DMR APAP Metabolic Phenotyping COEN FINAL
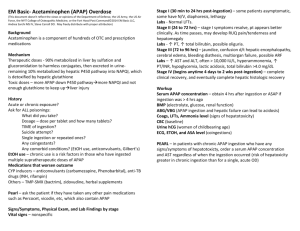
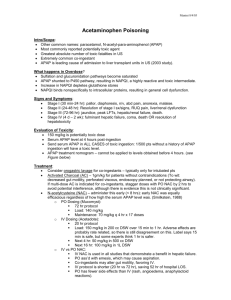
advertisement

Title: Metabolic phenotyping applied to pre-clinical and clinical studies of acetaminophen metabolism and hepatotoxicity Author: Muireann Coen1 1 Computational and Systems Medicine, Department of Surgery and Cancer, Faculty of Medicine, Imperial College London, London SW7 2AZ, UK m.coen@imperial.ac.uk Tel: +44 207 5941179 Word Count: 9145 (minus abstract and references) Keywords: Metabolic phenotyping, metabolomics / metabonomics, acetaminophen, NMR spectroscopy, liquid chromatography-mass spectrometry 1 Abstract Acetaminophen (APAP, paracetamol, N-acetyl-p-aminophenol) is a widely used analgesic that is safe at therapeutic doses but is a major cause of acute liver failure (ALF) following overdose. APAP-induced hepatotoxicity is related to the formation of an electrophilic reactive metabolite, N-acetyl-p-benzoquinone imine (NAPQI), which is detoxified through conjugation with reduced glutathione (GSH). One method that has been applied to study APAP metabolism and hepatotoxicity is that of metabolic phenotyping, which involves the study of the small molecule complement of complex biological samples. This approach involves the use of high-resolution analytical platforms such as NMR spectroscopy and mass spectrometry to generate information-rich metabolic profiles that capture both endogenous and xenobiotic metabolites that reflect both genetic and environmental influences. Data modeling and mining and the subsequent identification of panels of candidate biomarkers are typically approached with multivariate statistical tools. We review the application of multi-platform metabolic profiling for the study of APAP metabolism in both in vivo models and humans. We also review the application of metabolic profiling for the study of endogenous metabolic pathway perturbations in response to APAP hepatotoxicity, with a particular focus on metabolites involved in the biosynthesis of GSH and those that reflect mitochondrial function such as long-chain acylcarnitines. Taken together, this body of work sheds much light on the mechanism of APAP-induced hepatotoxicity and provides candidate biomarkers that may prove of translational relevance for improved stratification of APAPinduced ALF. 2 Introduction Metabolic phenotyping is a recently invented term to cover the ‘top-down’ systems level study of low molecular weight metabolites and is an inclusion of earlier metabolic profiling methods generally grouped as metabonomics or metabolomics. Metabolic phenotyping enables perturbations from metabolic homeostasis to be followed temporally and in integrated cellular matrices, examining effects arising from environmental factors such as drugs, diet or lifestyle or from modulated genetic backgrounds. Ultimately, this approach enables the generation of unique metabolic phenotypes that hold a wealth of mechanistic biochemical information and can be integrated with parallel ‘omics’ data. The field of metabolic phenotyping has endless potential applications and to date has been widely applied in disease diagnosis and personalized healthcare, large-scale molecular epidemiological studies, preclinical and clinical pharmacology and toxicology, in addition to improving the understanding of complex interactions between the host and the gut microbiome, to name but a few. High-resolution Analytical Platforms The earliest applications of metabonomics were centered in the field of toxicology and utilized high-field 1 H nuclear magnetic resonance (NMR) spectroscopy and pattern recognition approaches to identify unique metabolic phenotypes that reflected the target organ and site of toxicity (Nicholson et al., 2002, Nicholson et al., 1999) A major advantage of the approach lay in the ability to acquire metabolic profiles of biofluids such as urine across time, enabling the temporal systemic response to a toxin to be followed reflecting onset, progression and potentially recovery from toxic insult. Sample preparation is minimal for NMR spectroscopic analysis of biofluids, and detailed protocols describing how to conduct this type of analysis are available (Dona et al., 2014, Beckonert et al., 2007). One-Dimensional (1D) 1H NMR spectroscopic experiments are applied to generate spectra that detect metabolites from diverse chemical classes and that, depending upon the experimental parameters used to acquire them, are inherently quantitative. Typically, up to 100 metabolites can be assigned from a high-resolution biofluid 1 H NMR spectrum. The information present in these spectra enables the simultaneous identification of endogenous and xenobiotic metabolites. Two-dimensional (2D) NMR spectroscopic experiments, such as homo-nuclear 1H-1H correlation spectroscopy (COSY) and total correlation spectroscopy TOCSY and hetero-nuclear 13 C-1H multiple bond correlation 3 (HMBC) and heteronuclear single quantum correlation (HSQC), are employed to aid in structural identification. In addition, databases of standard metabolites are available commercially (Bruker S-BASE, Chenomx) and from online resources such as the biological magnetic resonance biobank (BMRB) and the human metabolome database (HMDB) to aid in structural identification. High-resolution magic angle spinning (MAS) NMR represents a means to generate ‘solution-state like’ spectral profiles from intact tissue samples (typically 50 mg), such as clinical biopsies (Beckonert et al., 2010). This has been shown to be a powerful, non-destructive tool for generating high-resolution metabolic profiles from tissues such as liver, kidney or brain. Such spectra are complementary