Age 65-74: Highest Rate Of Newly Sx. LEAD
advertisement

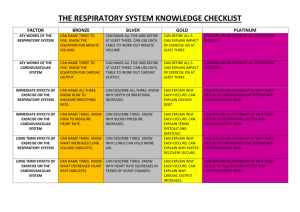
Common Cardiovascular Problems NUR 475 – Family Nurse Practitioner III Common Cardiovascular and Peripheral Vascular Problems – Part 2 Prevention, early identification and effective treatment significantly reduces cardiovascular morbidity and mortality Nurse Practitioners must focus on health maintenance and disease prevention, as well as diagnosis and management of disease. This includes a focus on the foundations of health. A healthy diet Regular physical exercise (not just activity) Good quality and quantity of sleep Good hygiene Common Chief Complaints Chest pain Palpitations Dizziness Fatigue Lower extremity swelling Common Cardiovascular disorders HTN - Hypertension Hyperlipidemia CAD - Coronary Artery Disease ACS – Acute Coronary Syndrome MI – Myocardial Infarction Syncope AF - Atrial Fibrillation Cardiac valve Endocarditis – bacterial prophylaxis Cardiomyopathy CHF – Congestive Heart Failure Common Peripheral Vascular disorders Arterial Venous 1 Common Cardiovascular Problems 2 Atrial fibrillation Clinical guidelines Clinical guidelines http://circ.ahajournals.org/content/114/7/700.full.pdf+html and http://circ.ahajournals.org/content/123/1/104.full.pdf Most common cardiac dysrhythmia - ↑ incidence and prevalence with aging Pathogenesis o May be precipitated by trauma, obstructive sleep apnea, pericarditis, chest surgery, thyroid disorders, pulmonary disease, drugs, alcohol excess/withdrawal o 5-fold increased risk of stroke Symptoms o Palpitations (acute onset) o Fatigue (chronic) Signs o Irregular and often tachycardic heart beat o High rate can lead to hypotension, myocardial ischemia and dysfunction o Pulse deficit Diagnostic testing o ECG – fast and irregular atrial rate, variable ventricular response o Chest x-ray (pulmonary disorder?) o Doppler echocardiogram (valvular disease, LVH) o In selected cases - TSH/T3/T4, CBC, CMP, polysomnogram Treatment – 3 objectives (rate control, prevention of thromboembolism, and correction of the rhythm disturbance) o Prevention of thromboembolism - Anticoagulation Warfarin or dabigatran (Pradaxa) – lower risk of major bleeding, no dietary restrictions, no regular INR, drug-drug interactions unlikely, more GI side effects, not for valvular disease (1) See: Outpatient management of Anticoagulation Therapy at http://www.aafp.org/afp/2007/0401/p1031.html (2) See Warfarin Therapy: Evolving Strategies in Anticoagulation at http://www.aafp.org/afp/1999/0201/p635.html?printable=afp Aspirin and clopidogrel o Rate control, rhythm correction Goal of rhythm <110 bpm β blocker, verapamil, diltiazem or digoxin amiodarone versus dronedarone (Multaq) Cardioversion for new onset; in selected cases for chronic after anticoagulation Catheter ablation in selected patients Referral o Hospitalize when hemodynamically compromised o Symptomatic with or without rate control o Poor rate control Case study #8 (in class) - notes Common Cardiovascular Problems Cardiac valve disorders Regurgitation/insufficiency o Retrograde (backward) flow of blood “upstream” when the valve should be closed Stenosis o Obstruction of the (forward) flow of blood across an open valve S1=closing of atriovenricular valves (mitral and tricuspid) S2= closing of semilunar valves (aortic and pulmonic) Murmurs graded I-VI Systolic murmurs o Aortic stenosis S&S; syncope, angina and dyspnea on exertion Associated findings; rales in lung bases with LVH, JVD, hepatomegaly, peripheral edema with RVH o Pulmonic stenosis (more common in women) More common in women Often hemodynamically insignificant S&S; dyspnea, cyanosis, syncope on exertion, palpitations, right heart failure o Hypertrophic cardiomyopathy or idiopathic hypertrophic subaortic stenosis Cause unknown, may be genetic S&S; dyspnea on exertion, chest pain, syncope (during or after exercise), atrial fibrillation, AND Ventricular dysrhythmias causing sudden death especially after exertion – important with athletic screening → What history should be obtained