CASCAP
advertisement

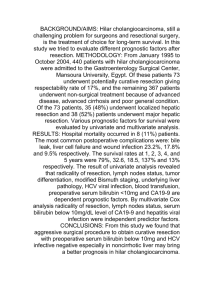
TITLE PAGE Title: Comparison of Characteristic CT findings of Mass-forming Cholangiocarcinoma and Hepatocellular Carcinoma with Pathological Proof in Northeastern Thailand. Authors: Ruangritkul Prapat1 Affiliations: 1 Department of Radiology, Faculty of medicine, Khon Kaen University, Thailand Corresponding authors: Name: Prapat Ruangritkul Address: Department of Radiology, Faculty of medicine, Khon Kaen University, Khon Kaen, 40002, Thailand Telephone:+66-88-5617878 Fax: e-Mail: Type of contribution: Original research results Running title: Number of words in the abstract: 250 Number of words in the text: x,xxx Number of tables: x Number of figures: x ABSTRACT Background: CT scan is the most suitable confirmatory investigation for diagnosis of hepatobiliary disease that recent available in all provinces in the northeast of Thailand. Hepatocellular carcinoma (HCC) is the most common primary liver cancer in the world and Cholangiocarcinoma (CCA) is the highest incidence in northeastern of Thailand. CT findings of mass-forming CCA and HCC are closely similar and each of these diseases needs different treatment. The goal standard for diagnosis of these diseases are pathological confirmation but it is invasive procedure which harmful to patients. Suitable and available investigation to confirm diagnosis before invasive treatment seem to have more benefit. There is no currently study in our knowledge to compare CT findings of these diseases with pathological proof. Objective: To compare CT findings in mass-forming CCA and HCC cases with pathologic proof. Methods: CT database of ??? patients were analyzed retrospectively from Srinagarind hospital, in northeast Thailand during ??? to ??? with pathological proof. Three experienced, abdominal radiologists blinded to clinical histories, pathological findings, separately reviewed CT findings. The overall results are analysed for statistics. Results: The total are ??? patients. Interobserver reliability is ???. The sensitivity was ??? (95%CI: ??.?, ??.?), specificity was ??? (95%CI: ??.?, ??.?), accuracy was ??? (95%CI: ??.?, ??.?), positive predictive value was ??? (95%CI: ??.?, ??.?) and negative predictive value was ??? (95%CI: ??.?, ??.?) for diagnosis of mass-forming CCA, comparing with HCC. Conclusions: The CT finding : ??? is high sensitivity and accuracy to diagnose mass-forming CCA, comparing with HCC. Introduction The diagnosis of cholangiocarcinoma and hepatocellular carcinoma should be considered if the tumor has similar findings to mass-forming cholangiocarcinoma without bile duct dilatation on cirrhotic liver and the patient has normal or low rising of the AFP level with or without elevated CA 19-9 level but in non-cirrhotic liver, the finding is nonspecific.(1) Twenty percent of the cholangiocarcinomas were difficult to distinguish from hepatocellular carcinomas or hemangiomas.(2) Cholangiocarcinoma is a primary liver cancer which highest incidence in northeast of Thailand(3) and hepatocellular carcinoma is the most common primary liver cancer in the world.(4) Cholangiocarcinomas are devided into three types on basis of their morphology; mass forming, periductal and intraductal types. Intrahepatic cholangiocarcinoma (IHCC) has three distinct CT patterns, solitary dominant mass (type I IHCC), dominant mass with satellite nodules in same segment (type II IHCC), and multiple scattered hepatic lesions (type III) with different prognoses and treatments.(5) Preoperative diagnosis of combined hepatocellular cholangiocarcinoma tumors on the basis of imaging features is accurate in the minority of cases. Tumor markers and risk factors may help improve accuracy; however, in the absence of classic imaging features and supportive information for HCC or cholangiocarcinoma, biopsy should be considered for pathological confirmation of diagnosis(6) but it is is invasive procedure which harmful to patients. CT or MR imaging may help differentiate mass-forming cholangiocarcinoma and hepatocellular carcinoma with invasions to biliary tracts.