Mega Immunology Block 4
advertisement
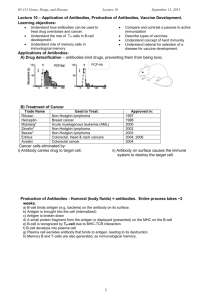
AUTOIMMUNITY Q: In general, what causes autoimmunity? A: Autoimmunity is due to a loss of tolerance, either from hormones, stress, or infection. It can be a loss of central tolerance or peripheral tolerance. Q: What is tolerance? A: Tolerance means in the presence of an antigen, the lymphocyte is unresponsive or goes through apoptosis. Q: What’s the difference between central and peripheral tolerance? A: Central tolerance happens in the primary lymph organs where the self-recognizing lymphocytes are eliminated. Peripheral tolerance happens in the secondary lymph organs where deletion or anergy of lymphocytes happen after meet self antigen. Q: What is the effect of T cells that bind APC via MHCII-TCR only (without co-stimulators)? A: T cells that do not bind with co-stimulatory molecules onto APC, will become anergic. Q: what is the effect on the T cell with TCR-MHCII and costimulatory binding? Just costimulatory binding? A: MHCII-TCR and Costimulatory signalling will acftivate T cell. Just costimulators binding will have no effect on T cell. Q: What is the requirement for Tregs to suppress autoreactivre CD4 T cells? A: In order for Tregs to suppress autoreactive T cells, they must interact on the same APC. Q: What are the genes of Tregs? A: Cd4+CD25+Foxp3+ Q: Tregs release a lot of different cytokins. What do they do? A: IL-10 inhibits APC functions. TGFbeta inhibits T proliferation. And they both inhibit macrophage activation. This all leads to the lack of a normal lymphocyte response (proliferation, activating macrophage). Q: What disease is caused by a mutation in the Foxp3 gene? A: IPEX Syndrome: Immune rysregulation, Polyendocrinophaty, Enteropathy, X-linked Q: What is Foxp3? A: a transcriptional regulator Q: What syndrome is caused by mutation in AIRE gene? A: APECED Syndrome: Autoimmune Polyendocrinopathy, Candidiasis, Ectodermal Dystrophy. It causes T autoreactive T cells to escape from thymus Q; What happens to your nails during APECED? A: They rot. Q: What matters in susceptibility to autoimmunity? A: gender (like females) and genes (like increased risk in monozygotic twins) Q: Who are most susceptible to Type 1 Diabetes? A: People who are heterozygous for DQ2 and DQ8, and who are different subtypes of DRB1. Q: Can injury cause a fever? A: Yes. IL-1 released from your damaged tissue can cause a fever. Q: What’s an example of trauma-induced autoimmunity? A: Sympathetic Ophthalmia. When one eye gets damaged, intraocular protein antigens are released and go to lymph nodees. T cells activate, travel through blood and attack antigen in both eyes. Q: How does streptococcus cause rheumatic fever? A: Streptococcal cell walls stimulate your immune system to make antibodies. When antibodies crossreact with heart tissue, it causes rheumatic fever. Q: How does self-peptide mimics cause autoimmunity? A: Self-peptide that mimics a pathogen peptide on an MHC is also another cause of autoimmunity. Q: How does abnormal expression of HLA molecules cause autoimmunity? A: Expression of HLA molecules on cells that don’t normally express them, like MHC II on non-APC self cells. T cells then attack these cells, causing autoimmunity. Q: What is a way to classify autoimmune diseases? A: Autoimmune diseases are either organ-specific or systemic. Q: What are autoantigens? A: Antgens that are from the self that shouldn’t normally be antigenic. Q: What happens with autoimmune hemolytic anemia? A: bacteria or virus immitates RBC antigen, and causes immune system to make anti-RBC antibodies. RBC/antibody complex gets phagocytosed in spleen. Q: What happens with pernicious anemia? A: your body produces auto-antibodies to intrinsic factor. B12 can’t be uptaken. You can’t make RBC so you get anemia. Treat by taking B12 supplements. Q: What happens with drug-induced hemolytic anemia? A: