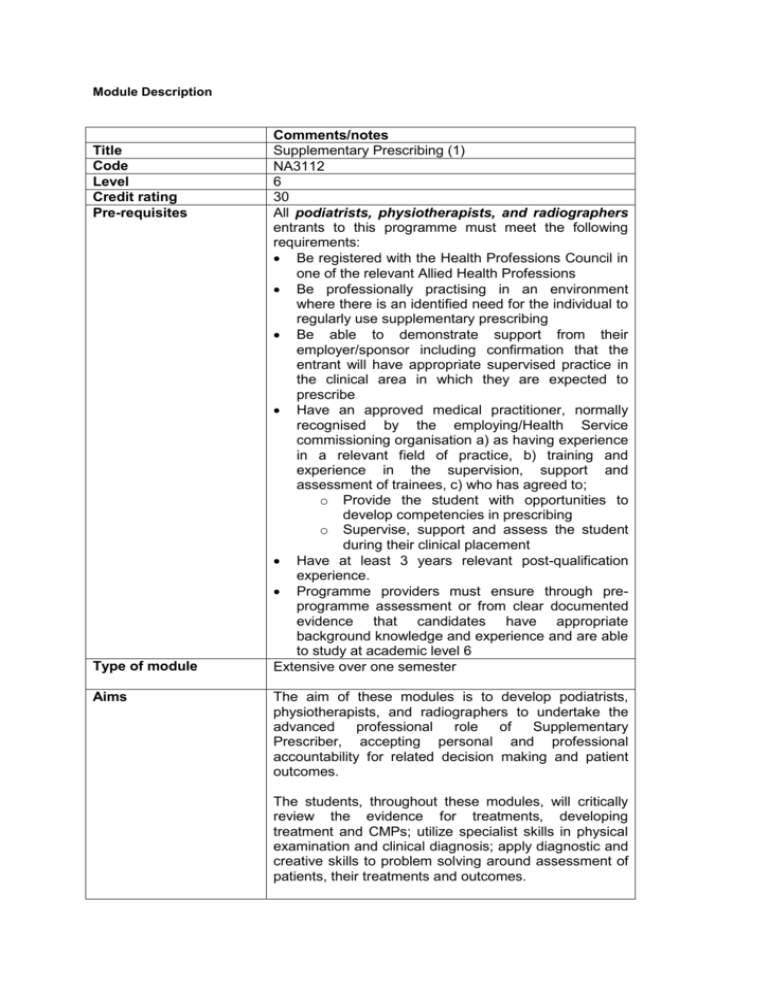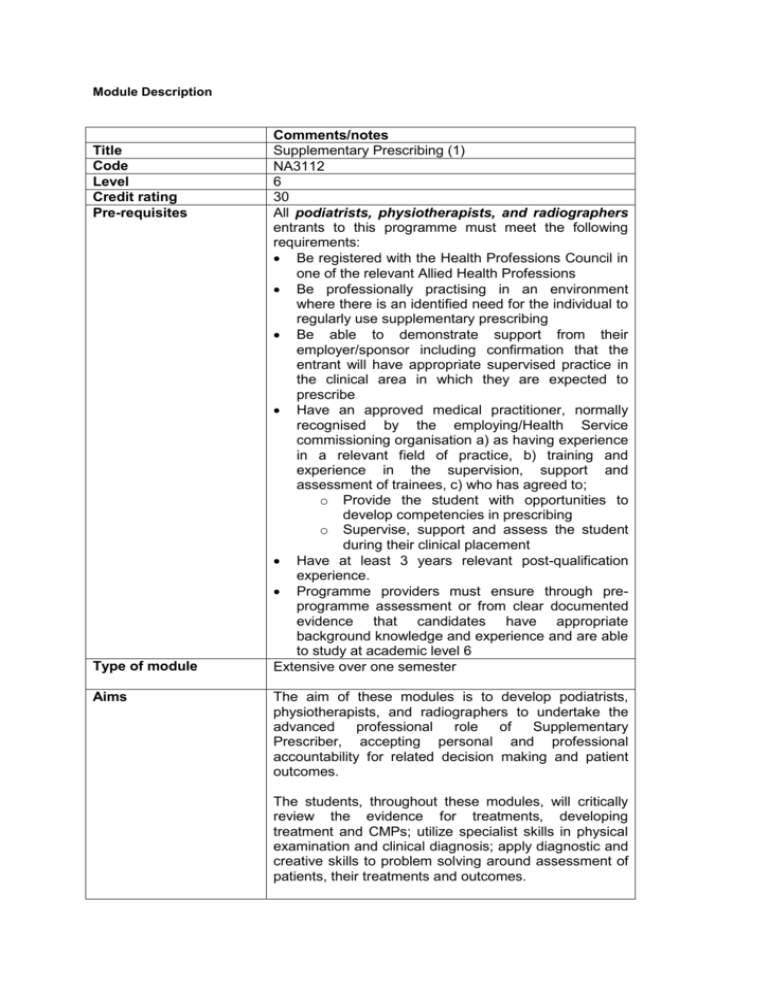
Module Description
Title
Code
Level
Credit rating
Pre-requisites
Type of module
Aims
Comments/notes
Supplementary Prescribing (1)
NA3112
6
30
All podiatrists, physiotherapists, and radiographers
entrants to this programme must meet the following
requirements:
Be registered with the Health Professions Council in
one of the relevant Allied Health Professions
Be professionally practising in an environment
where there is an identified need for the individual to
regularly use supplementary prescribing
Be able to demonstrate support from their
employer/sponsor including confirmation that the
entrant will have appropriate supervised practice in
the clinical area in which they are expected to
prescribe
Have an approved medical practitioner, normally
recognised by the employing/Health Service
commissioning organisation a) as having experience
in a relevant field of practice, b) training and
experience in the supervision, support and
assessment of trainees, c) who has agreed to;
o Provide the student with opportunities to
develop competencies in prescribing
o Supervise, support and assess the student
during their clinical placement
Have at least 3 years relevant post-qualification
experience.
Programme providers must ensure through preprogramme assessment or from clear documented
evidence that candidates have appropriate
background knowledge and experience and are able
to study at academic level 6
Extensive over one semester
The aim of these modules is to develop podiatrists,
physiotherapists, and radiographers to undertake the
advanced
professional
role
of
Supplementary
Prescriber, accepting personal and professional
accountability for related decision making and patient
outcomes.
The students, throughout these modules, will critically
review the evidence for treatments, developing
treatment and CMPs; utilize specialist skills in physical
examination and clinical diagnosis; apply diagnostic and
creative skills to problem solving around assessment of