to biofluid profiles and have found application in rapid diagnosis and staging of colorectal cancer (Jimenez et al., 2013, Mirnezami et al., 2014). Recently, the application of liquid chromatography and ultra-performance liquid chromatography coupled with mass spectrometry (UPLC/LC-MS) in metabolic profiling studies has rapidly increased. Mass spectrometry-based analysis offers a complementary approach to NMR with higher (albeit structurally dependent) sensitivity and hence broader coverage of the metabolome albeit with the need for stringent quality control strategies to ensure reproducibility and reliability of data. Protocols for untargeted approaches that attempt to cover the widest metabolome in both biofluids and tissues are now available, and detail the inclusion of suitable quality control strategies (Want et al., 2010b, Want et al., 2013, Dunn et al., 2011). Typically, more than 5000 metabolic features will be detected in a single biofluid spectrum generated from a UPLC-quadrupole time-of-flight (QTOF)-MS platform. The assignment of metabolic structures to these features can be both challenging and time-consuming and involves the generation of MS/MS fragmentation data, derivation of empirical formulae from accurate mass measurements and comparison with authentic standards and databases. For profiling the weakly polar and non-polar metabolic complement of urine reversed-phase liquid chromatography (RP-LC), usually obtained via gradient separations on C18-bonded silica stationary phases, is typically applied. Hydrophilic interaction chromatography (HILIC) has been applied to provide coverage of the more polar urinary metabolites, as chromatographic retention of polar compounds is improved in this mode of separation compared to RP-LC. In addition, metabolic profiling approaches also include targeted LC-MS methods that focus on a particular class of analyte, for example bile acids (Want et al., 2010a) or urinary steroid hormones (Dai et al., 2012) and often provide the means of rapid identification and quantification of metabolites with stable-isotope labeled standards. The stability and reproducibility of a UPLC-TOF-MS platform for urinary 4 metabolic profiling was assessed by Benton et al. in a study of inter-site (n=3 laboratories) and intra-site reproducibility which utilized stable isotope labeled metabolites and pooled control human urine (Benton et al., 2012). This study showed good platform reproducibility with coefficients of variation (CVs) of less than 18% across ionization modes and sites and displayed excellent between-site reproducibility of 0.96 and 0.98 for positive and negative ionization modes respectively. A schematic of a typical experimental work-flow for UPLC-MS based analysis of urine together with the data analysis strategy is provided in Figure 1 adapted from (Want et al., 2013) Alternative analytical platforms such as gas chromatography (GC) and capillary electrophoresis (CE) coupled to MS are also widely used in metabolic profiling research, and are detailed in the following review articles and experimental protocols (Chan et al., 2011, Dunn et al., 2011, Ramautar et al., 2011, Ramautar et al., 2014). Metabolic Profiling and Preclinical Toxicology An exemplar for the application of metabolic profiling in the field of preclinical toxicology is provided by the consortium for metabonomic toxicology (COMET) project. COMET evaluated the role of metabolic profiling in preclinical toxicity studies, primarily through NMRspectroscopic based profiling of biofluids for a diverse set of toxins and treatments, with a focus on renal toxins and hepatotoxins (n=150) (Lindon et al., 2005, Lindon et al., 2003). NMR-based spectroscopic analysis of split urinary samples from a study of hydrazine toxicity demonstrated that the platform was highly analytically reproducible and robust between two independent laboratories (Keun et al., 2002). In addition, the COMET consortium project database led to the generation of an expert system for prediction of the toxicity of novel compounds based on urinary 1H NMR spectroscopic profiles (Ebbels et al., 2007). The biobank and metabonomic database generated through this work represents a significant resource for data mining and future mechanistically-driven studies. The second phase of the COMET consortium project (COMET-2) applied a mechanistic approach for the study of a model renal toxin and a hepatotoxin; namely bromoethanamine and galactosamine, respectively. This involved the application of multiple analytical platforms to profile biofluids, tissue extracts and intact tissues from preclinical models with a focus on understanding inter-individual variability in response and protective mechanisms together with the use of stable isotope labeled studies to explore xenobiotic metabolism (Coen, 2010, Shipkova et al., 2011). The application of 1H NMR spectroscopy for large-scale urinary metabolic profiling in 5 molecular epidemiology studies has also been tested and shown to be highly reproducible and robust with respect to inter-site studies and displayed excellent analytical stability in terms of inter- and intra-day variability (Dumas et al., 2006). Multivariate statistical modeling Statistical treatment of the complex data generated in metabolic phenotyping studies depends largely on the study design, however such treatment typically involves application of multivariate statistical tools to identify panels of discriminatory metabolites associated with the biological outcome of interest, such as disease status or drug intervention. Data is also often reduced to single candidate biomarkers and associations with an outcome of interest assessed through