chart materials appropriate for Simulation 3
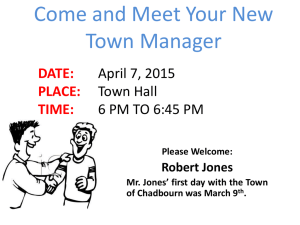
advertisement

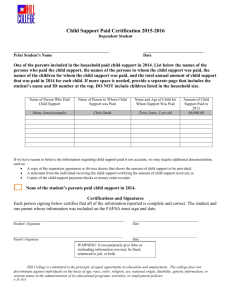
PATIENT CHART Chart for Judy Jones Simulation #3 STUDENT NAME:_______________________________ PATIENT INITALS: ___J.J._______________________ CLINICAL DATE(S): _____________________________ INSTRUCTOR: _______________ Chart Materials Judy Jones – Simulation #3 © National League for Nursing, 2014 1 Patient Name: Judy Jones Room: DOB: 11/13/xx Age: 85 MRN: 57428 Doctor Name: Annette Parks, MD Date Admitted: Diagnosis: Pneumonia Patient Report (Report from nurse ending shift) Current time: 1400 (day 9 of hospitalization) Situation: Judy Jones is an 85-year-old female patient of Dr. Annette Parks who was admitted 2 days ago with a diagnosis of community-acquired pneumonia. We are currently treating her with IV antibiotics and respiratory treatments. Background: Judy Jones is an 85-year-old female who was admitted 9 days ago with a diagnosis of community-acquired pneumonia, which has resolved. Ms. Jones has a medical history of hypertension that is controlled by spironolactone, cervical spondylosis, and hyperlipidemia that is controlled by diet. She has mild dementia and during this hospitalization she developed delirium that was manifested by seeing children underneath her hospital bed, wandering the halls, and agitation. She was given Ativan (lorazapem) which seemed to help initially, but then she became more agitated and delirious. A few days ago she developed atrial fibrillation and is being medicated with amiodarone 800mg PO every day. Tomorrow Ms. Jones is scheduled to be transferred to a rehabilitation center for a short time before returning home. Assessment: Ms. Jones is alert and oriented to self, but still needs periodic orientation to time and place. She is forgetful and confusion is present all day. The last three days she has not been sleeping well. The first Mini-Cog we did indicates possible dementia. She was having auditory and visual hallucinations at the time. The second was even worse. That was done when she became more delirious after the doses of lorazapam. Her most recent one was done yesterday and it was better, but her daughter says she is not back to her baseline of cognitive functioning – her level before she developed the pneumonia. Judy’s heart rate is irregular, ranging from 70 to 90 beats per minute. Dr. Parks wants us to call if she has a heart rate greater than 120 beats per minute. Her last set of vital signs were: temperature 98.6 F, HR 76, RR 18, BP 128/64, pulse oximetry 96% on room air. Judy occasionally has a productive cough of white sputum. Her lungs are clear; occasionally you will hear scattered rhonchi that clear with coughing and deep breathing. She needs to be reminded to use her incentive spirometer, and how to use it. Ms. Jones is on a regular diet and has a good appetite. Her abdomen is soft with positive bowel sounds; her last bowel movement was this morning. She is ambulating to the bathroom on her own with a steady gait and urinating without difficulty. Her skin is clean, dry and intact with no areas of breakdown. Recommendation: If Judy is sleeping, please let her rest. She really needs her sleep. If her heart rate goes above 120 beats per minute be sure to call the doctor. Chart Materials Judy Jones – Simulation #3 © National League for Nursing, 2014 2 Provider’s Orders Allergies: Sulfa Date/Time: Tuesday 1. Transfer to Rehabilitation Center in AM 2. DIET: Regular diet 1500 3. VITAL SIGNS: Q4 hours. Call MD if HR greater than 120 per minute 4. ACTIVITY: OOB ad lib 5. THERAPY: a. Incentive spirometry 10 times every hour while awake 6. MEDICATIONS: a. Aricept 10 mg PO q hs b. Spironolactone 50 mg PO q day, hold if systolic BP is less than 90 c. Ibuprofen 300 mg PO q 6 hours PRN neck pain d. Amiodarone 800 mg PO Q day Annette Parks, MD Medical Reconciliation Form Source of medication list (check all that apply) patient medication list, patient/family recall, pharmacy, PCP list, previous discharge paperwork, MAR for facility Allergies: NKA Medication Name Dose Route Frequency Last Dose Continue/DC Amiodarone 800 mg PO Daily C DC Aricept 10 mg PO HS C DC Spironolactone 50 mg PO C DC Ibuprofen 300 mg PO Daily, hold if systolic BP is less than 90 Q4 hours PRN neck pain C DC Provider Signatures Date/Time Today Initial AP Provider Signature Annette Parks, MD Initial LS Nurse Signature Lisa Sousa, RN Nurse Signatures Date/Time Today Chart Materials Judy Jones – Simulation #3 © National League for Nursing, 2014 3 Reviewed on Transfer by: Reviewed on Discharge by: Scan to Pharmacy Time: Date: Date: Date: Patient Name: Judy Jones Physician: Annette Parks, MD/Medical Team B Diagnosis: Pneumonia Age: 85 Gender: Female Height: 5’7” Weight: 115 lbs Major Support: Daughter Karen Jones Phone: 555-555-5555 Karen (daughter) 555-555-5566 Type of Operation: None History: Hypertension, cervical spondylosis, hyperlipidemia, and dementia (short term memory issues, sequencing and executive functioning deficits) Advanced Directives: No Allergies: Sulfa Fall Precautions: High Isolation Precautions: Standard Restraints: No Diet: Regular Monitoring Vital signs – Q4h Call if heart rate is greater than 120 beats/min Medication Oral medications Respiratory Incentive spirometry 10 times every hour while awake Social History - Widowed - Lives at home with her daughter Karen - Her two sons live approximately one hour away Consults Treatments Activities of Daily Living As tolerated, self-directed Discharge Planning - Transfer to Rehabilitation Center tomorrow Race: Religion: Baptist Medication brought from home: None Diagnostic Studies Chart Materials Judy Jones – Simulation #3 © National League for Nursing, 2014 4 Chart Materials Judy Jones – Simulation #3 © National League for Nursing, 2014 5 Chart Materials Judy Jones – Simulation #3 © National League for Nursing, 2014 6 Chart Materials Judy Jones – Simulation #3 © National League for Nursing, 2014 7