(7, 8) The CT scan is more available than MRI because CT scan is recent available in all provinces in the northeast of Thailand. There is no currently study in our knowledge to compare CT findings of these diseases with pathological proof. This study aims to compare CT findings in mass-forming CCA and HCC cases with pathologic proof. MATERIALS AND METHODS Study design This study had ??? patients with histopathologically confirmed mass-forming cholangiocarcinoma or hepatocellular carcinoma from pathology database at Srinakarind hospital between 2007 – 2014. Patients who did not have database CT at Srinakarind hospital were excluded from this study. The remaining ??? patients were included in our retrospective study. Imaging and image analysis MDCT images were acquired on MDCT (Siemens and Philips) scanners with 5-mm thickness axial images and 4-mm coronal reconstructions. Iopromide (300mgI/ml) was administered as intravenous contrast using and automated injecteor at rate of 2-3 ml/s. Precontrast, arterial and portovenous phases were performed. The images were reviewed separately on PACS by three experienced, abdominal radiologists blinded to clinical histories and pathological findings. Imaging features of the tumor, which were recorded included the largest dimension, presence of satellite lesions, capsular retraction, biliary obstruction, vascular involvement, segmental or lobar atrophy and calcification. Statistical analysis Demographic characteristics of the participants were described using frequency and percentage for categorical data and mean and standard deviation for continuous data. The overall results were analyzed by sensitivity, specificity, accuracy, positive predictive value (PPV) and negative predictive value (NPV). All analyses were performed using Stata version 10.0 (StataCorp, College Station, TX). All test statistics were two-sided and a p-value of less than 0.05 was considered statistical significant. This project was approved by the Human Research and Ethics Committees of the Ministry of Public Health of Thailand. Results Demographic Characteristics The study consisted of ?? men and ?? women with a mean age of ?? years (range ?? ?? years). There were mass-forming cholangiocarcinoma ?? patients and hepatocellular carcinoma ?? patients Table I Demographics and characteristic of patients Mass-forming CCA HCC Characteristics Number Percentage Number Percentage (%) (%) Gender male female Age >50 years <50 years Mean standard deviation Underlying Hepatitis Cirrhosis Fatty liver Laboratory AST ALT ALP AFP CA19-9 30 50 30 50 Table II Detail characteristics in each CT finding for pathologically proven patients CT findings Mass-forming HCC P-value CCA The largest dimension <3 cm 3-5 cm >5 cm Presence of satellite lesions Capsular retraction Biliary obstruction Vascular involvement Calcification Border Well-defined Irregular Attenuation Hypodense Isodense Hyperdense Heterogeneous Enhancement pattern Non-enhancement Enhancement Morphology Atrophic /Hypertrophic complex Table III Diagnostic parameters of each CT findings for mass-forming CCA comparing with HCC CT findings Sensitivity Specificity Accuracy PPV NPV Biliary obstruction Border Well-defined Irregular Enhancement pattern Non-enhancement Enhancement DISCUSSIONS Explaining the findings <copy narrative parts of the Results followed by explaining each important findings in turn , 5-10 references needed here in this section where about half of them are the same as the one cited in the Introduction section of the manuscript> Strength of the study <to be written> Limitation of the study Can selection bias distort the findings? Can information bias distort the findings? Can confounding bias distort the findings? Conclusions The CT finding : ??? is highly sensitivity and accuracy to diagnose mass-forming CCA, comparing with HCC. Recommendations <to be written> Acknowledgements: ******Reference conclusion****** The presence of peripheral bile duct dilatation, extrahepatic spreading, and proximal bile duct enhancement were highly suggestive of peripheral, mass-forming cholangiocarcinoma. (9) ICC in cirrhotic patients displays distinct vascular patterns at CT-scan that allow for differentiation from HCC.(10) In hilar type cholangiocarcinoma, the portal venous phase yielded the best findings. Furthermore, it showed all findings that were seen in the hepatic arterial phase. According to the present study, the authors suggest doing a pre-contrast study then a portal venous phase imaging for evaluation and diagnosis of hilar type cholangiocarcinoma. There is no necessity to perform hepatic arterial phase in hilar cholangiocarcinoma.