Preventing Postoperative Pulmonary Complications
advertisement

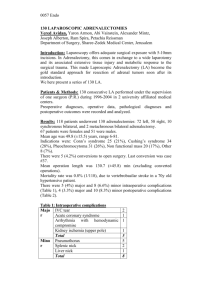
Running head: Preventing Postoperative Pulmonary Complications Preventing Postoperative Pulmonary Complications Danielle D Grant University of New Hampshire 1 Preventing Postoperative Pulmonary Complications Preventing Postoperative Pulmonary Complications Title: In postoperative patients, is including incentive spirometry therapy after surgery more effective in preventing pulmonary complications compared to patients who do not include incentive spirometry therapy? Background and Rationale After surgery, patients are at higher risk for pulmonary complications. Complications can include pulmonary embolism, atelectasis, and pneumonia. Factors leading to these complications are pain and increased bed rest due to immobility. Pulmonary complications occur due to lack of lung inflation after surgery from a change to shallow breathing pattern, prolonged recumbent positioning, and temporary diaphragmatic dysfunction. Clearance of mucus and a decreased effectiveness of coughing are also impaired in postoperative patients which increases the risk of retained secretions. Respiratory physiotherapy after surgery aims to promote maximal inspiration in order to expand the collapsed alveoli and limit secretions. An incentive spirometer is a device used to achieve and maintain maximal inspiration. Other interventions include taking a deep breath and holding it for 3-5 seconds as well as coughing. Intervention is necessary to prevent such complications after surgery, but the clinical efficacy of incentive spirometry is not completely clear. Hospitals are still using this device, yet could coughing and deep breathing produce the same results? Clinical research explores the best implantation in preventing postoperative pulmonary complications. Search Methods During the process of finding evidence, the main database used was CINAHL, provided by the UNH Library. CINAHL includes full text for nursing and allied health journals. Although 2 Preventing Postoperative Pulmonary Complications the search engine Google for basic definitions, all evidence was established from CINAHL. In the search, the key words "postoperative" and "incentive spirometer." The search was limited to English only, articles published since 2000, and full text available. Three citations were identified in establishing my evidence. Inclusion data were articles published after 2000 that focused on postoperative patients from cardiac or abdominal surgeries exploring the use of incentive spirometry to prevent pulmonary complications. Other types of surgeries were not included in this study. Articles that reviewed the effects of arterial blood gas and pulmonary pressure levels without an overview of pulmonary complications were also excluded. Critical Appraisal of the Evidence The first article, “The Effect of Incentive spirometry on Postoperative Pulmonary Complications,” is a systematic review of evidence examining the use of incentive spirometry for the prevention of postoperative pulmonary complications. The search consisted of articles from MEDLINE, CINAHL, HealthSTAR, and Current Contents databases. The review accepted 46 articles that included 26 randomized controlled trials, 9 quasi-randomized controlled trials, 4 cross-over designs, 4 case series, 1 prospective cohort study, 1 retrospective case series, and 1 meta-analysis. Each study was clinically appraised by one of three pairs of team members who each separately completed a Clinical Appraisal Form (CAF). The key areas on the CAF examined information on study purpose, subject characteristic, study design, and results. Each pair met to reach a consensus before presenting to the entire review team for discussion and agreement. The team was unable to accept conclusions in 35 of the 46 papers due to multiple methodolic problems. Of the 11 remaining articles, only one supported the proposed theoretical benefits of incentive spirometry. Due to this, the overall evidence did not support incentive spirometry for preventing postoperative pulmonary complications following cardiac or upper 3 Preventing Postoperative Pulmonary Complications abdominal surgery. Bias was minimized in the study by using an extensive search strategy along with independent review of the validity of each study using a standardized CAF followed by an overall consensus. Three studies evaluated the "short-term" effects of incentive spirometry by looking at a single treatment. They failed to show any benefit on diaphragm function, PaO2, or end-expiratory transpulmonary pressure following cardiac surgery. The other eight studies investigated the effects of incentive spirometry as either a stand-alone treatment or an adjunct to treatment. Four of the studies dealt with postoperative cardiac patients while the other four focused on abdominal surgery. Following cardiac surgery, there is little evidence to support the use of supervised incentive spirometry as either a stand-alone or adjunct therapy. Three of the studies involving abdominal surgery also indicated no support. One supported use of incentive spirometry, however, the authors noted that it included both upper and lower abdominal surgery and there is minimal risk for pulmonary complications in lower abdominal surgery. The limitations of the review were articles retrieved were English only, possibly lacking relevant studies. Also supplements of relevant journals for abstracts not published as peer-reviewed articles were not searched and all authors were not contacted to clarify information not clearly available. The objective of the second article, “Incentive spirometry for prevention of postoperative