patients, their treatments and outcomes.
Learning
outcomes/objectives
The module will enable the practitioners to meet the
outcomes specified by the NPC; namely to:
1. understand the responsibility that the role of
Supplementary / Independent prescriber entails, be
aware of their own limitations and work within the
limits of their professional competence – knowing
when and how to refer / consult / seek guidance from
another member of the health care team
2.
develop an effective relationship and
communication, assessing and consulting as
appropriate with patients, carers, other prescribers
and members of the health care team and
understand their roles in the medicines use process
3. describe the patho-physiology of the condition being
treated and recognise the signs and symptoms of
illness
4.
use effectively and interpret common diagnostic
aids e.g. stethoscope, sphygmomanometer
5. select and use diagnostic aids relevant to the
condition(s) for which the practitioner intends to
prescribe, including monitoring response to therapy
6. apply clinical assessment skills to:
inform a working diagnosis
formulate a treatment plan
the prescribing of one or more medicines if
appropriate
carry out a checking process to ensure
patient safety.
monitor response to therapy, review the
working/differential diagnosis and
modify treatment or refer / consult / seek
guidance as appropriate
7.
take a thorough and accurate history, including
medication history (including over-the-counter,
alternative and complementary health therapies) to
(in conjunction with 6) inform a diagnosis and choice
about treatment
8. demonstrate a shared approach to decision making
by assessing patients ‘needs for medicines, taking
account of their wishes and values and those of their
carers when making prescribing decisions
9.
identify and critically appraise sources of
information, access advice and decision support and
demonstrate how they will use them in patient care
taking into account evidence based practice and
national/local guidelines where they exist.