univariate statistical methods. However, this approach is limited by the assumption that variables/metabolites are independent and fails to utilize the potential of a multivariate signature in identifying a panel of metabolites (rather than a single metabolite) with high sensitivity/specificity and predictive power. Multivariate regression tools commonly applied include principal components analysis (PCA), partial least squares (PLS) and orthogonal partial least squares regression and discriminant analysis (OPLS/O-PLS-DA). PCA is an unsupervised approach (no a priori class information) that reduces the high dimensionality of the data and enables inherent clusters within the data, together with potential outliers, to be rapidly identified and visualized. Supervised approaches include PLS which enables variance in the spectral data to be modeled with class membership and hence, simplifies the identification of discriminatory metabolites of relevance to the outcome. Chemometric modeling of metabolic profiling data have recently been summarized and reviewed in depth in the following publications. (Madsen et al., 2010, Trygg et al., 2007) Application of metabolic profiling to study APAP metabolism and excretion In this review, acetaminophen (APAP, N-acetyl-p-aminophenol, paracetamol) is used as an exemplar to detail the application of metabolic profiling for the study of xenobiotic metabolism and toxicity and to highlight the experimental approach. The literature reviewed herein spans three decades of research, reflecting technological and methodological advances and continued generation of novel data of mechanistic and translational relevance. 6 The metabolic phenotyping approach that is outlined is equally applicable to the study of others drugs, therapies or interventions. APAP is a widely used analgesic and anti-pyretic agent that is safe at therapeutic doses. However, APAP is the most common cause in the USA and Western Europe of acute liver failure (ALF) as a result of both intentional and unintentional overdose (Bernal et al., 2010, Bernal et al., 2013, Lee, 2012). The majority of APAP is glucuronidated in the liver, a phase II conjugation reaction catalyzed by UDP-glucuronosyltransferases (UGTs). Glucuronidation of APAP accounts for about 50-70% of the dose with subsequent urinary excretion of the conjugate. In addition, about 25-35 % of APAP is hepatically sulfated by sulfotransferase enzymes and then also excreted in urine. APAP is also metabolized via cytochrome P450 enzymes (primarily CYP2E1 in humans) to the reactive electrophilic oxidizing agent, N-acetylpara-benzoquinone imine (NAPQI) (Dahlin et al., 1984, Jollow et al., 1973). It is this route of metabolism that is believed to represent the hepatotoxic liability of APAP via the bioactivation of the drug. NAPQI is detoxified through conjugation with GSH, a reaction that occurs both spontaneously and enzymatically via glutathione-S-transferase (GST) to form APAP-GSH. The APAP-GSH conjugate is further metabolized to an N-acetyl L-cysteinyl conjugate (APAP-NAC), a cysteinyl (APAP-CYS) and cysteinyl-glycine conjugate (APAP-CG). A large fraction of APAP-GSH is excreted in the bile together with a mixture of the thiolcontaining derivatives, which are also excreted in urine. A scheme which summarizes the hepatic metabolism of APAP is presented in Figure 2 (Nelson, 1982). One of the first studies to apply 1H NMR spectroscopy to quantify the urinary excretion of APAP and its metabolites, enabled rapid identification of APAP and its glucuronide (APAP-G), sulfate (APAP-S), N-acetyl-L-cysteinyl (APAP-NAC), and L-cysteinyl (APAP-Cys) metabolites (Bales et al., 1984b). The temporal excretion of APAP and its metabolites were quantified in healthy human subjects and showed that the mean 24 hour excretion as determined by 1H NMR reflected 77.3% of the dose (a single therapeutic 1g dose). In addition, the authors described simultaneous profiling of the excretion of a range of additional endogenous urinary metabolites that included creatinine, citrate, hippurate, and sarcosine. This pioneering work outlined the future potential of the approach to simultaneously profile both endogenous and xenobiotic metabolites. 1H NMR spectroscopy was also applied to study both urine and plasma from subjects who had taken a therapeutic dose or an overdose (fatal and non-fatal) of APAP (Bales et al., 1988). The ratio of glucuronide to sulfate conjugates 7 was greatly elevated in overdose cases, as were levels of APAP-NAC and APAP-Cys, reflecting increased detoxification of NAPQI. Perturbations in endogenous metabolites including elevation of numerous amino acids were also simultaneously identified and believed to reflect hepatic damage and impairment of deamination and transamination processes. Representative 600 MHz 1H NMR spectra of an aqueous-soluble liver extract from a control (vehicle-treated) and APAP-treated mouse at 2-hours post-treatment (C57BL/6, 300 mg/kg, ip) are provided in Figure 3 (unpublished data). This representative example demonstrates the high metabolic-information content of a typical 1D 1H NMR spectrum and displays the parallel assignment of both endogenous and xenobiotic metabolites (colored in red for APAP). The study of the preclinical in vivo metabolism of APAP has also been approached with the use of a UPLC-MS platform that enabled the urinary excretion of APAP and its major metabolites to be followed in the rat (oral gavage with 400, 1600 mg/kg) and showed the correlation of levels of the N-acetyl-L-cysteine conjugate (APAP-NAC) with toxic outcome as determined from clinical chemistry and histopathology. (Sun et al., 2009) Fractionation of complex biofluid