drugs like penicillin bind to RBC, modifying it. This causes antibodies to be made (because RBC now looks “foreign”). RBCs lysed and you get anemia. Q: What happens in Goodpasture’s Syndrome? A: Anti-3 chain of TypeIV collagen IgG in kidney or lung complement damage or neutrophils come in respiratory or renal failure. Treat with immunosuppressive drugs or plasmapheresis. Q: Goodpasture syndrome affects which sex the most? A: Mostly males affected by goodpasture syndrome for unknown reasons. Q: What happens during Grave’s Disease (hyperthyroidism)? A: Anti-TSH-R antibodies stimulate thyroid hormone production, resulting in high T3 and T4. Q: What are some symptoms due to the Anti-TSH-R antibodies in Graves’ Disease? A: heat intolerance, irritability, nervousness, weight loss, goiter. Q: What are some symptoms due to the anti-eye muscle antibodies in Graves’ Disease? A: bulging eyes. Q: What are some short-term and long-term treatments of Graves’ Disease? A: Short-term: drugs that inhibit thyroid function. Long-term: thyroid removal, then take synthetic thyroid hormone daily. Q: What’s the clinical name for “bulgy eyes”? A: exophthalmos Q: What do you need thyroglobulin for? A: to make T3 and T4. Q: What happens with Hashimoto’s Thyroiditis? A: When immune system (CD8 with lots of HLA DR5) damages thyroid cells, causing the release of autoantigens and the subsequent reaction of autoantibodies to attack thyroid peroxidase (TPO), thyroglobulin (Tg). Q: What happens when a pregnant woman with Grave’s disease have a baby? A: the anti-TSH-R antibodies cross the placenta and the fetus suffers from Grave’s as well. To cure, do plasmapheresis on the baby. Q: What is the autoantigen that causes multiple sclerosis? A: Myelin Basic protein (MBP) and Myelin Oligodendrocyte Glycoprotein (MOG) Q: What is distroyed in multiple sclerosis? A: myelin sheath. This disrupts neural transmissions. Q: What does the autoantibody attack or block in Myashthenia Gravis? A: alpha subunit of nicotinic acetylcholine receptor of neuromuscular junctions in skeletal muscle. This causes the receptors to be internalized and degraded. This causes muscles to lose sensitivity to neuronal stimulation. Q: What are some symptoms of myasthenia gravis? A: muscle weakening, ptosis, double vision, impaired breathing. Q: How do you treat myasthenia gravis? A: via cholinesterase inhibitor.. Which blocks acetylcholine degradation. Or, immunosuppressive drugs. Q: What is the autoantigen of Insulin-Dependent Diabetes Mellitus (“Diabetes Type I”)? A: GAD 65 (glutamate decarboxylase 65). Beta-cell-specific CTL activate and Th1 cells make IFNgamma. Q: How does a Cox-Sackie virus cause Diabetes Mellitus Type I? A: Cox-Sackie Virus does molecular mimicry of GAD, causing the body to do anti-GAD immune response. This causes the real GAD in the body to be destroyed by Th1, macrophages, and CTL, destroying the islets of Langerhans. Q: What cells get destroyed in Type I Diabetes? A: beta cells of Islets of Langerhans. Q: What happens in Crohn’s Disease? A: Too much Th17, causing lesions in any part of the GI tract. The hypersensitivity that is caused is Type IV, granulomatous reactions. Q: What mutated gene may be the cause of Crohn’s Disease? A: NOD2 Q: What is Ulcerative Colitis? A: Like Crohn’s Disease it is an inflammatory disease of the bowel, but it is only restricted to the rectum/colon region of the GI tract. It is also type II hypersensitivity. Q: What is Celiac Disease? A: Abnormal metabolism of gluten to become gliadin. Gliadin binds to HLA DQ2, which stimulates type IV reaction. Damages Jejunal villi. Q: What is the initiating antigen of Pemphigus Vulagaris? A: Desmoglein 1 and 3 (the adhesion part of desmosomes). Q: What are the two extracellular proteases that attack the desmogleins? A: IgG1 and IgG4. they break down cell junctions (desmosomes), causing blisters in the skin (acantholysis). Q: What population has a high frequency of Pemphigus Vulgaris? A: Ashkenazi Jewish populations Q: What is a rheumatic disease? A: A disease that affects joints and connective tissue. Q: What does SLE stand for? A: Systemic Lupus Erythematosus. The symptoms are varied, and causes are many. Q: What populations have a higher incidence of lupus? A: women, african, asian. Q: How do you diagnose SLE? A: detect anti-double stranded DNA, anti-SnRNP, or smith antigen. You can also find deposition of immune complexes in glomeruli of kidney. ANA is used as a screening test only, because very sensitive but not very specific. Q: What is a physical sign of SLE? A: Butterfly or Malar rash (on cheek). This happens when immune complexes are deposited at epidermal-dermal interface, causing the rashes. It is also lodged in the arteries. Q: How does SLE cause arthritis? A: When immune complexes lodge in joints. Q: What is the rheumatoid factor (autoantibody) responsible for rheumatoid arthritis? A: Anti-IgG Fc IgM antibody. They form immune complexes with the autoantigens (IgG Fc) and get lodged in joints to cause chronic inflammation. Q: What causes the inflammation of joints in rheumatoid arthritis? A: prostaglandins and leukotrienes. Th1 cells also activate macrophages, causing inflammation. Q: How do you treat rheumatoid arthritis? A: anti-TNF alpha (produced by macrophages for inflammation) Q: Where are the autoantigens in Sjogren’s Syndrome? A: in lacrimal and salivary glands. Q: What are the symptoms of Sjogren’s Syndrome? A: chronic inflammation causes decrease in tears and saliva… so dry nose, mouth, eye, and vagina. Q: What is a common physical sign of Sjogren’s Syndrome? A: enlarged parotid gland. Q: What is the autoantigen causing Wegener’s Granulomatosis? Autoantibody? A: Proteinase 3 (PR3) (found in PMN neutrophils) is the autoantigen. Anti-Neutrophil Cytoplasmic Antibody (c-ANCA) is the autoantibody. Q: What is the autoantigen causing Wegener’s Granulomatosis? Autoantibody? A: Proteinase 3 (PR3) is the autoantigen. Anti-Neutrophil Cytoplasmic Antibody (c-ANCA) is the autoantibody. Q: What causes Wegener’s Granulomatosis? A: PMN neutrophils adhere normally to endothelial cells due to inflammatory cytokines. C-ANCA causes neutrophil to degranulate (releasing PR3), causing cell lysis and necrotizing vasculitis. Q: What are some symptoms of Wegener’s Granulomatosis? A: upper respiratory tract granulomas. Cavitation and lesions. Necrotizing glomerulonephritis. Saddlenose deformity. Q: What are three wyas in which Ankylosing Spondylitis can be pathogenic? A: If HLA-B27 share a common peptide similarity with a microbe, T cells and antibodies can attack it, causing cell damage. This mimicry can also cause tolerance to bacterial antigen. HLA-B27 can be presented by MHC II to CD4 T cells, causing CD8 T cell to kill the APCs, causing arthritis. Q: What are the two types of Scleroderma? A: Diffuse Cutaneous (spreads fast and affects inner organs as well), Limited Cutaneous (limited to hands, arms, and face, accompanied by pulmonary hypertension.) Q: What causes Scleroderma? A: When CD4 T cells accumulate in the skin, releasing cytokines that recruit and activate inflammatory cells like mast cells and macrophages. Eventually this will cause fibroblasts to form collagen and fibronectin thickening of skin. Q: When would you ever use plasmapheresis to treat autoimmune diseases? A: if the disease is caused by circulating antibodies or immune complexes, like type II or III mediated diseases. Q: How can monoclonal antibodies be used to treat autoimmune diseases? A: let it target cytokines or other inflammatory molecules. VACCINES Q: What are the four types of vaccines? A: Active Natural, Active Artificial, Passive Natural, Passive Artificial Q: Transplacental maternal antibodies to fetus is an example of what type of vaccine? A: Passive natural Q: Why do neonates