Institutional Review Boards
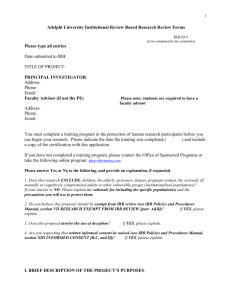
advertisement

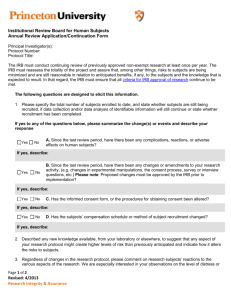
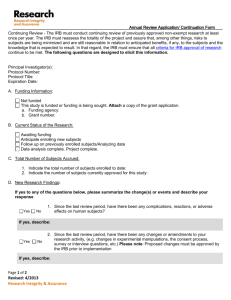
Institutional Review Boards Historical Perspective: Institutional Review Boards (IRB’s) were created as a result of past abuses of the human research process. Even after the Nuremburg Code, which addressed the ethics of research and informed consent, unethical practice in research continued. An example was the Tuskegee Syphilis Study (1932 – 1972). In this study, African-American men with syphilis where withheld medical treatment after treatment became available. These abuses demonstrated the need for an ethical guideline for human research protection. These ethics were outlined in the Belmont Report of 1979, which provided guidance for legislation, (Perlman, 2004). The Protection of Human Subjects Law (45 CFR and 21 CFR 50 & 56) was signed into law in 1981 Researchers could no longer decide for themselves if their studies were ethical or not. Now an IRB would make these decisions. The IRB: An IRB is a group of people who oversee research. This group is made up of scientific, non-scientific, professional and lay persons from the community, who are not associated with the studies being reviewed. The purpose of an IRB is to ensure protection of the rights and welfare of clinical trial participants. An IRB has the authority to approve, require modifications or disprove research, (45 CFR 46.109(a)). No study treatment or informed consent can take place until the protocol has full IRB approval. Institutional administration cannot dictate or overturn the decisions of an IRB. Protocol Review: Prior to IRB submission of a protocol there are several reviews that may take place. Scientific Review Committees: At larger institutions a scientific review may take place prior to IRB submission. This is required for all NCI-designated Cancer Centers. The committee evaluates the study for scientific merit, and feasibility at their specific site. If the committee approves the study, then it is submitted to the IRB. Smaller institutions may not have a scientific review committee, but there should be a mechanism in place to evaluate if the study is feasible & is acceptable scientifically at the institution. IRB Review: The Institutional Review Board reviews the research from an ethical stand point to assure that patient’s rights are up held. Institutions utilizing the National Clinical Trial Network (NCTN) studies, must utilize the Central IRB, otherwise the IRB of record for the institution can be used. Federal Wide Assurance: Every institution that conducts federally funded research must: Utilize an IRB that is registered with the Office for Human Research Protection (OHRP) (Trocky, 2013 & 21 CFR 56.106). Sign a Federal Wide Assurance (FWA) agreement with the Office for Human Research Protection, (OHRP). An assurance is a legal agreement between an institution and the government that research will be conducted in accordance with federal regulations & Good Clinical Practices (GCP). http://www.hhs.gov/ohrp/assurances/assurances/index.html Recruitment Material: Any type of advertisement, including social networking, must be reviewed and approved by an IRB before it can be used. Advertising, is considered part of the informed consent process, and as such is reviewed with the same scrutiny. The following is a list of IRB submission requirements, based on information from Filchner, K. & Herman, P.B., 2008; U.S. Food & Drug Administration, 2009. For further information, refer to the Code of Federal Regulations on-line @ http://www.hhs.gov/ohrp/humansubjects/guidance/45cfr46.html Developed: 3/3/07 Revised 1/16/08; 2/24/14 1 of 3 INITIAL REVIEW Submit the following: IRB specific application Full Protocol Consent Recruitment material Investigators Brochure List of Key Personnel & Responsibilities Means of patient identification IRB looks at: Minimized & reasonable risks Sound Research Design Equitable selection of subjects Informed consent Adequate provisions for data monitoring Adequate provision to protect privacy Vulnerable populations Other information specific to local rules and regulations EXPEDITED REVIEW An expedited review may be used in the following circumstances. Involves no more than minimal risk. Minor changes in previously approved projects, provided the project has been reviewed and approved within the past 365 days It is the IRB that ultimately determines the review type for an initial protocol or protocol amendment. Expedited Adverse Event Reporting (AKA: Serious Adverse Event (SAE)/Adverse Drug Reaction (ADR) Expedited reporting of adverse events will be required of IRB’s. Check with your IRB for the specific requirements. INFORMED CONSENT DOCUMENT Informed consent is a process and should be affirmed throughout the course of treatment (e.g. at each visit). Each consent should have a version and expiration date. Most IRBs stamp the consent with this information or include it in the footer. Each IRB will have an Informed Consent Document template. Check with your IRB for the specific requirements. The NCI sample template can be used as a guide: Consent template available @: http://ctep.cancer.gov/guidelines/templates.html . Informed Consent Document: Regulatory requirements: Consent recommendations: 8 required elements Lay language Involves research Avoid words with > 3 Risks syllables. Benefits < 8th grade level Alternatives 12 – font Confidentiality L-justified, R-Ragged Compensation & Dates: Initial review, med. Tx for injury revisions, expiration Contact info. Approval date by IRB Voluntary Line in footer for subject to initial each page Developed: 3/3/07 Revised 1/16/08; 2/24/14 6 Additional elements Unforeseeable risks (embryo/preg.) Circumstances for subject study termination. Costs Consequences of withdraw Additional findings communicated to patient. # of subjects 2 of 3 Reading level can be calculated in MS Word. Click the File tab, and then click Options. Click Proofing. Under When correcting spelling and grammar in Word, make sure check grammar with spelling check box is selected. Select Show readability statistics. CONTINUED REVIEW Requirements vary with each individual IRB Must at least be reviewed annually (< 365 days) per the regulations o Higher risks Some examples of information to include in report: o # of subjects registered, locally and nationally o Summary of subject’s experiences o # of withdrawals, and reasons o Any interim results or new information if available o Personnel changes o Copy of the current IRB approved consent document References: Filchner, K. & Herman, P.B. (2008). Institutional review boards/protocol modifications. . In Klimaszewski, A.D., Bacon, M.A., Ehrenberger, H.E., Ford, B.A.& Westendorp, J.G. (Ed.) [Second. Ed]. Manual for Clinical Trials Nursing.(pp. 91-96). Pittsburgh: Oncology Nursing Press, Inc. Perlman, D. (2004). Ethics in clinical research: A history of human subject protections and practical implementation of ethical standards. SoCRA, Issue 40, 37-41. Trocky, N. (2013). Institution & IRB registration. The Monitor, 27(5), 49-52. U.S. Food & Drug Administration (2009). Code of federal regulations (Title 45, Part 46). Washington, DC: U.S. Government Printing Office. Developed: 3/3/07 Revised 1/16/08; 2/24/14 3 of 3