samples to remove interfering or potentially confounding metabolites from the metabolite/s of interest has also been successfully applied to aid in the characterization of drug metabolites in biofluids, typically through the use of solid phase extraction chromatography (SPEC). The utilization of SPEC provides a separation step leading to generation of ‘cleaner’ fractions that can be profiled and those that contain metabolites of interest can be further concentrated to improve sensitivity of the NMR analysis. This approach has been applied to characterize drug metabolites in human urine, including APAP in addition to ibuprofen, aspirin, oxpentifylline and naproxen (Wilson and Nicholson, 1988). Furthermore, hyphenated analytical platforms have been applied to characterize the urinary excretion of APAP and its metabolites. Applications have included the direct coupling of reversed-phase high performance liquid chromatography (RP-HPLC) with high-field NMR spectroscopy that incorporated gradient HPLC elution and direct acquisition of both oneand two-dimensional NMR spectroscopic data in stopped-flow mode (Spraul et al., 1994). This approach was useful for rapid detection of APAP and its major metabolites in human urine, rat urine and rat bile and to be widely translatable to the identification of drug metabolites, for example those containing a UV chromophore. In addition, the hyphenation of NMR, HPLC and ion-trap mass spectrometry was achieved in continuous-flow mode and 8 applied to study the excretion of APAP in human urine. This approach enabled the unequivocal detection of urinary APAP-G and APAP-S, together with endogenous metabolites such as phenylacetylglutamine (Shockcor et al., 1996). This hyphenated analytical approach was extended to incorporate the use of a cryo-flow probe to couple LCMS and NMR and improve the NMR limit of detection (Spraul et al., 2003). The cryogenic cooling of the NMR radio-frequency coils and electronics greatly increases the signal to noise (S/N) ratio and hence allows for analysis of much lower sample volumes (for example, 100 l of urine) resulting in the detection of many minor APAP metabolites that would otherwise be below the limit of detection. The hyphenation of analytical platforms also demonstrated the complementarity of NMR and MS, for example in the characterization of ‘NMR-silent’ APAP metabolites by MS (Spraul et al., 2003, Shockcor et al., 1996). The hyphenation of LCSPE-NMR-MS was also applied to the study of a minor human urinary APAP metabolite that was unequivocally identified as the ether glucuronide of 3-methoxy-acetaminophen. (Godejohann et al., 2004) 1 H and 2H NMR spectroscopy has also been applied to study the metabolism and excretion of APAP in rat, using APAP with a stable-label incorporated into the acetyl group as C2H3 or 13 CH3 (Nicholls et al., 1995). The introduction of these labeled acetyl groups enabled the extent of deacetylation followed by reacetylation (“futile deacetylation”) to be determined. The 13C-labelled form was included in the study for comparison of the influence of kinetic isotope effects on the extent of deacetylation, as in general smaller kinetic isotope effects are seen with 13C-labelled compounds than with 2H-labelled compounds. When the recovery of the labeled-APAP metabolites was ascertained, excretion of the metabolites of the deuterated-APAP form was found to be lower than that of the 13C-labelled version, which may have been a reflection of deuterium isotope effects on the disposition of the drug. Thus, the excretion and recovery of 13CH3-APAP and its metabolites as calculated from 1H NMR spectroscopic analysis was 100% while that of the 2H3 form was about 61 %. This study revealed that the extent of futile deacetylation (deacetylation followed by reacetylation) of APAP in the rat was far higher than previously thought and provided a means of assessing this pathway which was believed to be relevant with respect to induction of nephrotoxicity by 4-aminophenol (deacetylated APAP). This elegant isotope exchange study was further extended through direct coupling of NMR with HPLC and through use of a double-labeled acetyl group: 13CO-13CH3. The level of futile deacetylation was characterized for the sulfate and, following an SPE step and HPLC-NMR analysis for the glucuronide and was found to be 9 approximately 9% for each metabolite. The work was also translated to study the futile deacetylation of each conjugated metabolite in human (ca. 1-2%) (Nicholls et al., 1997). LC-NMR-MS was also applied to study glutathione GSH conjugation of NAPQI, and identified 2’-GS-APAP and 3’-GS-APAP as the major conjugates together with a novel labile ipso adduct. This was a mechanistically relevant finding as the ipso adduct was shown to reduce back to NAPQI and potentially migrate from its site of formation and interact with other cellular compartments with the liability to oxidize or covalently bind protein thiols (Chen et al., 1999). An LC-MS based approach was also applied to study APAP metabolism and toxicity in CYP2E1-null mice and wild-type mice, with resistance to APAP observed in the null mice on the basis of serum aminotransferase activities and blood urea nitrogen levels (Chen et al., 2008). The contribution of CYP2E1 to APAP metabolism was delineated from this study design, which unexpectedly revealed that CYP2E1 contribution to APAP metabolism decreased as the dose administered increased. The simultaneous measurement of hepatic GSH and hydrogen peroxide enabled assessment of the oxidative stress associated with the toxic response. Novel metabolites of APAP were determined in wild-type mice that included; 3-methoxy-APAP glucuronide