(11) The sensitivity of computed tomography during arterial portography for diagnosing intrahepatic cholangiocarcinoma and its intrahepatic metastasis was low due to segmental perfusion defect. It is necessary for intrahepatic cholangiocarcinoma to be subjected to systematic segmentectomy including all areas corresponding to the segmental perfusion defect.(12) Combined interpretation of CT and direct cholangiographic images by using our revised criteria resulted in overall accuracy of 74.5% for prediction of resectability for hilar cholangiocarcinoma.(13) The contrast-enhancement pattern of ICC on single-level dynamic CTHA is related to the intratumoral artery.(14) In the proper clinical setting, detection of a hypodense hepatic lesion with peripheral enhancement, biliary dilatation, and contrast enhancement on delayed images are highly suggestive of peripheral intrahepatic cholangiocarcinoma.(15) Segmental or lobar dilatation of the intrahepatic bile ducts associated with or without intraductal polypoid mass, amorphous structures, or both with slight hyperattenuation are common CT findings of intraductal intrahepatic cholangiocarcinoma. The size of the intraductal mass determines the visibility on CT.(16) Both D-CT and D-MRI can provide important information for the diagnosis of PCC. D-CT is better than D-MRI for demonstrating vascular involvement and extrahepatic invasion. D-MRI gives more conspicuous enhancement.(17) The variation over time in the intensity of contrast enhancement in HCC and cholangiocarcinoma differs sufficiently to make this a useful diagnostic criterion. The delayed phase is particularly important because it amplifies this difference.(18) Helical CT aids in tumor localization and in assessment of parenchymal, biliary intrahepatic, and portal involvement in hilar cholangiocarcinoma. However, helical CT is not effective in the assessment of biliary extrahepatic, arterial, and lymph node involvement.(19) Multiphasic helical CT can be used to detect and classify hilar cholangiocarcinomas. However, the exact proximal tumor extent along bile ducts tends to be underestimated with helical CT; therefore, helical CT is inaccurate for determining resectability.(20) CT scanning should be one of the most important investigative methods for IHPCC due to the disease characteristics identified in CT image, especially "encysted sign of dilated bile ducts" which possesses specificity in diagnosing the disease.(21) Delayed tumoral contrast enhancement is a typical feature of intrahepatic cholangiocarcinoma and may aid in the detection and characterization of such lesions at CT.(22) Thin, mild, incomplete rimlike contrast enhancement at the tumor periphery and markedly low intratumoral attenuation with amorphous areas of slightly high attenuation during both scanning phases are typical findings of peripheral cholangiocarcinoma.(23) In the evaluation of hilar or intrahepatic cholangiocarcinoma, delayed CT images are helpful for tumor characterization and may improve observer confidence for the presence of tumor. The optimal time for acquisition of delayed images is 10-20 min after contrast media injection.(24) In the CC type, enhanced CT images were compatible with CC, but positivities for virus markers and serum AFP levels were almost equivalent to those in HCC. Therefore, the CC type can be diagnosed as combined HCC-CC by evaluating virus markers and serum AFP levels with CT. In addition, no association of intrahepatic bile duct dilatation was considered to be a characteristic feature of combined HCC-CC.(25) Dynamic enhancement patterns and signals in T2-weighted images were the most important MR features to differentiate sIMCC from atypical sHCC with cirrhosis and chronic viral hepatitis.(26) Although annual HCC incidence in cirrhotic patients did not differ significantly among different age groups, rates among noncirrhotic patients were significantly higher in older patients and up to 1.1% in males above 55 years.