Chronic Kidney Disease Program
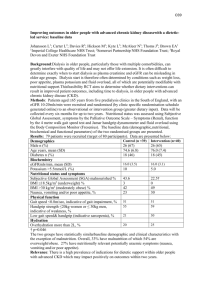
advertisement

Chronic Kidney Disease (CKD) Program Description 2013 (MCCD2012) Table of Contents Program Description and Purpose ...........................................................................................1 Program Goals ...........................................................................................................................2 Member Selection.......................................................................................................................2 Enrollment and Disenrollment Process ...................................................................................3 Criteria for Adding Patients .....................................................................................................4 Sources of New Patients.............................................................................................................5 Criteria for Disenrollment ........................................................................................................5 Initial Intake Process .............................................................................................................................. 6 Interventions............................................................................................................................................ 6 Outcome Measurement .............................................................................................................7 Partnership HealthPlan of California Program Description and Purpose The incidence of chronic kidney disease (CKD) in the US is growing at an alarming rate as supported by corresponding increases in the prevalence of type 2 diabetes and hypertension, two critical factors in CKD. Studies indicate that significant reductions in disease complications and hospitalization costs can be achieved by optimizing several key indices of the quality of care for CKD patients, including: earlier detection of CKD, interventions to delay disease progression, prevention of uremic complications, modification of co-morbidity, and preparation for renal replacement therapy (RRT). Studies stress the need for earlier detection of CKD and indicate that even among high-risk groups, kidney disease (proteinuria >1+, serum creatinine >1.5 mg/dl) is infrequently documented in hospitalized patients. Drug therapy with angiotensin-converting enzyme (ACE) inhibitors, control of blood pressure and blood glucose levels, and restriction of dietary protein intake can retard the progression of kidney disease. However, 33% or fewer patients with CKD are currently treated with ACE inhibitors. The complications of CKD such as anemia, renal osteodystrophy, and acidosis should be diagnosed early and treated aggressively. Anemia is extremely common in CKD patients and is associated with ventricular hypertrophy, exacerbation of angina, reductions in aerobic capacity, decreased cognition, and sexual dysfunction. While dialysis-associated anemia is well recognized, the vast majority (77%) of CKD patients do not receive an erythropoiesis stimulating agents (ESAs) such as Epogen / Procrit / Aranesp™ for the treatment of anemia, although most are anemic before the start of RRT. Even when therapy is initiated, it is often at a level insufficient to correct the anemia. Likewise, the majority of patients who start dialysis have low serum albumin levels, suggesting malnutrition. In addition to the above, the co-morbid conditions that accompany CKD such as diabetes, hypertension, cardiac and vascular disease need timely diagnosis, effective prevention, if possible, and aggressive treatment. Finally, as the patient approaches the need for RRT, disease education, RRT modality selection, timely access placement, and timely initiation of dialysis ensure a seamless transition to RRT. A comprehensive management program that monitors all key indices of quality of care reflects a safer and more efficacious approach to treating CKD and end-stage renal disease (ESRD) patients. Program Goals The goals for the CKD Program are as follows: Page 1 Provide benefit to the largest number of patients that can effectively be case managed with the resources given Help members understand their condition, its implications and how to take informed action to best mange their condition Reduce the complications of CKD Reduce the co-morbid conditions that accompany CKD Slow progression to renal replacement therapy (dialysis/ transplant) Ensure good Advance Care Planning for all participants prior to RRT Reduce the cost of initiation of dialysis Encourage early preparation by creation of access for dialysis treatment as clinically appropriate Encourage home treatment modalities i.e. Peritoneal dialysis Reduce inpatient admissions and or length of stay Member Selection The CKD Program will initially focus on adult (>20) residents of Napa and Solano counties with primary insurance coverage of Partnership HealthPlan of California (PHC) Medi-Cal and/or PartnershipAdvantage lines of business who meet the criteria for classification of CKD. Continuous enrollment for at least six of the last twelve months with a PCP and the PCP agrees the patient would benefit from participating in a CKD program. Based upon program evaluation at six months following implementation, the program may be expanded into other counties in PHC’s service area. The target population for this program is those members who have been determined to have