and S-(5-acetylamino-2-hydroxyphenyl)mercaptopyruvic acid (formed by renal APAP-CYS transamination), 3,3'-biacetaminophen (a dimer of APAP), and a benzothiazine compound (originating from deacetylated APAP). These novel minor metabolites provided mechanistic insight into APAP-induced toxicity as they were associated with dose, time and genotype. This study represented a powerful combined application of genetically modified animals and metabolic profiling to identify novel minor metabolites of mechanistic relevance with the potential to serve as biomarkers. In addition, LC-MS-based metabolomic approaches have been used to screen for reactive metabolites through identification of conjugates formed in ‘trapping’ experiments with nucleophiles such as GSH (Li et al., 2011). This approach was applied to study APAP in human liver microsomes (HLMs) that contained cytochrome P450 enzymes and the presence or absence of NADPH and trapping agents such as GSH, semicarbazide and potassium cyanide. Supernatants from the incubations were fractionated using SPEC and analyzed by UPLC-TOFMS. In parallel, mice were treated with vehicle or 300 mg/kg APAP (ip, n = 4), the livers were collected 30 minutes post-treatment and aqueous soluble liver extracts were prepared for UPLC-TOF-MS analysis. The APAP and GSH trapping experiment in HLMs identified four conjugated metabolites, one of which was a ‘novel GSH-trapped reactive metabolite’, that reflected conjugation of deacetylated APAP with GSH (PAP-GS). Characterization of the in 10 vivo liver extracts also showed increased levels of the major APAP-GSH conjugate (3’ position) and lesser levels of the PAP-GS conjugate, albeit with the limitation that this was not quantified nor identified in the loadings S-plot. The authors also applied this approach to study reactive metabolites of pulegone and clozapine (Li et al., 2011). Additional approaches to characterize complex drug metabolism signatures whilst avoiding analytical separation of the mixture components have included statistical total correlation spectroscopy (STOCSY), originally described in an application to large-scale human molecular epidemiology studies (Cloarec et al., 2005). STOCSY has proved to be powerful in structural elucidation and in enhancing information recovery from complex metabonomic analytical datasets. The application of STOCSY to 1D 1H NMR metabolic profiles of human urine enabled the separation of APAP-derived xenobiotic signatures through the generation of statistical connectivities based on the covariance of spectral resonances in independent 1D spectra (Holmes et al., 2007). The STOCSY approach is demonstrated in Figure 4 where the correlation matrix for a 1-dimensional dataset is generated from a single data point (driver peak), in this case for D-3-hydroxybutryate. The highest correlations are identified between resonances from the same molecule and lesser correlations are observed for additional drug metabolites and endogenous metabolites in what could be termed ‘pathway’ connectivities. STOCSY has rapidly found new application, for example in the analysis of heteronuclear data such as 1H-31P and 1H-19F data (Keun et al., 2008, Coen et al., 2007), for uncovering intra- and inter-metabolite relationships in iterative STOCSY (Sands et al., 2011), and for the study of reaction kinetics as exemplified in acyl migration reactions of 1-beta-O-acyl glucuronides (Johnson et al., 2008). A comprehensive review of the myriad of STOCSY-related tools and applications in metabolic profiling and systems medicine has been provided (Robinette et al., 2013). It is likely that the continued development and application of STOCSY holds significant potential in enhancing the study of drug metabolism and systems toxicology in the context of improving information recovery from metabolic profiling datasets. Application of metabolic profiling to the study of the endogenous metabolic consequences of APAP administration Metabolic profiling has also been applied to study the endogenous metabolic consequences of APAP administration in order to further explore and elucidate the mechanism of APAPinduced toxicity. In addition, the potential this approach has for identification of a novel panel of biomarkers that would ultimately prove of translational relevance for the clinical 11 setting and prediction of prognosis with respect to APAP-induced ALF is undergoing exploration. A review of the most-noteworthy literature with respect to understanding APAP-induced endogenous metabolic perturbations and identification of novel biomarkers in both pre-clinical and clinical studies is provided below. Early pre-clinical application of untargeted metabolic profiling Following on from the early work described above (Bales et al., 1988, Bales et al., 1984a, Bales et al., 1985, Ghauri et al., 1993), the application of NMR-based metabonomics to comprehensively profile the systems-wide endogenous metabolic consequences of APAP administration was first reported by Coen et al., (Coen et al., 2003). This approach involved an integrated systems level approach and was anchored with traditional clinical chemistry and histopathological assessment. The study design encompassed treatment of mice (Alderley Park-1) with differential doses of APAP (0, 50, 150 mg/kg, intra-peritoneal) and terminal time-points of 15, 30, 60, 120 and 240 min post-treatment (Coen et al., 2003). Magic angle spinning (MAS) NMR was applied to study intact liver tissue (ca. 10 mg) as this technique enables the acquisition of high-resolution NMR spectroscopic data which is comparable to solution-state NMR and also non-destructive (Beckonert et al., 2010). In parallel, metabolic profiles were acquired for plasma and both aqueous and lipid-soluble hepatic extracts. The metabolic consequences of APAP administration were determined from both time- and dose-dependent PCA multivariate models. Clinical chemistry and histopathology enabled ‘gold-standard’ assessment of hepatic damage induced by APAP, which was anchored with the metabolic phenotype data. 1H NMR profiles revealed the detection of APAP, APAP-S, APAP-G and APAP-NAC in the plasma spectra and APAP-G in spectra of intact liver tissue and aqueous soluble liver extracts. Integration of the multicompartment data revealed a general perturbation of energy metabolism, as reflected by elevated triglyceride levels in liver and plasma. 