(27) The rate increase in the first 5 to 6 years may be due to improved completeness of the registry, since in the subsequent 10 to 12 years there is a rather stable rate. It may be, however, that the recent decline in incidence represents a real fall in risk.(28) Developing a consistent and uniform topographical classification for acceptable coding practice to all health professionals is necessary. In addition, epidemiological research on risk factors according to anatomical location (intrahepatic versus extrahepatic) and the macroscopic appearance and/or new histological classification of cholangiocarcinoma is also needed.(29) the rates of HCC and ICC approximately doubled between 1976 and 2000. Trends by age, gender, ethnicity, and birth cohort suggest that heterogeneity exists in the factors influencing these rates.(30) 1. Phongkitkarun S, Srisuwan T, Sornmayura P, Jatchavala J. Combined hepatocellular and cholangiocarcinoma: CT findings with emphasis on multiphasic helical CT. Journal of the Medical Association of Thailand = Chotmaihet thangphaet. 2007 Jan;90(1):113-20. PubMed PMID: 17621741. 2. Honda H, Onitsuka H, Yasumori K, Hayashi T, Ochiai K, Gibo M, et al. Intrahepatic peripheral cholangiocarcinoma: two-phased dynamic incremental CT and pathologic correlation. Journal of computer assisted tomography. 1993 May-Jun;17(3):397-402. PubMed PMID: 8388005. 3. Vatanasapt V, Uttaravichien T, Mairiang EO, Pairojkul C, Chartbanchachai W, Haswell-Elkins M. Cholangiocarcinoma in north-east Thailand. Lancet. 1990 Jan 13;335(8681):116-7. PubMed PMID: 1967406. 4. Poustchi H, Sepanlou S, Esmaili S, Mehrabi N, Ansarymoghadam A. Hepatocellular carcinoma in the world and the middle East. Middle East journal of digestive diseases. 2010 Jan;2(1):31-41. PubMed PMID: 25197510. Pubmed Central PMCID: 4154905. 5. Baheti AD, Tirumani SH, Shinagare AB, Rosenthal MH, Hornick JL, Ramaiya NH, et al. Correlation of CT patterns of primary intrahepatic cholangiocarcinoma at the time of presentation with the metastatic spread and clinical outcomes: retrospective study of 92 patients. Abdominal imaging. 2014 Dec;39(6):1193-201. PubMed PMID: 24869789. 6. Fowler KJ, Sheybani A, Parker RA, 3rd, Doherty S, E MB, Chapman WC, et al. Combined hepatocellular and cholangiocarcinoma (biphenotypic) tumors: imaging features and diagnostic accuracy of contrast-enhanced CT and MRI. AJR American journal of roentgenology. 2013 Aug;201(2):332-9. PubMed PMID: 23883213. 7. Yang NJ, Song B, Wu B, Xu J, Zhao LM. [CT and MR imaging differences between intrahepatic cholangiocarcinoma and hepatocellular carcinoma with invasions to billary tracts]. Sichuan da xue xue bao Yi xue ban = Journal of Sichuan University Medical science edition. 2009 May;40(3):525-8. PubMed PMID: 19627020. 8. Park HS, Lee JM, Kim SH, Jeong JY, Kim YJ, Lee KH, et al. CT Differentiation of cholangiocarcinoma from periductal fibrosis in patients with hepatolithiasis. AJR American journal of roentgenology. 2006 Aug;187(2):445-53. PubMed PMID: 16861550. 9. Apisarnthanarak P, Pansri C, Maungsomboon K, Thamtorawat S. The CT appearances for differentiating of peripheral, mass-forming cholangiocarcinoma and liver meatastases from colorectal adenocarcinoma. Journal of the Medical Association of Thailand = Chotmaihet thangphaet. 2014 Apr;97(4):415-22. PubMed PMID: 24964684. 10. Iavarone M, Piscaglia F, Vavassori S, Galassi M, Sangiovanni A, Venerandi L, et al. Contrast enhanced CT-scan to diagnose intrahepatic cholangiocarcinoma in patients with cirrhosis. Journal of hepatology. 2013 Jun;58(6):1188-93. PubMed PMID: 23485522. 11. Aphinives C, Tumsatan P, Srinakarin J, Laopaiboon V, Aphinives P. Helical CT assessment on hilar cholangiocarcinoma: comparison value of arterial phase and portovenous phase correlation. Journal of the Medical Association of Thailand = Chotmaihet thangphaet. 2007 Nov;90(11):2403-8. PubMed PMID: 18181327. 12. Miura F, Okazumi S, Takayama W, Asano T, Makino H, Shuto K, et al. Evaluation of CT during arterial portography for preoperative diagnosis of intrahepatic cholangiocarcinoma. Hepato-gastroenterology. 2006 May-Jun;53(69):435-7. PubMed PMID: 16795987. 13. Lee HY, Kim SH, Lee JM, Kim SW, Jang JY, Han JK, et al. Preoperative assessment of resectability of hepatic hilar cholangiocarcinoma: combined CT and cholangiography with revised criteria. Radiology. 