have very few infections in first few months? A: Because they get maternal IgG across the placenta. Q: What are some risks of passive immunity? A: Allergic Reaction, Serum Sickness (immune response against foreign antibodies), blood borne pathogens, immunosuppression. Q: What kind of vaccine is RhoGam? A: Artificial passive immunization (which prevents natural passive immunization, ironically). IgG anti-Rh. Q: What are some methods of active immunity? A: Blocking of adhereence, Neutralization, Opsonization, Th1, memory. Q: What is a toxoid? A: A modified bacterial toxin that is altered to be non-toxic that is used as a vaccine. Q: What is the most common vaccine-preventable disease today? A: Pertussis. Q: When would you use inactivated vacacines? A: When the microbes are oncogenic or cannot be attenuated. Q: What are the disadvantages of inactivated vaccines compared with live vaccines? A: not as effect, not lifelong, larger doses needed, immune response mostly humoral, titer diminish with time so boosters needed, anaphylaxis. Q: How do you inactivate a pathogen to make an inactivated vaccine? A: kill using heat or formalin. Q: What must the live attenuated vaccine do to be effective? A: It must replicate. Q: What are live attenuated vaccines? A: They are usually genetic mutants (weaker), or related species (like cowpox and smallpox) Q: Can temperature-sensitive attenuated vaccines be transmitted? A: Yes. It can replicate at cooler upper respiratory tract, but not at normal body temperature. So it can still cause sniffles and be transmitted but it will protect and not cause influenza. Q: What are the advantages of live attenuated vaccines? A: Immune response is more similar to natural infection, low dose is all it takes, both cellular and humoral response. Q: What are the disadvantages of live attenuated vaccines? A: you can get bad side effects, especially to immunosuppressed or pregnant patients. They must be stored and handled carefully, and there is also the rare possibility that they will revert back to virulent form. Q: What are some examples of live attenuated vaccines that I know? A: MMR, Varicella/zoster, Rotav Q: What kind of response is live attenuated vaccines good at inducing? A: CTL Q: What is the difference between Rotarix and RotaTeq? A: Rotarix is made from human rotaviruses. RotaTeq is made from bovine rotaviruses but engineered to express human VP4 and VP7 Q: What is a subunit vaccine? A: vaccines made from the subunit of the pathogen, like surface structures, internal macromolecules, or flagella Q: What are the disadvantages of subunit vaccines? A: lack lifelong immunity so you need boosters. Q: When would you make a subunit vaccine? A: When the microbe cannot be attenuated, or when infection by microbe does not lead to disease. Q: Pure polysaccharide vaccines are not as effective as those made of proteins. How do you improve the immunogenicity? A: by conjugation to an immunogenic protein. Q: What is the problem about pure polysaccharide vaccines/ A: It is not consistently immunogenic in children younger than 2 years old. Q: Name some vaccine adjuvants. A: Alum, CpG, MF59 Q: What is a new delivery method? A: via Virosome – reconstituted flu virus envelope (spherical, unilamellar lipid bilayer) to deliver drug, DNA, or protein IMMUNODEFICIENCY Q: What are the two big types of causes for immunodeficiency? A: Primary B cell deficiency and primary T cell deficiency. Q: What are the four Primary B cell deficiencies? A: X-linked agammaglobulinemia (XLA), Selective IgA deficiency, Common variable immunodeficiency (CVID), Immunoglobulin subclass deficiencies. Q: What is an example of Primary T cell deficiency? A: X-linked hyper-IgM syndrome Q: People with B-cell deficiencies often present what symptoms? A: recurrent sinopulmonary infections, infection with extracellular pyogenic bacteria Q: What happens in X-linked