pulmonary complications in upper abdominal surgery,” was to assess the effect of incentive spirometry compared to no such therapy on all-cause postoperative pulmonary complications and mortality in adult patients admitted for upper abdominal surgery. The study included randomized controlled trials of incentive spirometry in adult patients admitted for any type of upper abdominal surgery. Two authors independently assessed trial quality and extracted data from 11 studies with a total of 1160 patients. Three trials looked at the effects of incentive spirometry 4 Preventing Postoperative Pulmonary Complications with no respiratory treatment. Two trials compared incentive spirometry with deep breathing exercise. Two other trials compared incentive spirometry with other chest physiotherapy. The study found no evidence regarding the effectiveness of the use of incentive spirometry for prevention of postoperative pulmonary complications. There were no language restrictions which allowed for all relevant studies to be examined. The study included patients undergoing laparoscopic procedures which may be a weakness due to the lower risk of pulmonary compilations. Many trials were of only moderate methodological quality and did not report on compliance with the prescribed therapy. The third article discussed a prospective observational study over eight months of patients attending the surgical high dependency unit following open abdomen or open chest surgery. During the first four months, the patients in the hospital received standard chest physiotherapy consisting of five deep breaths. Each breath included an inspiratory hold and sniff followed by a supported cough. The patients in the hospital during the final four months received standard chest physiotherapy with deep breaths being performed via and incentive spirometer rather than inspiratory hold and sniff. There were a total of 111 patients in the no incentive spirometry group and 117 patients in the incentive spirometry group. The average length of stay on the high dependency unit was 4 days in the group without incentive spirometry and 3.1 days with incentive spirometry. According to the study, 17% of patients in the no incentive spirometry group developed postoperative pulmonary complications versus 6% in the incentive spirometry group. Since the study was designed as an observational study, interpretation of complications is open to observer bias. Length of stay should be proportional to the rate of complication, yet there was minimal significant difference in that area. This study concluded that a decreased incidence 5 Preventing Postoperative Pulmonary Complications of pulmonary complications postoperatively is demonstrated when incentive spirometry is added to physiotherapy. Evidence Synthesis From the evidence I have collected on the effectiveness of using incentive spirometry to prevent postoperative pulmonary complications, I have concluded that there is no significant difference. Although incentive spirometry is designed to encourage the patient to take long, slow, deep breaths to increase lung expansion, the evidence does not supportive its clinical efficacy compared to other physiotherapies. There is no evidence signifying that incentive spirometry is harmful to postoperative patients, however, deep coughing and breathing seem to be just as effective. In the first review, the study that supported the use of incentive spirometry also looked at lower abdominal surgeries which already have a lower risk of complications. This may have skewed the data. Although the third study also supported the use of incentive spirometry, the postoperative pulmonary complications was increased by only 11%. It also stated that that physiotherapist were requested to see patients as emergency contacts less often in the incentive spirometry group, but this failed to achieve statistical significance. Overall I do not believe there is enough evidence to support the clinical decision that incentive spirometry significantly lowers the risk of pulmonary complications in postoperative patients. Clinical and Research Recommendations Based on my critical appraisal of the evidence, nursing practice should implement the use of deep breathing and coughing as much as possible during postoperative care. No significant evidence supports the idea that incentive spirometry is more effective in preventing pulmonary complications. This does not, however, determine that it will cause any harmful side effects to the patient. Further research requires trials of high methodological to continue to define any 6 Preventing Postoperative Pulmonary Complications benefits from incentive spirometry. As long as patients are taught the effective method of coughing and deep breathing and encouraged to do so regularly, there risk for pulmonary complications is no greater than those using incentive spirometry therapy. Clinical practices need to be sure correct methods are instituted and performed effectively. 7 Preventing Postoperative Pulmonary Complications References Overend, T. J., Anderson, C. M., Lucy, S., Bhatia, C., Jonsson, B. I., & Timmermans, C. (2001). The Effect of Incentive Spirometry on Postoperative Pulmonary Complications. Chest, 120(3), 971. Guimarães, M., El Dib, R., Smith, A., & Matos, D. (2009). Incentive spirometry for prevention of postoperative pulmonary complications in upper abdominal surgery. Cochrane Database Of Systematic Reviews, (3), doi:10.1002/14651858.CD006058.pub2 Westwood, K., et al. "Incentive Spirometry Decreases Respiratory Complications Following Major Abdominal Surgery." Surgeon (Edinburgh University Press) 5.6 (2007): 339-342. Academic Search Alumni Edition. Web. 11 Dec. 2013. 8