path 29 LO [5-6
advertisement

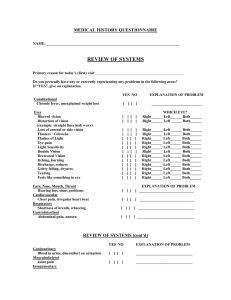
Chapter 29 The Eye, pages 1346-1368 1. In which direction does lacrimal gland inflammation push the eye? Inferiorly and medially, since lacrimal gland is superior and lateral to the eye 2. What are the two most common malignancies of the eyelid? Basal cell carcinoma and sebaceous carcinoma 3. Where does basal cell carcinoma like to strike and what does sebaceous carcinoma resemble? Basal cell carcinoma; targets lower eyelid and medial canthus Sebaceous carcinoma; mimics chalazion, blepharitis, and ocular cicatricial pemphigoid i. Vacuolization of the cytoplasm can help with the diagnosis Which is the only bacterial infection to cause conjunctival scarring? Why is scarring bad? Chlamydia Scarring reduces the number of goblet cells, which means that there is less mucin Even with adequate aqueous tear film, insuficient mucin means that the eyes dry out 4. 5. Where do pinguecula and pterygium originate? What typifies each? Originate at the limbus of the conjunctiva (just next to the cornea) Pterygium is a submucosal growth of fibrovascular connective tissue that migrates onto the cornea; might cause mild astigmatism Pinguecula stays put near the limbus, but can cause an unequal tear film distribution over the cornea, resulting in a dellen (saucer-like corneal depression) 6. What two neoplasms of the conjunctiva are asociated with HPV 16 & 18? What other neoplasm is usually benign? How do melanomas first begin to form? Squamous papillomas and conjunctival intraepithelial neoplasia; indolent course Conjunctival nevi, pigmented splotches that are sometimes inflamed in children Start as primary acquired melanosis with atypia (melanoma in situ)=> conjunctival melanoma i. Extirpate these 7. What is the most likely cause of corneal ulcers? Herpes simplex virus 8. What is bullous keratopathy? Where does copper deposit in Wilson’s disease? Decrease in endoethelial cells=> edema in the corneal endothelium=> Separation of the epithelium (bullous keratopathy) The Descemet membrane, the basement membrane on which the corneal endothelium rests 9. What are the two kinds of corneal disorders? Under which falls band keratopathy? Where does calcific band keratopathy deposit calcium? Why does actinic band keratopathy develop? Degenerations (unilateral and acquired) and dystrophies (bilateral and familial) Band keratopathies = degeneration Bowman layer People exposed to high levels of UV light, therefore it develops on the horizontal 10. What causes keratomalacia? Vitamin A deficiency 11. What is corneal hydrops? In what conditions does it occur? Effusion of aqueous humor through a rupture in the Descemet membrane i. => sudden worsening of vision, sometimes permanent scarring Keratoconus and infantile glaucoma (Haab’s striae) 12. How does Fuchs endothelial dystrophy present clinically (3 features)? Under what circumstance does a similar condition arise? bullous keratopathy & stromal edema, both caused by loss of endothelial cells Guttata: droplike deposits of abnormal basement membrane, which resemble Descemet membrane Following cataract surgery; “pseudophakic bullous keratopathy” 13. What is the major form of stromal dystrophy? What mutation causes stromal dystrophies like lattice, granular, and Avelino dystrophies? Macular corneal dystrophy is a misnomer, involving the cornea and not the macula TGFB1 mutations disrupt the folding of keratoepithelin and lead to various depositions 14. When do inflammatory reactions to lens material occur? What do you call it when the lens material liquefies entirely? What is its complication? After surgery or after traumatic rupture Morgagnian cataract Phacolysis: liquefied lens seeps throught the lens capsule, clogs the trabecular meshwork, and causes secondary open-angle glaucoma 15. What occular complication can happen with long-term high dose glucocorticoid therapy? cataracts 16. What does particulate matter from ghost cells (RBCs after trauma), pigment, exfoliation, or melanoma cause when the trabecular meshwork is clogged? What gene mutation is associated with the primary version of this condition? [Benedum] By the way, the trabecular meshwork is where aqueous humor is reabsorbed Secondary open angle glaucoma MYOC => primary open angle galaucoma 17. When will you observe glaukomflecken (subscapular opacities) by slit lamp? Be specific! When is this condition likely to occur? Primary angle closure glaucoma i. Glaucomflecken are caused by pressure-induced damage to the