agammaglobulinemia? A: can’t make antibodies, no tonsils, get pneumonia by 2-3 years old, upper respiratory tract infection that doesn’t resolve. Q: What happens in X-linked agammaglobulinemia? A: can’t make antibodies (so IgM not detectable, although IgA and IgG may be because IgA transmitted from breast milk and IgG through placenta), no tonsils, may be normal first 6-8 months of age because get antibodies from mother, get pneumonia by 2-3 years old, upper respiratory tract infection that doesn’t resolve. Q: What is the defect in XLA? A: Defect in B-cell maturation. Q: Can XLA patients receive live vaccines? A: NOOO!!! Because they don’t have B cells to “fight off” the live vaccines. T cell levels are normal though. Q: What is IG (gamma globulin)? A: It is NOT Ig!! It is all the immunoglobulins (IgA, IgB, IgG) Q: What is the genetic cause of XLA? A: btk gene (Bruton’s Tyrosine Kinase), used in B cell maturation in bone marrow. Q: What happens in Selective IgA Deficiency? A: absence of IgA (both serum and secretory). B cells don’t mature into IgA-producing plasma cells. Q: What is the epidemiology of Selective IgA Deficiency? A: It’s the most common primary immunodeficiency disease. Q: Can you treat people with Selective IgA with blood containing IgA? A: NO! Because their bodies will see IgA as foreign objects and cause anaphylactic reactions. In particular, they have IgE anti-IgA antibodies. Q: What’s up with Common Variable Immunodeficiency (CVID)? A: very common and variable disease. Patient has low levels of serum immunoglobulin. Cause is unknown. Q: What are the symptoms of CVID? A: chronic or recurrent bacterial infections of ears, sinuses, bronchi, lungs, etc. Q: How do you treat CVID? A: with Intravenous IG (so all of the immunoglobulins) Q: How do the B Cells and T Cells appear in CVID? A: normal. The defect is in the differentiation of the B-cells!! Q: CVID is associated with what diseases? A: chronic lung disease, autoimmune diseases Q: What happens in Selective IgG Subclass Deficiency? A: Deficiency in one or two IgG subclasses, like IgG2 deficiency in children or IgG3 deficiency in adults. Q: Why are T-cell deficiencies never purely T-cell problems? A: Because T cells are necessary for optimal CD8 and B-cell function. Q: What is X-linked Hyper-IgM? A: defect in CD40L on T Lymphocyte. T cells can’t help B cells class switch IgM to IgG or IgA. So you got lots of IgM but very little IgG or IgA. Q: How do you treat XHIGM? A: With IGIV every 3-4 weeks. Q: What happens in DiGeorge Syndrome? A: No Thymus due to de novo 22q11 Q: What happens in Bare Lymphocyte Syndrome Type I? II? A: Type I: mutation in TAP1 or TAP2 genes that lead to defect in MHC Class I expression low CD8 T Cells Type II: mutation in CIITA or RFX genes that lead to defect in MHC Class II expression low CD4 T cells. Q: What types of deficiencies can cause SCID where both T and B are missing? A: 1. ADA (Adenosine Deaminase) deficiency 2. PNP (purine nucleoside phosphorylase) deficiency 3. Artemis or RAG1 and RAG2 deficiency Q: What types of deficiencies can cause SCID where ONLY T cells are missing? A: 1. Gamma common chain deficiency 2. Jak3 deficiency 3. CD45 (LCA) deficiency 4. IL-7R deficiency 5. CD3 or deficiency Q: Which deficiency of SCID is X-linked? A: gamma common chain. Q: RAG1, RAG2 (on Chrom 11p) or Artemis (on Chrom 10p) deficiency causes what syndrome? A: Omenn Syndrome (It is basically SCID with hypereosinophilia). Q: What does Artemis do? A: It is a DNA cross-linking repair Q: How does ADA deficiency cause SCID? A: Because ADA is used to break down adenosine into inositol. If can’t do this, adenosine and dATP accumulates, toxic. Q: How does PNP deficiency cause SCID? A: Because PNP is used to convert deoxyguanosine into guanine. If can’t do this, you shunt to make dGTP, which is toxic to T and B cells when accumulated. Q: What is the most common form of SCID? A: X-linked SCID – the one defective in gamma common chain of IL-2 receptor. Q: Deficiency in what causes SCID similar to X-SCID. Why? A: Deficiency in Jak3. This is because Jak3 is the main signal tranducer for the common gamma chain of IL2. Q: What is the Classic Triad in Wiskott-Aldrich Syndrome (WAS)? A: thrombocytopenia, severe eczema, recurrent pyogenic infections (bloody diarrhea). Q: What is the mode of inheritance for WAS? A: It is X-linked. Q: What immunoglobin is low in WAS patients? What is high? A: IgM is low. IgA and E are higher than normal Q: WAS patients are defective in response to what type of antigen? A: Polysaccharide antigens. Q: How does WAS affect T cell count? A: CD3+ cells decrease over time, and there is low isotype switching, and poor T-dependent responses in general. Q: What does the WAS protein (WASP) do? A: facilitates actin polymerization, and remember T cells proliferate (MTOC uses actin) upon contact with cytokines, APCs, etc. Q: What kind of kinase is WAS? A: TEC Kinase Q: What kind of immunoglobin deficiency is very common among those with Ataxia-Telangiectasia? A: IgA deficiency Q: What is Ataxia? What is Telangiectasia? A: Ataxia is poor motor coordination. Telangiectasia is dilated small vessels (like in eyes). These are the key symptoms of this genetic disease. You also get immunocompromised, so lots of neoplasia and recurrent infections. EXTREMELY SENSITIVE TO RADIATION. Q: What is the mode of genetic inheritance for Ataxia-Telangiectasia? A: Autosomal Recessive. Gene at 11q22. Q: Which Classical Pathway components can be deficient in Complement Deficiency? What do they lead to? A: C1,2,4 they all lead to immune-complex disease (Type III hypersensitivity) Q: Which Lectin Pathway components can be deficient in Complement Deficiency? A: MBL, MASP1 and 2, C2, C4 Q: Which Alternative Pathway components can be deficient in Complement Deficiency? A: Factor D, Factor P (“Properdin”) they do not lead to immune-complex disease, but they become susceptible to capsulated bacteria and Neisseria. Q: What is Hereditary Angioedema (HAE)? A: Deficiency in C1 inhibitor (a complement regulatory protein) inflammation not inhibited edema Q: What’s the difference between HAE Type I and Type II? A: Type I has lower serum levels of C1 inhibitor. Type II has normal levels, but non-functional mutant protein. Q: What happens when you have Factor H Deficiency? A: Factor H regulates alternative pathway, so deficiency leads to continuous activation of alternative pathway. Continuous deposition of C3 results in dense deposits, thickening of basement membrane glomerulonephritis. Q: What causes Paroxysmal Nocturnal Hemoglobulinuria? A: Deficiency in CD55 (aka Decay Accelerating Factor) and CD59 (aka Homologous Restriction Factor) (caused by PIGA defect, which prevents DAF and HRF from binding to cell membrane to do its job, which is to break down complement on host cell) unrestricted complement excessive lysis of RBC hemoglobulinuria (blood in pee) Q: What are three phagocyte deficiencies? A: LAD, CGD, and CHS Q: hat happens in Leukocyte Adhesion Deficiency (LAD)? A: Deficient in CD18 (used in leukocyte adhesion) no LFA-1 lymphocytes can’t do tethering or diapedesis across endothelium recurrent infections, extreme leukocytosis (white blood count). Q: How do you treat LAD? A: Bone Marrow Transplant (BMT). Q: What causes Chronic Granulomatous Disease (CGD)? A: mutated gp91 (NADPH Oxidase Complex, which does “respiratory burst”) no respiratory burst phagocytes ingest microbes, but can’t kill them granulomas that are chronic. Q: How do you test for CGD? A: Nitro Blue Tetrazolium (NBT) test – test neutrophils to see if they can phagocytose and reduce NBT (which become dark-blue crystals). Q: What causes Chediak-Higashi Syndrome (CHS)? A: mutation in LYST (lysosomal trafficking regulator) gene Vesicles can’t walk on microtubules to get to