Stage 4 kidney disease or those with Stage 5 kidney disease who are not yet on dialysis. At a later time the Stage 3Bs may be considered. Members already receiving dialysis will be excluded from this program but may receive necessary case management services under PHC’s Episodic or Complex Case Management programs as appropriate. Using extracts from Amysis (PHC’s production system) that are refreshed daily or from other available resources, the member will be screened for participation using the following data: Current Member Age County of residence Line of business Continuous enrollment with a PCP Estimated Glomerular Filtration Rate (eGFR) Using the results of the estimated Glomular Filtration Rate (eGFR), each patient will be categorized by stage of chronic kidney disease. The target population for this program is Stage 4 Page 2 chronic kidney disease or Stage 5 chronic kidney disease, not yet on dialysis. The following table describes the stages of Chronic Kidney Disease. Enrollment and Disenrollment Process Select 60 or so good candidates Initiate intake process Begin to enroll patients, gradually, so as to develop relationships with them, adding about 3 patients per week until the acuity level reaches 20; 2 new patients per week if the total acuity level is 21-25; one new patient per week if the acuity level is 26-30. Page 3 Partnership HealthPlan of California Intensity Scale ACUITY PATIENT CONDITION FREQUENCY OF CONTACT ACUITY SCORE LEVEL 1 Independently accessing services, highest level of self management 1 Phone call q 2 months case remains open to RN Case Manager, telephonic contact completed by Guide/Navigator 0.05 LEVEL 2 LEVEL 3 LEVEL 4 LEVEL 5 Increasing Independence, high level of self management Dependent but Stabilizing medical and psychosocial needs Dependent/ High Risk for ER/ Hospitalization Dependent/ Critical Complex Conditions 1 phone call q month Call Weekly Visit Monthly Call Weekly Visit q 1-2 weeks Call Daily Visit Weekly or more 0.1 1 1.5 3 Criteria for Adding Patients The number of patients in the CKD program optimally is dependent on 1. The acuity of the patients 2. The number of staff providing services and 3. The skills of that staff The overall acuity is calculated by adding the acuity rating of all patients not disenrolled from the program. The target overall acuity score therefore varies by factors 2 and 3 above. A good initial target to consider is: Target: Overall acuity score 26-30 per FTE of total staff working This translates to about 26-30 hours per week per FTE of direct patient contact work, including documentation and transportation to see patients. This allows for vacations, illness, meetings, trainings and other non-patient care responsibilities. It is expected that many high acuity patients will be brought under better control over time and transition to lower acuity, allowing the option of new patients to be recruited. However, if many patients chronically require higher acuity level (4-5), the overall case load may reach a maximum of only 15-20 patients. Sources of New Patients Page 4 Any of the following may be used for ongoing enrollment of new patients in addition to obtaining refreshed data using the initial member selection criteria: Provider suggested (if provider feels the patient is at risk for high cost that could be modified by being in the CKD program) Health plan recommended (by UM or Care Coordination staff) Recent High Cost (Internal Data ) Predictive Modeling (Internal Data ) Criteria for Disenrollment If a patient reaches an acuity level of 1-2 they can continue to be contacted on an intermittent basis by phone by program staff. These patients are not disenrolled, but rather considered lower acuity (stable) patients. Patients are disenrolled from the CKD program in the following circumstances. Client requests to be disenrolled from Care Management services Client does not meet, or no longer meets program enrollment criteria i.e. moves out of the service area Client enrolls in another medical case management program Client initiates long term Renal Replacement Therapy i.e. dialysis or transplant Client refuses to attend scheduled medical appointments The staff has been unable to locate the client for 45-60 days (depending on acuity level) Client death Client placement in long-term custodial care or hospice The client’s needs exceed the Care Management Team’s scope of service i.e.: clinician assessment reveals the client’s cognitive status renders the client inappropriate candidate for self-management education services, or client living conditions are found to be unsafe for staff contact The client exhibits inappropriate or threatening behavior toward staff, or is under the influence of illegal drugs or alcohol during client visits, or exhibits repeated narcotic seeking behavior. The client poses a safety or security risk to staff, other patients, or clinic property If after reasonable case management/disease management services have been implemented, the client demonstrates continuing or repeated non-adherence with the physician/health care provider treatment plan Page 5 Initial Intake Process If a member is identified as meeting Stage 4 or 5 and is not on dialysis, PHC’s electronic data system will be used to identify demographic information (name, address, CIN#, county of residence, etc), and the identity of the assigned member’s primary care physician (PCP). The assigned (PCP) and/or Nephrologist will be contacted to introduce the Program, and the intent to outreach to the member. The member’s clinical status will be discussed along with any barriers to care identified by the PCP. Following discussion with the PCP, the member will be contacted to introduce the program and obtain the member’s permission for enrollment. Once permission is granted the Program Manager will initiate an interview with the member. The interview will include a review of medical history (from the member’s perspective) and standard forms will be used to determine the member’s health status and degree of motivation for active participation toward improvement in self-management skills. The following tools will be used: PHC Health Risk Assessment Patient Activation Measure (PAM) Patient Health Questionnaire (HQ 2 and 9 as appropriate) Veterans RAND 12 item Health Survey (VR 12) During the initial interview process the Program Manager will initiate conversation regarding Advance Care Planning. The goal of this conversation is to define the member’s values and goals and initiate Physician Orders for Life-Sustaining Treatment (POLST) or an Advanced Directive if desired by the member. If the member is not willing to engage in this type of discussion during the initial interview process, the Program Manager will continue to encourage the discussion intermittently during the entire period of enrollment. Based upon the member’s responses to the interview process the Program Manager will work with the PCP and or Nephrologist to develop the member’s individualized care plan. The Plan will include an action plan addressing the member’s priorities. The framework of the Care Plan and Action Plan to include the following four domains: Ensuring access to care/services Optimizing Physical Health Optimizing Psychosocial Health Optimizing Self Management Interventions Care management methodology will include use of Motivational Interviewing and Coaching for Activation. Interventions will be tailored to the need of the individual member but will include, at a minimum, the following: Care Plan development with PCP and/or Nephrologist Action Plan development with member Setting timely intervals for follow up Page 6 Providing ongoing education and encouragement on the relationship between comorbidities and kidney disease to improve self management Focusing on goals including: Optimizing blood pressure Anemia management Medication compliance Diet compliance Healthy lifestyle adherence to include flu, pneumonia and hepatitis B vaccines Coordinating referrals as appropriate that may include but are not limited to: o Registered Dietician o Specialty Care o Counseling/Social Worker Achieving optimal collaborative relationships with providers Overcoming barriers to appointment compliance Review of all members who are hospitalized to determine any changes in the program that might have prevented the hospitalization Coordination with PHC UM and Care Transition Coach if any participant is hospitalized Accompanying members to nephrology appointments as indicated If clinically indicated, and if member desires dialysis, working with providers and member to establish early access in preparation for dialysis treatment Outcome Measurement The outcomes for the initial pilot will include comparison of the members participating in the program to a control group consisting of members with stage 4 and 5 chronic kidney disease not on dialysis and not in a high touch case management program in Sonoma, Marin and Yolo counties. The following information will be collected on both the control group and program participants: Member Age Member Gender Member Ethnicity County of residence Line of business Continuous enrollment with a PCP LABS Estimated Glomerular Filtration Rate (eGFR) 0-29 Iron/Total Iron Binding Capacity/Transferrin Saturation (TSAT) Hb and Hct Did member initiate dialysis? (Yes or No) If yes: What was the first date of dialysis? Was the first dialysis started in a hospital or dialysis center? % of patients with a permanent access prior to initiation of dialysis Page 7 % of patients that are in a home treatment modality at initiation of dialysis Number of Inpatient days in the last six months Total cost of care in the last six months Morbidity. In the event of death, members that die will have their costs followed for 6 months after their death, to allow collection of all claims information and to account for decreased costs associated with improved Advanced Care Planning and appropriate use of the POLST form. For members participating in the program the following additional information will be collected: PHC Health Risk Assessment PAM Scores PHQ 2/9 Scores Veterans RAND 12 item Health Survey (VR 12) Scores Medication Compliance Score Percentage of members who have: Had the Advance Care Planning discussion Have an Advance Directive completed Have a POLST completed Member demonstrates education enhancement regarding options for end stage renal replacement modalities of dialysis and transplant Member has active Nephrology involvement prior to initiation of dialysis Percentage of members who plan to go on dialysis Member initiates dialysis with hemoglobin greater than or equal to 11 Percentage of those members for which dialysis access was: Discussed Planned Completed Matured and ready for dialysis Number of Inpatient days in the six months prior, during and after CKD program participation with associated diagnosis and an analysis of whether the admission could have been prevented in any way. Only PHC costs will be included in the outcome measurement Page 8