10. recognise, evaluate and respond to influences on
prescribing practice at individual, local and national
levels
11.
prescribe, safely, appropriately and cost
effectively
12.
work effectively within a prescribing partnership
13.
maintain accurate, effective and timely records in
the patients notes and ensure that other prescribers
and health care staff are appropriately informed, and
comply with national guidance as appropriate e.g.
adverse drug reaction reporting
14.
demonstrate an understanding of the public
health issues related to medicines use
15.demonstrate an understanding of the legal, ethical
and professional framework for accountability and
responsibility in relation to prescribing
16.work within clinical governance frameworks that
include audit of prescribing practice (including any
near misses) and personal development
17.participate regularly in CPD and maintain a record of
their CPD activity
18.understand and apply knowledge of drug actions in
prescribing practice
19.develop a clinical management plan within legislative
requirements and develop effective working
partnerships with the Independent Prescriber(s)
(supplementary prescribing only)
Content
On completion the prescriber should demonstrate
concordance with the NPC’s competencies for
Prescribing.
1.
Consultation, decision-making therapy
selection, monitoring of therapy selection, and
referral
Accurate and effective communication and
consultation with professionals, other prescribers,
patients and their carers
Building and maintaining an effective relationship
with patients, parents and carers taking into account
their values and beliefs
Partnership working with the patient including
concordant approach and the importance of
explaining why medication has been prescribed,
side effects and other relevant information to enable
patient choice
Understands own limitations
A knowledge of the range of models of consultation
and their applications
Development and documentation of a treatment or
clinical management plan including referral to the
independent prescriber and other professionals
Principles of diagnosis and the formulation of a
working diagnosis, principles and methods of patient
monitoring, further investigation and referral for
diagnosis.
Management options including non-drug treatment
Autonomous working and decision making within
professional competence
Numeracy and drug calculations•
Chemical and biochemical methods for monitoring
the treatment of the condition(s) for which the
practitioner intends to prescribe on qualification and
responses to results.
Clinical examination skills relevant to the condition(s)
for which the practitioner intends to prescribe.
Recognition and responding to common signs and
symptoms that is indicative of clinical problems. Use
of common diagnostic aids for assessment of the
patient’s general health status; e.g. stethoscope,
sphygmomanometer, tendon hammer, examination
of the cranial nerves.
Assessing responses to treatment against the
objectives of the treatment plan/clinical management
plan
Working knowledge of any monitoring equipment
used within the context of the treatment/clinical
management plan
Identifying and reporting adverse drug reactions
Management options including non-drug treatment
and referral
2. Influences on and Psychology of Prescribing
Patient demand versus patient need including
partnership in medicine taking, awareness of cultural
and ethnic needs
External influences, at individual, local and national
levels.
Awareness of own personal attitude and its influence
on prescribing practice
3. Prescribing in a Team Context
The role and functions of other team members
The responsibility of the supplementary prescriber in
developing and delivering the clinical management
plan.
The professional relationship between independent
and
supplementary
prescribers
and
those
responsible for dispensing
Documentation and the purpose of records in
communicating prescribing decisions to other
members of the team.
Structure, content and interpretation of medical
records/clinical notes including electronic health
records
Interface between multiple prescribers and the
management of potential conflict
The framework for prescribing budgets/cost effective
prescribing, audit and evaluation
The responsibility of the Supplementary and
Independent Prescriber in the development and
delivery of the treatment / clinical management plan
4. Clinical pharmacology and applied therapeutics,
including the effects of co-morbidity
Clinical pharmacology
5.
Pharmacodynamics and pharmacokinetics (including
controlled drugs)
Changes in physiology and drug response, for
example the elderly, young, pregnant or breast
feeding women and ethnicity
Adverse drug reactions (including reporting), drug
interactions (drug and disease) and drug related
morbidity
Patho-physiology of defined conditions for which the
prescriber intends to prescribe.
Selection and optimisation of drug regimen
Natural history and progression of defined conditions
for which the practitioner intends to prescribe.
Impact of co-morbidities on prescribing and patient
management
Evidence-based practice and clinical
governance in relation to prescribing
The rationale for national and local guidelines,
protocols, policies, decision support systems and
formularies – understanding the implications of
adherence to and deviation from such guidance
Local and professional clinical governance
procedures including
Supplementary prescribing in the context of the local
health economy e.g. application of local priorities to
supplementary prescribing, prescribing guidance
produced by PCT prescribing forum, health
economy Area Prescribing Committees and priorities
for health improvement.
Principles of evidence-based practice and critical
appraisal skills
Reflective practice and continuing professional
development – role of self and organisation.
Development and maintenance of professional
knowledge and competence in relation to
condition(s) for which the practitioner intends to
prescribe
Auditing, monitoring and evaluating prescribing
practice
Risk assessment and risk management
Audit and systems monitoring
Analysis and learning from medication errors and
near misses
The Medication Use Process
6.