1H and 31P NMR profiles of lipid soluble tissue extracts enabled the detailed study of lipid species that spanned mono- and polyunsaturated fatty acids, cholesterol and phospholipids such as phosphatidylethanolamine and phosphatidylcholine. In response to APAP an increase in hepatic monounsaturated fatty acids was observed, suggestive of impairment of mitochondrial oxidative phosphorylation. The level of polyunsaturated fatty acids decreased, suggestive of increased -oxidation activity of peroxisomes which may have reflected a compensatory response to counteract depleted energy levels. Histopathological assessment revealed APAP-induced generation of 12 mega-mitochondria that were reported to be ATP depleted, supportive of metabolic perturbations in energy metabolism. Reduced hepatic glycogen and glucose were observed together with increased lactate, suggestive of increased rates of glycogenolysis and glycolysis. 31 P NMR spectroscopy of the lipid soluble tissue extracts indicated depletion of all phospholipidic species, and an increase in the phospholipid degradation products, choline and phosphocholine were observed in the aqueous-soluble liver extracts. The degradation of phospholipids may have reflected an increase in the activity of hepatic phospholipase, an inhibition of enzymes involved in phospholipid synthesis or APAP-induced free radical damage or lipid peroxidation. Elevation of numerous hepatic amino acids suggested perturbation of transamination reactions as a result of impairment of the citric acid cycle. Transcriptomic data was also generated in parallel for this study and integrated with the metabonomic data and many of the significantly differentially expressed genes were found to correlate biologically with the metabonomic changes, suggesting APAP-induced global energy failure. For example, down-regulation of lipoprotein lipase mRNA, which is responsible for hydrolysis of triglycerides and very-low-density lipoprotein, correlated with the observed metabonomic increase of hepatic triglycerides. (Coen et al., 2004) The COMET consortium initiative involved both acute and chronic dose studies of APAP in both the rat (Sprague-Dawley) and mouse (male B6C3F1). A metabonomic study of APAP in the rat was analyzed independently and reported by Sun et al., (Sun et al., 2008) who applied a multi-platform NMR and UPLC-MS approach to study both chronic and acute dosing of APAP in Sprague-Dawley rats (acute dosing 0, 400 and 1600 mg/kg by oral gavage; chronic dosing 0, 200, 400, 800 mg/kg by oral intubation for 7 days). Clinical chemistry revealed elevated plasma alanine transaminase (ALT) activity in the acute dosing study at 1600 mg/kg with no perturbation identified in the chronic dose study, reflective of the established resistance of the rat to APAP (McGill et al., 2012b). Histopathological assessment revealed the presence of multifocal, centrilobular hepatic necrosis at 48 hours following the acute administration of the high dose of APAP (1600 mg/kg), with inter-individual variability in the severity of the necrotic response ranging from mild to severe. Regenerative changes were identified as early as 48 hours post-treatment with resolution of necrosis by 168 hours. In addition, renal necrosis of the epithelial cells of the proximal convoluted tubules was observed (APAP 1600 mg/kg) albeit with a minimal score in terms of severity. The parallel urinary metabolic profiling component revealed similar qualitative endogenous metabolic perturbations in both the chronic and acute studies and identified APAP-related metabolites 13 using both NMR and UPLC-MS technologies which provided evidence for GSH conjugation of NAPQI. However, hepatic metabolic profiles or GSH levels were not assessed in this study. The urinary metabolic profiles paralleled histopathological assessment, with respect to regeneration and adaptation reflected in the re-establishment of metabolic homeostasis (metabolic profiles returned to pre-treatment or control states) in the acute dosing study. In contrast, the chronic dose study revealed persistent perturbations of endogenous metabolites and the absence of a return to homeostasis across the 13-day study time-course. Analysis of the NMR urinary profiles representing toxic response (acute dose of 1600 mg/kg) revealed significant perturbation of TCA cycle intermediates suggestive of a shift in energy metabolism. In addition, depletion of S-adenosylmethionine, taurine and N- methylnicotinate suggested a response to oxidative stress and potential upregulation of the trans-sulfuration pathway in an attempt to regenerate hepatic GSH stores. Glutathione biosynthesis, one carbon metabolism and the trans-sulfuration pathway The targeted application of metabolic profiling to study the effect of APAP administration on GSH biosynthesis and one carbon metabolism and trans-sulfuration has provided important mechanistic insight into hepatotoxic insult. A pioneering study in this regard involved the 1H NMR spectroscopic detection of urinary 5Oxoproline (pyroglutamate, 5-OP), an intermediate in the biosynthesis of GSH, with its urinary excretion potentially representing a non-invasive means of assessing hepatocellular GSH status. The first report of elevated urinary concentrations of 5-OP in response to druginduced depletion of glutathione was shown in a study of chronic APAP administration in the rat (1% in the diet for up to 10 weeks)(Ghauri et al., 1993). 