and documented? What physical examination should be done and documented? o Mitral regurgitation S&S; dyspnea and palpitations most common, atrial fibrillation Bacterial endocarditis concern o Mitral valve prolapse 10% of young women, generally hemodynamically insignificant S&S; usually asymptomatic, palpitations Bacterial endocarditis concern o Tricuspid regurgitation Common with pulmonary hypertension and LVF S&S; fatigue, abdominal and ankle swelling, ascites, liver congestion, atrial fibrillation o Physiologic or functional murmurs Temporary increase in blood flow due to anemia, hyperthyroidism, pregnancy and fever o Innocent murmurs Commonly occur in children and young adults Caused by turbulent blood flow due to great velocity of flow during early systole Diastolic murmurs – almost always pathologic! o Mitral stenosis S&S; dyspnea on exertion, hemoptysis, rales, orthopnea, atrial fibrillation 3 Common Cardiovascular Problems o Tricuspid stenosis Often caused by rheumatic fever S&S; fatigue, right upper quadrant discomfort (enlarged liver) o Aortic insufficiency/regurgitation Life threatening → acute pulmonary edema (dyspnea, orthopnea, cough) Most common cause is infective endocarditis with rheumatic fever Chronic S&S; palpitations possibly due to ventricular dysrhythmias, dyspnea and chest pain (LVH), diaphoresis o Pulmonic insufficiency/regurgitation Often in pulmonary hypertension and LVH S&S; cor pulmonale, dyspnea on exertion o Ventricular septal defect Congenital Left-to-right shunting causes increased blood flow over pulmonic valve Large defects - dyspnea on exertion o Atrial septal defect Congenital Left-to-right shunting causes increased blood flow over tricuspid valve to the lungs S&S; asymptomatic until early adulthood then dyspnea on exertion, palpitations, atrial dysrhythmias, RHF Diagnostic testing o Chest X-ray – enlarged ventricles o ECG – dysrhythmias o Echocardiogram – valve disease o Cardiac catheterization – unstable, surgical intervention Case study # 9 (in class) – notes Bacterial endocarditis prophylaxis See clinical practice guidelines http://circ.ahajournals.org/content/116/15/1736.full.pdf Used in what 2 conditions? 4 Common Cardiovascular Problems Pericarditis Case study #10 (in class) – notes First must rule out MI and cardiac tamponade (serious complication requiring urgent pericardiocentesis) Essential Evaluation: o Detailed symptom description and relevant history o Vital signs including temperature o Chest and cardiac examination o ECG electrical alternans with tamponade diffuse ST ↑ and associated PR depression o If suspect MI Cardiac biomarkers o If suspect pericarditis CBC (↑ leukocytes), ESR (↑) Chest x-ray (normal or effusion and ↑ cardiac shadow) Pathogenesis o Acute pericarditis (inflammation for 1-2 weeks) 5% of non-ischemic chest pain Idiopathic in most cases, presumed viral Dressler syndrome – 24-72 hours after transmural MI Chest trauma (including post coronary artery by-pass surgery) o Constrictive pericarditis (occurs over time due to scarring of pericardial sac from a disease processes) Connective tissue disorders (rheumatoid arthritis, SLE, scleroderma, sarcoidosis) Bacterial, viral or fungal infections including HIV and TB Chest trauma (including post coronary artery by-pass surgery, AICD pads) Neoplastic Uremia Irradiation Idiopathic S&S o Sharp, stabbing, crushing, steady anterior chest pain o Pain worsens with inspiration, lying flat or leaning forward o May be associated with shortness of breath, fever, chills and malaise o Additionally in constrictive pericarditis S&S of RHF and low cardiac output Lower extremity edema Abdominal complaints Hepatic congestion, possibly jaundice Atrial fibrillation Tricuspid regurgitation 5 Common Cardiovascular Problems 6 Differential Diagnosis; see chest pain section Differentiation of Acute Pericarditis from Myocardial Ischemia or Infarction Clinical finding Acute Pericarditis M. Ischemia or Infarct Chest pain Character Duration *Change with position Change with respirations Response to nitroglycerin