lysosomes properly Delayed fusion of phagosome with lysosome in leukocytes form granules in cells, impaired chemotaxis, abnormal NK cell activity recurrent bacterial infections. Q: What are secondary immunodeficiencies? A: Immunodeficiencies that were acquired, either by diseases like HIV, malnutrition, drugs, or aging. Q: What are two B-cell malignancies? A: Multiple Myeloma and Waldenstrom’s Macroglobulinemia Q: What is multiple myeloma? A: a type of “Cancer of plasma cells” Q: What cytokine lets myeloma cells thrive? A: IL-6 Q: What causes the bone destruction in multiple myeloma? A: MIP-1α and RANKL , which activate osteoclasts Q: Patients with multiple myeloma are susceptible to what? A: encapsulated bacteria (i.e. pneumococcus), like agammaglobulinemia patients. Q: What are Bence Jones proteins? A: excessive light chains of immunoglobulins produced by the cancerous plasma cells, that get lodged in tissues throughout body to form amyloids. This leads to renal failture and other problems. Q: What are M proteins (or paraproteins)? A: M for monoclonal or myeloma!! M proteins are immunoglobulins produced by monoclonal (myeloma) plasma cells. The light chain of it is called Bence Jones protein, and is found in the urine of patients with multiple myeloma. Q: What kind of paraprotein do most multiple myeloma produce? A: IgG paraprotein Q: How deaths due to multiple myeloma occur? A: renal failure – Bence Jones proteins are toxic to renal tubular epithelial cells and form “casts” that obstruct the tubules. Q: What physical symptoms do you have with multiple myeloma patients? A: lower back pain, “punched out” lesions in skull Q: Waldenstrom’s Macroglobulinemia, like multiple myeloma, is a “B-cell cancer.” But in this case, what is the main paraprotein? A: IgM aka “macroglobulin” Q: What symptoms differs Waldenstrom’s from Multiple Myeloma? A: no lytic bone disease, no renal failure. Q: What is MGUS? A: Monoclonal Gammopathy of Undetermined Significance. Basically if you detect a lot of immunoglobulins in your blood and don’t know the cause. Q: What happens to serum when you have Waldenstrom’s Macroglobulinemia? A: it gets thicker (hyperviscous) because of all that serum protein accumulation! Q: How does Epstein-Barr Virus hijack the cell? A: By tricking the B cell to make more IL-10, which suppresses anti-viral reactions Q: How does Measles hijack the cell? A: By inhibiting it from producing IL-12, and therefore prevent Th1 response. Q: What is X-linked Lymphoproliferative Syndrome (XLP)? A: Defect in SH2D1A (SAP-SLAM Associated Protein) – important in enhancing T cell activation uncontrolled T cell proliferation and cytokine secretion can’t control EBV infection Q: What is CCR5 and CXCR4? A: These are the cytokine co-receptors on T cells that HIV use to enter CD4 T cells. Q: What are the glycoproteins on the HIV that bind to CD4 T cells? A: gp120 and gp41 TRANSPLANTATION Q: Distinguish: Autograft vs. Isograft vs. Allograft vs. Xenograft. A: Autograft – transplant from one part of body to another in same person Isograft – transplant from one identical twin to another Allograft – transplant from one person to another Xenograft – transplant from one animal to another Q: What’s the difference between Direct and Indirect allorecognition? A: Direct: T cell directly recognize donor dendritic cell. Indirect: recipient dendritic cell take up donor polypeptides and present to T cell Q: Chronic rejection of organ transplants is caused by which pathway of allorecognition? A: Indirect Allorecognition Q: What are Minor Histocompatibility Antigens? A: receptors on surface of donated transplanted tissue that induce some rejection reaction, even when HLA of MHC is compatible. Q: What are examples of Minor Histocompatibility Antigens? A: Y-chromosome proteins (which are not tolerated by females, even when HLA is identical), polymorphic proteins (that just differ in a few amino acids), stress-induced proteins. Q: What are the targets of allograft and xenograft rejections? A: ABO antigens, MHC I and II, Minor Histocompatibility antigens. Q: What are ways to test for tissue compatibility? A: Agglutination (used in blood typing), Mixed Lymphocyte Reaction, Mmicrocytotoxicity test Q: What are the four types of Graft Rejection? A: Hyperacute (minutes-hours), Accelerated (Days), Acute (days-weeks), Chronic (months, years) Q: What causes Hyperacute Rejection? A: Pre-formed anti-donor antibodies, followed by complement Q: What causes Accelerated Rejection? A: Reactivation of sensitized T cells Q: What causes Acute Rejection? A: Donor Dendritic cells migrate to spleen where they present themselves to recipient T cells Effector T cells go to graft and destroy them. Q: What causes Chronic Rejection? A: lots of possible things: antibodies, immune complexes, slow reaction, etc. Q: What is Graft vs. Host Disease (GVHD)? A: When graft’s T cells attack recipient’s tissue, instead of the other way around. This occurs with bone marrow transplant, where donor’s T cells are made. Q: What are some symptoms of GVHD? A: jaundice, rash, diarrhea Q: What is Immunosuppressive Therapy? A: remove or prevent activation of T cells (i.e. FK506, Rapamycin, Cyclosporin A inhibit IL-2 production) Q: You can’t exactly deplete T cells in bone marrow transplants to solve the problem GVHD. Why? A: Because T cells facilitate engraftment. If you deplete T cells in bone marrow transplant, you become immunocompromised (higher risk of leukemia, fungal infections, and EBV) TUMOR IMMUNITY Q: What is the Immunosurveillance Theory? A: The theory that the immune system protects the body from spontaneous cancerous tumors. Immunodeficient individuals are more likely to develop certain kinds of tumors than general population. Q: What are the immunosurveillance effectors? A: CD8 cells, CD4 cells, NK cells, macrophages Q: How does NK cells know to kill an infected cell and not a healthy cell? A: Infected cells lose their MHC Class I, which the NK’s inhibitory receptor identifies as “self.” Q: What cytokines activate NK cell’s killer functions? A: IFN, IFN- secreted by infected cells. Q: What cytokine activates NK cell’s cytokine production function? A: IL-12, causing it to release INF-gamma, which activates macrophages and CTL Q: What are the two categories of Tumor Antigens? A: Tumor Specific Antigen (TSA) – expressed on tumor cells, mutant protein Tumor Associated Antigen (TAA) – expressed on normal cells, normal protein but overexpressed. Immunity against tumors can target TSA and TAA. Q: What is one way that TSA can be made? A: but cutting two non-related peptides by the proteasome and pasting them together. Q: What are some ways that Tumors can evade immune system? A: down-regulate HLA, so CTL can’t recognize them. Q: What is MIC and what is NKG2D? A: MIC is expressed on tumor cells. NKG2D on NK cells bind MIC and kills the tumor cell. Q: What is one thing tumor cells can do to MIC to inhibit NK cells from killing them? A: tumor cells can cut off own MIC to become soluble. NK cells bind soluble MIC instead of tumor membrane-bound MIC, so it does not kill. Q: What is TGF-beta’s role in tumor? A: TGF-beta inhibits proliferation of cells, so it inhibits Th1 and CTL proliferation. Tumor itself is immune to TGF Q: What are some ways to treat cancer via immune system? A: via IFN-alpha (activates NK), IFN-gamma (activates CTL), IL-2 (T cell or NK proliferation) Q: What are two ways to make conjugated monoclonal antibodies against cancer? A: conjugate a toxin to an anti-cancer antigen antibody. The antibody binds to the cancer antigen, brings the toxin into the cancer cell, and kills the cancer cell by apoptosis. You can also conjugate a anti-cancer antigen antibody to an irradiating substance, which binds to the cancer cell and kills it by radiation.