Legal, policy, and professional and ethical
aspects
Policy context for prescribing
Professional
Ethics and Practice Guidance,
especially in relation to the supply and
administration of medicines
Legal
basis
for
prescribing,
supply
and
administration of medicines
Medicines regulatory framework including Marketing
Authorisation, the use of unlicensed medicines and
“off-label” use.
Application of the law in practice, professional
judgment, liability and indemnity
Maintenance of professional knowledge and
competence in relation to the conditions for which
the supplementary prescriber may prescribe.
Accountability and responsibility to the employer or
commissioning
organisation, awareness of local complaints
procedures
Informed consent with particular reference to
patient’s with learning disabilities, mental illness,
critical illness; those requiring emergency treatment,
and children
Prescription pad security and procedures when pads
are lost or stolen
Writing prescriptions
Record keeping, documentation and professional
responsibility
Confidentiality, Caldicott and Data Protection, and
Freedom of Information
Suspicion, awareness and reporting of fraud or
criminal behaviour, knowledge of reporting and
‘whistle blowing’ procedures
Compliance with guidance arising from the Shipman
inquiry
Professional
competence,
autonomy
and
accountability of Supplementary Prescribing Practice
7. Prescribing in the public health context
Duty to patients and society
Public health policies, for example the use of
antimicrobials and resistance
Inappropriate use of medicines including misuse,
under and over-use
Inappropriate prescribing, over and underprescribing
Patient access to healthcare and medicines
Use of medicines in populations, and in the context
of health priorities
Teaching and learning
strategies
Keynote lectures, self-directed learning, critical
reflection, portfolio, case analysis of treatment
scenarios, group discussion, problem-based learning.
The students will be encouraged to use studentcentral
with electronic learning materials on:
clinical pharmacology
ethics and law in prescribing
skills in consultation and assessment
on-line submission and blogging
Learning support
on-line chat support sessions
Teaching, supervision and support by lecturers and
personal tutors.
Supervision, support and shadowing opportunities by
Designated Medical Practitioner
Reading list
Bickley, L.S. 2009 Bates’ Guide to Physical Assessment and
History Taking. Lippincott Williams & Wilkins.
Brookes, D. & A. Smith. 2006 Non-Medical Prescribing in
Healthcare Practice: a Toolkit for Students and Practitioners.
London: Palgrave.
Beauchamp, T.L. & J.E. Childress. 2009 Principles of
Biomedical Ethics. 6th ed. Oxford: Oxford University Press.
Clinical Evidence. 2003. 9th ed. London: BMJ Publishing.
Courtenay, M & M. Griffiths (eds.) 2005. Independent and
Supplementary Prescribing: an Essential Guide. Cambridge:
Cambridge Press.
Courtenay, M. & Griffiths, M (eds) 2010. Medication safety: an
essential guide. Cambridge University press.
Dale, M.M. & Haylett, D.G. 2009 Pharmacology Condensed
2nd ed. Churchill Livingstone; Elsevier.
Department of Health. 2006. Improving Patients’ Access to
Medicines: A Guide to Implementing Nurse and Pharmacist
Independent Prescribing within the NHS in England. London:
DOH.
Department of Health. 2005. Supplementary Prescribing by
Nurses,
Pharmacists,
Chiropodists/Podiatrists,
Physiotherapists and Radiographers within the NHS in
England. London: DOH.
Dimond, B. 2005. Legal Aspects of Medicines. Quay.
Galbraith A. et al 2007 Fundamentals of Pharmacology 2nd
ed. Pearson Prentice Hall.
Jones, M. & Guatam, N. 2004 The hands-on guide to practical
prescribing. Blackwell.
Kumar, P. & Clark, M. (eds). 2009. Clinical Medicine. 7th ed.
Saunders Elsevier.
Lymn, J., Bowskill, D., Bath-Hextall, F., Knaggs, R. (eds) 2010
the new Prescriber. An integrated approach to medical and
non-medical prescribing. Wiley-Blackwell.
Morgan, R. & Johnson, M. 2000 Pharmacology for podiatrists.
Blackwell Science.
Neal, M.J. 2005 Medical Pharmacology at a glance. 5th ed.