Electrocardiography P-R segment depression Q waves Ration of ST-segment elevation to T-wave amplitude in V6 ST-segment elevation No change T waves Inverted after ST segments have normalized Inverted when ST segments are still elevated *Friction rub on physical exam Physical Examination o Pericardial friction rub in 60-70% o In constrictive pericarditis Marked JVD Kussmaul sign Pericardial knock Hepatomegaly Spider angiomata Palmar erythema Additional diagnostic testing o Echocardiogram o CT or MRI if workup inconclusive-consult cardiology Treatment (Goal is to relieve pain and prevent complications. Most cases are uncomplicated and can be managed in outpatient setting.) o Acute pericarditis Focus on cause Common Cardiovascular Problems 7 NSAIDS (ibuprofen 600-800 mg 3 times a day for 2 weeks); can use aspirin, avoid Indocin especially in elderly (↓ coronary flow) Colchicine - 2-3 mg loading dose followed by 1 mg daily for 10-14 days Corticosteroid – for unresponsive cases only, (can cause relapse); 60 mg for 2 days and taper over 7 days o Chronic pericarditis Corticosteroids may be helpful Pericardiectomy Diuretics and sodium restriction with RHF Avoid β blockers and calcium antagonists (HR of 80-90 bpm acceptable, use Digoxin in atrial fibrillation first) Hospitalize for acute pericarditis for o Cardiac tamponade o Body temperature control o Anticoagulation therapy o Surgical treatment o Immunocompromised Case study # 11 (in class) – notes Cardiomyopathies Dilated o Most common o 50% idiopathic Hypertrophic (HCM) previously known as hypertrophic obstructive cardiomyopathy and idiopathic hypertrophic subaortic stenosis o Resource: http://www.mayoclinic.com/health/hypertrophiccardiomyopathy/DS00948 o Prevalence 1:500 o Mutation of 10 genes coding protein of the cardiac sarcomere o Slight male predominance up to mid-life; female predominance over 60 years of age o Inappropriate and marked left ventricular hypertrophy, ranging from mild to extreme, esp. localized hypertrophy, typically in the anterior septum. This hypertrophy may result in areas of ischemia or infarction due to abnormal microvasculature, impaired coronary vasodilator reserve, or mismatch between myocardial mass and coronary circulation. This causes scarring. o Outflow tract obstruction, not demonstrated in the majority; causes a loud systolic murmur and may be symptomatic with exertion intolerance, syncope, or sudden death o Highest predictors of sudden death – marked LVH, abnormal BP response to exercise, syncope, history of cardiac arrest, documented sustained ventricular tachyarrhythmia and family history of sudden death Restrictive o Less common o 50% due to noninfiltrative (familial, diabetic, others) and infiltrative (amyloidosis, sarcoidosis, others) Common Cardiovascular Problems Arrythmogenic right ventricular Unclassified S&S of HCM Majority asymptomatic or have mild symptoms Dyspnea, chest pain, presyncope or syncope with symptoms worse with exertion Primarily related to diastolic dysfunction Atrial fibrillation occurs in ¼ of patients thus hemodynamic compromise because of inadequate filling of the hypertrophied ventricle. Physical Examination for HCM Forceful and enlarged precordial impulse, often laterally displaced Murmur results from flow through the left ventricular outflow tract, and is usually a harsh crescendo-decrescendo, starts well after the first heart sound and is best heard between the apex and left sterna border. The murmur increases with maneuvers that increase the gradient through increased contractility, decreased preload, or decreased afterload; conversely, the murmur decreases with interventions that decrease contractility, increase preload or increase afterload. i) Squatting (increased afterload) = decreased murmur ii) Standing (decreased afterload) = increased murmur iii) Valsalva (decreased preload) = increased murmur iv) Precordial impulse-presystolic, systolic, and late systolic impulse (“triple ripple”) Diagnostic testing for HCM Echocardiogram – examines outflow tract obstruction, septal hypertrophy which is