2006 Apr;239(1):113-21. PubMed PMID: 16467211. 14. Miura F, Okazumi S, Takayama W, Asano T, Makino H, Shuto K, et al. Hemodynamics of intrahepatic cholangiocarcinoma: evaluation with single-level dynamic CT during hepatic arteriography. Abdominal imaging. 2004 Jul-Aug;29(4):467-71. PubMed PMID: 15136895. 15. Valls C, Guma A, Puig I, Sanchez A, Andia E, Serrano T, et al. Intrahepatic peripheral cholangiocarcinoma: CT evaluation. Abdominal imaging. 2000 SepOct;25(5):490-6. PubMed PMID: 10931983. 16. Lee JW, Han JK, Kim TK, Kim YH, Choi BI, Han MC, et al. CT features of intraductal intrahepatic cholangiocarcinoma. AJR American journal of roentgenology. 2000 Sep;175(3):721-5. PubMed PMID: 10954456. 17. Zhang Y, Uchida M, Abe T, Nishimura H, Hayabuchi N, Nakashima Y. Intrahepatic peripheral cholangiocarcinoma: comparison of dynamic CT and dynamic MRI. Journal of computer assisted tomography. 1999 Sep-Oct;23(5):670-7. PubMed PMID: 10524843. 18. Loyer EM, Chin H, DuBrow RA, David CL, Eftekhari F, Charnsangavej C. Hepatocellular carcinoma and intrahepatic peripheral cholangiocarcinoma: enhancement patterns with quadruple phase helical CT--a comparative study. Radiology. 1999 Sep;212(3):866-75. PubMed PMID: 10478259. 19. Feydy A, Vilgrain V, Denys A, Sibert A, Belghiti J, Vullierme MP, et al. Helical CT assessment in hilar cholangiocarcinoma: correlation with surgical and pathologic findings. AJR American journal of roentgenology. 1999 Jan;172(1):73-7. PubMed PMID: 9888743. 20. Tillich M, Mischinger HJ, Preisegger KH, Rabl H, Szolar DH. Multiphasic helical CT in diagnosis and staging of hilar cholangiocarcinoma. AJR American journal of roentgenology. 1998 Sep;171(3):651-8. PubMed PMID: 9725291. 21. Chen H, Hui Y. Intrahepatic peripheral cholangiocarcinoma: CT features in 18 pathologically proven cases. Chinese medical journal. 1998 May;111(5):453-6. PubMed PMID: 10374358. 22. Lacomis JM, Baron RL, Oliver JH, 3rd, Nalesnik MA, Federle MP. Cholangiocarcinoma: delayed CT contrast enhancement patterns. Radiology. 1997 Apr;203(1):98-104. PubMed PMID: 9122423. 23. Kim TK, Choi BI, Han JK, Jang HJ, Cho SG, Han MC. Peripheral cholangiocarcinoma of the liver: two-phase spiral CT findings. Radiology. 1997 Aug;204(2):539-43. PubMed PMID: 9240550. 24. Keogan MT, Seabourn JT, Paulson EK, McDermott VG, Delong DM, Nelson RC. Contrast-enhanced CT of intrahepatic and hilar cholangiocarcinoma: delay time for optimal imaging. AJR American journal of roentgenology. 1997 Dec;169(6):1493-9. PubMed PMID: 9393152. 25. Fukukura Y, Taguchi J, Nakashima O, Wada Y, Kojiro M. Combined hepatocellular and cholangiocarcinoma: correlation between CT findings and clinicopathological features. Journal of computer assisted tomography. 1997 Jan-Feb;21(1):52-8. PubMed PMID: 9022770. 26. Sheng RF, Zeng MS, Rao SX, Ji Y, Chen LL. MRI of small intrahepatic massforming cholangiocarcinoma and atypical small hepatocellular carcinoma (</=3 cm) with cirrhosis and chronic viral hepatitis: a comparative study. Clinical imaging. 2014 MayJun;38(3):265-72. PubMed PMID: 24559750. 27. Do AL, Wong CR, Nguyen LH, Nguyen VG, Trinh H, Nguyen MH. Hepatocellular carcinoma incidence in noncirrhotic patients with chronic hepatitis B and patients with cirrhosis of all etiologies. Journal of clinical gastroenterology. 2014 Aug;48(7):644-9. PubMed PMID: 24201999. 28. Kamsa-ard S, Wiangnon S, Suwanrungruang K, Promthet S, Khuntikeo N, Kamsa-ard S, et al. Trends in liver cancer incidence between 1985 and 2009, Khon Kaen, Thailand: cholangiocarcinoma. Asian Pacific journal of cancer prevention : APJCP. 2011;12(9):220913. PubMed PMID: 22296358. 29. Shin HR, Oh JK, Masuyer E, Curado MP, Bouvard V, Fang Y, et al. Comparison of incidence of intrahepatic and extrahepatic cholangiocarcinoma--focus on East and SouthEastern Asia. Asian Pacific journal of cancer prevention : APJCP. 2010;11(5):1159-66. PubMed PMID: 21198257. 30. McGlynn KA, Tarone RE, El-Serag HB. A comparison of trends in the incidence of hepatocellular carcinoma and intrahepatic cholangiocarcinoma in the United States. Cancer epidemiology, biomarkers & prevention : a publication of the American Association for Cancer Research, cosponsored by the American Society of Preventive Oncology. 2006 Jun;15(6):1198-203. PubMed PMID: 16775181.