcium gluconate or p.o. calcium carbonate – at least 1500 mg daily but depends on severity, Vit D 3 (Calcitriol is best) – once to twice daily, But NOT synthetic PTH (Teriparatide/Forteo) osteoporosis treatment only! PTH Resistance: Pseudo hypoparathyroidism types 1 A and 1 B, end-organ resistance to PTH, Receptor or post-receptor defect , Defect is in the Gs subunit of the receptor Hypocalcemia, hyperphosphatemia, high iPTH Type 1 A (Albright’s Hereditary Osteodystrophy-AHO): Characteristic appearance/phenotype: Short stature, round face, short metacarpals and metatarsals, calcified basal ganglia, mild mental subnormality. Pseudohypoparathyroidism 1B: Same lab findings but not phenotype Pseudo pseudohypoparathyroidism: Same phenotype as pseudohypoPTH 1A (AHO) but no biochemical abnormalities of hypoPTH, remember PTH is in pseudohypoPTH…patient is resistant to PTH not deficient in it. Clinical Case: 22 y male with Graves’ disease not responding to I 131 ablations (x2) or antithyroidal agents. He comes in for a total thyroidectomy. Post-op c/o tingling in hands, feet, lips and cramps in his legs. Stat serum Ca++ 6.1 mg/dl (NR 8.3-10.5 mg/dl) Tx: Give 1 g calcium gluconate i.v. and repeat serum calcium regularly. Check magnesium and replace if low, iPTH assay will take 2-3 days to come back, Start calcium carbonate 1-2 grams po tid , Start Calcitriol (Vit D3) po 0.5 mcg po bid