usually asymmetric, and enhanced contractility. Systolic anterior motion of the anterior mitral valve is present if there is outflow tract obstruction. ECG – LVH, prominent Q waves in the inferior and lateral leads due to septal hypertrophy. Giant negative T waves suggest the apical variant of HCM Stress testing Treatment for HCM β blockers are considered the initial therapy of choice AICD if considered high risk for sudden death Heart Failure 8 Case study #12 (in class) – notes Epidemiology o Increasing incidence and prevalence ~ 5000,000 new cases/year o > 75% of new and existing cases in 65 and over age group Pathogenesis o Normal → injury → compensatory hypertrophy (remodeling) → dilated and fibrotic (distorted architecture) o Impaired ability of ventricles to fill or eject blood o Circulatory and neurohormal response (SNS, RAAS) to cardiac dysfunction o Systolic dysfunction; inability of the left ventricle to pump blood to the body Ejection fraction less than 40% Myocardial contractility Heart rate (↓ SV → ↑ HR → ↓ CO = HF) Common Cardiovascular Problems Preload (end-diastolic volume or pressure) Afterload (ventricular wall tension during systole → ejection from left ventricle) o Diastolic dysfunction; inability of left ventricle to relax and fill normally o Risk factors: Physical inactivity, BMI ≥ 30, excessive alcohol intake, smoking, high sodium intake Symptoms o LV failure Exertional dyspnea → orthopnea → paroxysmal nocturnal dyspnea → at rest Others; fatigue, cough, nocturia o RV failure Peripheral edema, loss of appetite, nausea Often LV symptoms Signs o LVF – S3, rales o RVF – S4, JVD, peripheral edema, hepatomegaly, acites o In many cases no specific signs Differential Diagnosis o Underlying causes; CAD (“plumbing”), HTN, cardiomyopathies, valvular disease (“structure”), dysrhythmias (“electrical”) o Precipitating factors; MI, PE, exacerbation of HTN or COPD, infections, drugs, etc. o Non cardiac: pulmonary disease, thyroid abnormalities, hemoglobinopathies, renal dysfunction, obstructive sleep apnea, inflammatory disorders, metabolic disorders, drugs and toxins o Other causes of peripheral edema Diagnostic testing o Chest x-ray o Brain natriuretic peptide (BNP) – specific to ventricular stretch and correlated with severity o Echocardiogram Treatment o Acute IV loop diuretics and vasodilators o Chronic management – see Clinical guideline at http://www.annals.org/content/155/4/252.full.pdf+html First line: ACE-I and β-blocker or ARB if intolerant to ACE-I Referral – hospitalize when unable to manage symptoms in the office/home o Requires IV drug therapy, oxygen Follow-up and prevention o Proper medication use o Guided exercise o Smoking cessation o Weight reduction o Immunization; flu and pneumonia 9 Common Cardiovascular Problems 10 Common Peripheral Vascular disorders Occlusive or inflammatory disease in the peripheral arteries, veins or lymphatics. Differentiation of Arterial and Venous Insufficiency Sign Pulse Edema Pain Temperature Color Arterial Insufficiency Venous Insufficiency Decreased/absent Normal Absent or mild Significant Severe Absent/mild Cool Normal Pallor with elevation; dusky red on Hyperpigmentation; cyanotic on dependency dependency Skin Thin, atrophic; risk of gangrene Thick; risk of stasis ulcer Goolsby, M. J. & Grubbs, L. (2011). Advanced assessment: interpreting findings and formulating differential diagnosis (2nd Ed.). F.A. Davis: Philadelphia, PA. Arterial Disease Arterial Insufficiency (PAD, LEAD) See clinical guidelines at http://content.onlinejacc.org/article.aspx?articleid=1146931&resultClick=1 Epidemiology o Symptoms of lower extremity arterial insufficiency are common in old age. o Affects 12-20% of people older than age 65 o Affects 8-12 million individuals of all ages in the United States o Age 65-74: Highest rate of newly sx. LEAD– Lower Extremity Arterial Disease o In middle age, affects men 2X > women o Gender disparity begins to disappear after age 65 Pathogenesis o Refers to any occlusive process that limits blood flow to limbs or to vital organs