lens epithelium Most often found in people with hyperopia (shallow anterior chamber) 18. What is a common cause of secondary angle closure glaucoma? Neovascularization which occludes the canal of Schlemm, esp. necrotic tumors 19. What problem does anterior synechiae cause? What about posterior synechiae? Elevation of intra-ocular pressure; anterior synechiae is adherence of iris + trabecular meshwork i. I don’t think it always causes glaucoma?? Fibrous metaplasia of the lens epithelium, resulting in anterior subcapsular cataract 20. What form of uveitis has the “candle wax dripping” sign on biopsy? What is this condition a complication of? What are two microbes that can cause uveitis? Which form of uveitis develops after penetrating injury? Granulomatous uveitis i. Complication of scarcoidosis Pneumocystis carinii, Toxoplasmosa gondii Sympathetic opthalmia; “sympathetic” because retinal antigens also cause blindness in the untraumatized eye 21. What is the most common intra-ocular malignancy in adults? Where/How does it like to metastasize? Uveal melanoma i. Arise w/o a precursor; it is very rare for uveal nevi to progress to melanoma Hematogenously to the liver 22. How do hemorrhages in the nerve fiber layer of the retina appear? How about in the external retinal layers? What does rhegmatogenous mean in regards to retinal detachment? Horizontal “flame” streaks dots = Full thickness retinal tear 23. What are some occular signs of hypertension? How do focal choroidal infarcts from malignant hypertension appear clinically? Flame streaks, cotton- wool spots, arteriolar narrowing, and hard waxy exudates Elschnig pearls; may be a warning sign or retinal detachment 24. What are the two kinds of diabetic retinal vasculopathy? What other manifestations are there? Background: thickened vessel basement membranes, microaneurysms=> macular edema, exudates, angiogenesis within retina (“intraretinal microangiopathy”) Proliferative: angiogenesis on the optic nerve head (“neovascularization of the disk”) or the surface of the retina (“neovascularization elsewhere”) i. Can cause anterior synechiae and glaucoma Microaneurysms and retinal detachment (late) 25. Besides the angiogenesis in Retinopathy of prematurity, what else can happen? The macula can be dragged laterally because the lateral aspect of the retinal periphery is incompletely vascularized in premies 26. What signs are visible in the retina of a person with sickle cell anemia? Why do they happen? Salmon patches, iridescent spots, black sunburst lesions, angiogenesis, and sometimes hemorrhage which leads to retinal detachment Root cause is occlusion due to low oxygen tension within vessels of the retinal periphery 27. What are Hollenhorst plaques? What does the retina look like when blood supply stops suddenly? What does a total occlusion of the central retinal artery look like? Fragments of atherosclerotic plaques that lodge in the retinal circulation (emboli) Retina swells and becomes opaque Cherry-red spot; this is unsurprisingly why it appears inTay-Sachs and Niemann-Pick 28. How do pathologists classify age-related macular degeneration? Which has drusen? Non-neovascular (atrophic/dry): diffuse deposits in the Bruch membrane (drusen); loss of vision is more severe Neovascular (exudative/wet): what it sounds like; occasional massive hemorrhage 29. What are the clinical signs of retinitis pigmentosa (4)? Both rods and cones are lost to apoptosis, leading to night blindness an loss of central visual acuity Optic nerve head atrophy (“waxy pallor”) and constriction of retinal vessels 30. What is the most common primary intra-ocular malignancy of children? Signs? Retinoblastsoma i. Flexner-Wintersteiner rosettes and fleurettes in well-differentiated tumors 31. What are the signs of normal-tension glaucoma? Divide it up by signs in children (2) and adults (2): Diffuse loss of ganglion cells and thining of the retinal nerve fiber layer In children, buphthalmos (diffuse swelling) and megalocornea In adults, focal thinning of the sclera and staphyloma (uveal tissue lining ectatic sclera) (??) 32. What does optic neuritis mean? A loss of vision caused by demyelinization of the optic nerve 33. What is phthisis bulbi? The end stage eye; both atrophic (small) and internally disorganized i. NOTE: Doesn’t include congenital micropthalmia Ciliochoroidal effusion (between sclera + choroid or ciliary body + choroid), cyclitic membrane, chronic retinal detachment, intra-ocular bone formation, thick sclera—especially posteriorly