London: Blackwell
Porth, C.M. & Matfin, G. 2009. Pathophysiology: concepts of
altered health states. 7th ed. Lippincott, Williams & Wilkins
Robinson, D. 2002. Clinical Decision-Making, a case study
approach 2nd ed. Lippincott
Swage, T. 2004. Clinical Governance in Health Care Practice.
2nd ed. Butterworth-Heinemann
Assessment tasks
The assessment regulations will conform to the
University of Brighton General Examination and
Assessment Regulations and the rules and regulations
of the Undergraduate Professional Practice Framework.
Competence will be demonstrated through assessment
of both theory and practice. To facilitate this, each
student will maintain a portfolio of assessment and
achievement of the stated learning outcomes. A range
of assessment strategies will be employed to test
knowledge, decision-making and the application of
theory to practice. These are dictated by the NPC and
are listed in the 4 parts as follows:
Examination
(Part A)
Objective Structured Clinical Examination
(OSCE), a systematic examination of practice
within a simulated clinical environment, including
a pass/fail calculation element.
(Part B)
Final examination consisting of 30
multiple choice questions and an unseen written
paper to test pharmacological knowledge,
application to practice and analytical reasoning
(nurses must achieve a minimum 80% pass for
the multiple choice paper, a statutory body
requirement):
Coursework
(Part C)
Clinical Management Plans for the
students’ specific client group
(Part D)
Review of portfolio (to include reflection,
critical incident analysis, case studies etc.,
including a pass/fail calculation element) will
include a record of the satisfactory completion of
a minimum of 12 days or the equivalent (90
hours) of learning experience. The assessment
of practice will be the responsibility of the
prescribing medical practitioner providing
support, teaching and supervision of the student.
This portfolio is designed to provide evidence of
the NPC’s Competencies for Supplementary /
Independent Prescribers.
Each part of the above examination and coursework
elements of the assessment strategies carries an equal
weighting and students must achieve the required
pass or pass mark in each of the components,
individual statutory body requirements apply differently
depending on the profession.
Brief description of
module content and/or
The final mark is calculated from the arithmetic mean of
the mark from the four components (A – D). All 4 parts
of the assessments are marked in accordance to
separate marking criteria for the level of assessment
(6 or 7) that the student has opted to be examined
at. (See appendix 7 for the unseen written examination
marking criteria). Certain elements are also graded pass
or fail independent of the overall mark awarded.
Therefore a pass mark awarded cannot compensate
against a fail element.
This module will enable Supplementary Prescribers to
prescribe Prescription Only Medicines including
aims (maximum 80
words)
Area examination board
to which module relates
Module team
Semester offered, where
appropriate
Site where delivered
Date of first approval
Date of last revision
Date of approval of this
version
Version number
Replacement for
previous module
Field for which module
is acceptable and status
in that field
Course(s) for which
module is acceptable
and status in that
course
School home
External examiner
Controlled Drugs and off-label use in accordance with
an individual patient’s Clinical Management Plan and
the agreement of the medical practitioner and with the
patient’s consent
BSc(Hons) in Professional Practice Under Graduate
Continuing Professional Development AEB, School of
Nursing and Midwifery
Maria Young (Module Leader: Podiatrist)
Penny Lindley: Assistant Head - Continuing Professional
Education, School of Nursing & Midwifery
Kate Barnham: Former Student March 2010 cohort
Independent Prescriber (Respiratory Nurse Specialist)
Inge Bateman: Non-Medical Prescribing Lead & Clinical
Nurse Specialist in Acute Pain Management
Joanne Burgess: Former Student Sept 2006 cohort,
Independent Prescriber (Mental Health Nurse)
Peter Coyne: Information Adviser
Sharon De Goeas: Senior Lecturer (Ethics)
Dr. Les Ellam: Learning Technologies Adviser
Mary Elliott: Independent prescriber, Lead Fracture
Liaison Nurse Specialist, Visiting Lecturer for Physical
Assessment Elements
Sue Oliver: Former Student March 2010 cohort,
Independent Pharmacist Prescriber
Paula Rabin, Director of Radiography, Brighton and
Sussex University Hospitals NHS Trust
Samantha Taylor: Programme Administrator
Stevan Monkley-Poole: Module Lead: Nurses
Greg Scutt: Module Lead: Pharmacists
1 and 2
Falmer
March 2011
Podiatry / Physiotherapy / Radiography
School of Nursing and Midwifery
Dr. Christine Thorp (01/04/2011 to 31/03/2015)