other than the heart o Underlying atherosclerosis o Most often due to enlarging atherosclerotic plaques in the distal aorta and its branches o Rarely confined to the lower extremities…By the time lower limb ischemia is symptomatic, cerebrovascular disease and CAD are usually present as well. o Risk factors (same as CAD); DM, HTN, Obesity, age, hyperlipidemia, tobacco use S&S o Initially, may be asymptomatic, progresses to intermittent, and for some then severe ischemic pain o Rapid onset of pain, often described as cramping with activity o Aortoiliac disease – pain in buttocks or thigh muscle o Femoral or popliteal diseases – pain in calf muscle o Relief from pain with rest (intermittent claudication) 3 Clinical Presentations of LEAD o Young smoking man, age 40-60, with hyperlipidemia & family hx. of vascular disease Common Cardiovascular Problems o Man or woman age 65-75 who c/o calf aching or burning o Diabetic patient of either sex, with years of suboptimal control Differential Diagnosis o Venous insufficiency o Peripheral neuropathy o DJD of lumbar spine Physical Examination o General; hair distribution, nails, muscle bulk o CV o Lower extremity vascular exam o Diminished or absent pulses o Blanching with limb elevation o Dependent rubor o Decreased distal skin temperature o Ulcer’s (tissue loss) o Lower extremity neurological exam o DTRs o Sensation o Strength Diagnostic testing o ABI (Ankle-Brachial Index) o Normal 1.00 or higher o < 0.5 = impaired flow → vascular consult Treatment o Daily exercise o Foot care o Treat hypercholesterolemia, HTN and DM o No smoking o Debridement of ulcers o Antiplatelet therapy (aspirin, clopidogrel) o Pentoxifyline or cilostazol, is selected cases o Arterial reconstructive surgery o Percutaneous transluminal angioplasty or stent Raynaud’s phenomenon Usually benign, may have underlying disorder (see Faci page 740) S&S o Fingers blanch, next cyanotic, then red with cold exposure Treatment o Keep hands warm o CCB or α-adrenergic antagonists, may be helpful Case study # 13 (in class) – notes 11 Common Cardiovascular Problems 12 Venous Disease Varicose veins – see readings Superficial Thrombophlebitis – see readings Deep Venous Thrombosis (DVT) - See clinical guidelines: o Management of venous thrombolembolism: http://annals.org/article.aspx?articleid=732701 What are the usual causes of VTE (venous thromboembolism)? What might be the etiology if it is an “idiopathic” VTE? Post-thrombotic syndrome: What is this? Chronic Venous Insufficiency (CVI) Essentials Features o History of prior DVT or leg injury o Edema, stasis (brawny) skin pigmentation, subcutaneous liposclerosis in the lower leg o Large ulcerations at or above the ankle are common (stasis ulcers) Epidemiology o One quarter to a third of all adults in western world have varicose veins o USA-80 million; estimates of the prevalence 7-60% of adults; Best point estimate is 30% o 1 million-venous ulceration due to venous incompetence of superficial system o 100,000 disabled Pathogenesis o Chronic elevation in venous pressure; normally can hold large volume changes that can occur with exercise; when valves in the deep or perforating veins are destroyed as in thrombophlebitis, valvular reflux and bidirectional flow result in high ambulatory venous pressures. Damage to any component of the calf muscle pump can cause dysfunction of the pump, thus leading to superficial varicosities, edema, fibrosis of the subq tissue and skin, hyperpigmentation, and later, dermatitis and ulceration. o Long-term complication of venous thrombosis due to destruction of deep vein valves o Potentially life-threatening complication → thrombophlebitis leading to pulmonary emboli o Frequently caused by varicose veins o Often secondary to DVT o Other causes; trauma, pelvic neoplasm, immobilization, pregnancy S&S o Gradual onset of aching, heaviness, tiredness, cramps, itching, burning, restlessness or pain in lower leg for hours to days o Question about prolonged immobility or travel o See the following website for pictures of common findings: http://www.veinclinics.com/cme/skin-findings.html Common Cardiovascular Problems 13 Differential Diagnosis o DVT o PAD o Peripheral neuropathy o Lymphedema Associated with brawny thickening in the subcutaneous tissue that does not respond to elevation; edema is particularly prominent on the dorsum of the feet, and in the toes (sausage toe); varicosities are absent, often history of recurrent cellulitis o Heart Failure o Chronic Renal Failure Physical Examination o Pulses o Ankle edema - earliest sign Check groin to ankle Unlike the edema associated with salt-retaining conditions such as heart failure and nephrotic syndrome, the edema that precedes venous ulcer formation accumulate under high pressure, creating tissue damage that is tender. o Thinning and hyperpigmentation of skin Common Cardiovascular Problems 14 Hyperpigmentation-hemoglobin deposited in the tissues is digested, but the iron remains in the dermis as hemosiderin and produces a brown or brown-red pigmentation in skin surrounding ulcer Stasis Dermatitis-DeGowin-increased venous and capillary pressures lead to inflammation, edema, subcutaneous fibrosis, and skin atrophy with hemosiderin staining. Often mistaken for cellulitis. With chronic disease, the subcutaneous tissues become fibrotic and the edema no longer pits (brawny edema). o Superficial veins and varicosities Include inspection of abdomen telangiectatic veins o Venous stasis o Ulcers o Lower extremity neurological exam Proximal and distal strength Sensory exam; particularly to sharp and dull Deep tendon reflexes Casual, toe, heel and tandem gaits Interesting cases o Lipodermatosclerosis-“Champagne bottle” appearance- leg assumes the shape of an inverted champagne bottle – wide at knee narrow at the ankle) o Eczema to ulceration - case study of Mr. Crabbe: http://www.worldwidewounds.com/2005/november/Doherty/Encourage-patientInvolvement-Mgt-Lymphovenous.html o Review website for pictures of ulcers at http://www.bmj.com/cgi/content/full/320/7249/1589 Diagnostic testing o Duplex Doppler ultrasound – accurate for clots in large vessels not small thrombi Not needed with intact skin and normal pulses o Venography – most accurate o MRI – if ulcer and considering osteomyelitis o Labs to rule out autoimmune/blood disorders Treatment o Prompt treatment for DVT with anticoagulants ↓ risk o Elevation of legs intermittently during the day and at night o Avoidance of prolonged sitting or standing Common Cardiovascular Problems 15 o Support or compression stockings (TEDs not enough pressure) If ulcer present use the Rule of 6, see below Compression Strength 8-15mm 15-20mm 20-30mm 30-40mm 40-50, 50-60 mm Indications Leg fatigue, mild swelling, stylish Mild aching, swelling, stylish Requires prescription-Aching, pain, swelling, mild varicose veins Requires prescription-Aching, pain, swelling, varicose veins, post-ulcer Requires prescription-Recurrent ulceration, lymphedema o o o o o Unna boot for stasis ulcers Pentoxifylline may be helpful (consider drug/drug interactions) Sclerotherapy Ambulatory phlebectomy Procedures, see http://www.veindirectory.org/content/surgical_methods.asp Endovenous ablation with laser or radiofrequency-video Subfascial endoscopic perforator surgery (SEPS) Transilluminated Power Phlebectomy (TIPP) Surgical vein ligation or stripping Refer for non-healing venous ulcers, arterial ulcers and neuro/DM Location Lesion features Surrounding skin Palpation findings Comparison of 3 common types of leg ulcers Venous Arterial Neuro/DM Garter area of leg-will Pressure sites/toes, Pressure sites/plantar, break down/medial heels, foot arches heels, toes leg Shallow, partial Punched-out, eschar Punched-out thickness with (blackened if necrotic) irregular borders/shaggy Hyperpigmented, Hair low, not Hair loss, not thickened, with hyperpigmented, hyperpigmented, dermatitis-stasis atrophic callus changes Non-pitting, tight Peripheral pulses Altered sensation with edema; peripheral decreased, capillary touch, vibration, pulses may be normal refill time increased peripheral pulses decreased