5-Oxoprolinuria (pyroglutamic aciduria), in the context of APAP administration, was first observed using high-resolution 1H NMR spectroscopy following 2 weeks of APAP dosing, with urinary excretion at high levels thereafter (up to 1M absolute urinary concentration). 5-Oxoprolinuria was absent in animals supplemented with methionine, suggesting that chronic dosing of APAP resulted in a severe impairment of the total sulfur pool, which was restored with methionine supplementation. Elevation of 5-OP in urine, liver and plasma was also reported from a 1H NMR spectroscopic based metabonomic study of acute dosing of bromobenzene (1.5 g/kg Han-Wistar rats)(Waters et al., 2006). Bromobenzene, which causes centrilobular hepatic necrosis, is known to lead to GSH depletion as a result of detoxification of reactive epoxides (Lau et al., 1984). The induction of 5-oxoprolinuria which occurred between 31 and 55 hours post- 14 treatment, was believed to result from the bromobenzene-induced inhibition of GSH synthase and the lack of negative feedback inhibition of gamma-glutamyl-cysteine synthetase. 5-Oxoprolinuria has also been reported in patients with inherited disorders of the gammaglutamyl cycle such as a deficiency in GSH synthetase (EC 6.3.2.3) or in 5-oxoprolinase (EC 3.5.2.9) (Shi et al., 1996, Dahl et al., 1997, Calpena et al., 2013). 5-Oxoprolinuria has also been reported clinically in anion gap metabolic acidosis and is associated with exposure to APAP in the context of certain risk factors that include chronic use, pre-existing hepatic or renal disease, sepsis, malnutrition, female gender and pregnancy (Dempsey et al., 2000, O'Brien et al., 2012). With respect to further understanding perturbation of GSH homeostasis a particularly noteworthy study involved the application of CE-TOF-MS to profile aqueous-soluble liver extracts and serum following APAP administration (male C57BL/6 mice, 150 mg/kg, ip) with a focus on the study of metabolites involved in GSH homeostasis (Soga et al., 2006). A major reduction in both hepatic GSH and GSH disulfide (GSSG) was observed at 2 hours posttreatment, together with a reduction of numerous metabolites involved in the taurine shunt and the biosynthesis of GSH as summarized in Figure 5. Metabolites that were upstream of the cysteine biosynthesis pathway, such as methionine, were found to be significantly elevated. Interestingly, the authors found significantly increased levels of ophthalmic acid (OA), a non-sulfur-containing analogue of GSH, in which cysteine is replaced with 2aminobutyrate (gamma-Glu-2-AB-Gly, a thiol group is replaced with a methyl group). OA can be formed in vivo from 2-aminobutyrate in two reactions catalyzed by gammaglutamylcysteine synthetase (GCS) to form gamma-Glu-2AB and GSH synthetase (GS) to form OA. In support of this pathway elevated levels of gamma-Glu-2AB were also identified, which suggested induction of GCS. Critically, the authors carried out mechanistically driven experiments in which they they perturbed hepatic GSH levels via differential mechanisms through administration of diethylmaleate (DEM) or buthionine sulfoximine (BSO). BSO is known to inhibit GCS and thus reduce downstream metabolites, including GSH whereas DEM is known to oxidize the GSH thiol group and lead to lipid peroxidation and necrotic cell death. The BSO pre-treated group revealed reduced hepatic and serum levels of gamma-Glu-2AB, GSH and OA compared to the DEM pre-treated group, which resulted in increased levels of gamma-Glu-2AB and OA, with close concordance between serum and liver for OA and gamma-Glu-2AB. These data suggested that GCS inhibition, following oxidative stress and the utilization of GSH, resulted in increased synthesis of OA, and that OA may represent a 15 circulating biomarker of hepatic oxidative stress. The further study of OA and its upstream metabolites as potential biomarkers of oxidative stress together with translation to the clinical setting is warranted. Furthermore, a systems toxicology approach that generated a mathematical model of the gamma-glutamyl pathway in response to detoxification of APAP, on the basis of data generated following APAP exposure to a human liver-derived THLE cell line exposed to APAP, and transfected with human cytochrome CYP2E1 (THLE-2E1 cells), revealed that both OA and 5-OP levels alone depend not only on hepatocellular GSH levels but also on methionine status. Hence, it was concluded that both markers should be measured simultaneously to report on hepatic GSH status (Geenen et al., 2012). The authors identified an adaptive response experimentally, with respect to up-regulation of glutamyl cysteine synthetase, which explained the inability of the model to fully predict the experimental metabolite concentrations and flux data. With incorporation of this adaptive response the mathematical model revealed that 5-OP and OA were useful predictive biomarkers of GSH status when analyzed together and that methionine was critical in terms of detoxification capacity. The translation of this work to in vivo pre-clinical studies and the clinical setting will further strengthen the application of this model for prediction of GSH status and toxicological response. HPLC-MS/MS methods have recently been developed that enable the quantitative and targeted determination of both OA and 5-OP in both cellular media (THLE-CYP cell lines) and rat plasma and will prove invaluable for future studies of the clinical utility and predictive ability of these markers in the context of drug-induced liver injury and understanding cellular response to GSH perturbation (Geenen et al., 2011a, Geenen et al., 2011b). The wider cellular effects of perturbed GSH biosynthesis have been alluded to through the parallel profiling of perturbations in taurine and its downstream products, which provides potential to improve understanding of broad sulfur-dependent metabolic processes. Hepatic taurine and hypotaurine were found to be depleted following acute exposure to APAP in the rat (500 and 1000 mg/kg), in a metabolomic study of 14 different hepatotoxins (Yamazaki et al., 2013). The effect on taurine homeostasis was further explored through profiling of GSH and associated metabolites, and revealed that reduced hepatic GSH was associated with increased levels of OA, 2-aminobutyrate and the GSH catabolites that included gammaglutamyl-dipeptides and 5-OP. In addition, the targeted analysis of bile acids in this study showed increased plasma levels of glycine conjugated primary bile acids (glycocholate and 16 glycochenodeoxycholate) and depletion of taurine conjugated bile acids (taurocholate and taurochenodeoxycholate) following exposure to APAP. Taken together, this data suggests that the depletion of GSH, which was reflected in increased hepatic levels of 5-OP, OA and gamma-glutamyldipeptides, led to the increased utilization of cysteine for GSH resynthesis at the expense of taurine. The depletion of taurine supported the reduction in both hepatic and plasma taurine-conjugated bile acids. Given the complex task of reporting the clinical chemistry, pathological and targeted metabolic profiling (>1900 metabolites) of urine, plasma and liver for 14 hepatotoxins, it would be insightful to present the data for APAP alone and explore it at a deeper mechanistic level. The perturbation in the overall profile and conjugation pattern of bile acids is of interest for future study and could be extended to detail primary and secondary bile acid profiles in multiple matrices with assessment of their mechanistic specificity. A recent clinical study has explored serum bile acid profiles following APAP overdose in survivors and non-survivors (Woolbright et al., 2014) and found that glycodeoxycholic acid was significantly elevated in non-survivors and was modestly predictive of survival at admission to hospital (AUC 0.7) and when ALT peaked (AUC 0.68). This study focused on six bile acids that represented greater than 95% of the systemic bile acid pool and were present at high concentrations in the serum, namely, glycochenodeoxycholic acid (GCDCA), taurochenodeoxycholic acid (TCDCA), glycocholic acid (GCA), taurocholic acid (TCA), glycodeoxycholic acid (GDCA) and taurodeoxycholic acid (TDCA). Mitochondrial function and long-chain acylcarnitines Perturbation of serum acylcarnitines in response to APAP-induced toxicity has been reported and is of potential significance as a mechanistic means of assessing mitochondrial toxicity. Furthermore, the potential for serum acylcarnitines to act as mechanistic and predictive biomarkers of APAP-induced mitochondrial toxicity and clinical prognosis is compelling. Acylcarnitines are formed following conjugation of long-chain fatty acids with carnitine and are essential for the transport of long-chain fatty acids into mitochondria where they are subsequently metabolized by β-oxidation. A particularly note-worthy study and the first published example that showed acylcarnitine perturbations in response to APAP incorporated the use of a knock-out mouse model (Chen et al., 2009). The application of LC-MS to phenotype serum from both wild-type and CYP2E1null mice revealed significantly elevated levels of long-chain acylcarnitines 17 (palmitoylcarnitine, myristoylcarnitine, oleoylcarnitine and palmitoleoylcarnitine) at early time-points post APAP treatment (Figure 6A, B). In addition, the simultaneous detection of elevated levels of triglycerides and free fatty acids in wild-type mice suggested that there was an APAP-induced perturbation of fatty acid -oxidation. The elevation of long-chain acylcarnitine concentrations was persistent in wild-type mice but returned to control levels in CYP2E1-null mice within 24 hours of APAP treatment. The temporal elevation in serum acylcarnitines occurred at a different time-point than the observed increase in aspartate transaminase (AST) activity (Figure 6C), which it preceded, and the depletion of hepatic GSH (Figure 6D), which it followed. This suggested that serum acylcarnitine profiles informed upon a unique cellular phenotype and that they may serve as complementary to traditional markers of liver injury or function. The role of the nuclear transcription factor, peroxisome proliferator-activated receptor alpha (PPAR-) in raising serum concentrations of acylcarnitines was explored through the study of response to a fasting challenge in wild-type and PPAR- null mice. PPAR- null mice that were either fed or fasted exhibited gross metabolome differences in comparison to wild-type mice, which included accumulation of acylcarnitines, suggesting a link with inhibition of PPAR- function and regulation of βoxidation. This was further explored through a targeted study of PPAR- gene expression following APAP challenge, which revealed that activation of PPAR- was more persistent in CYP2E1-null mice leading to greater up-regulation of PPAR- genes involved in β-oxidation. An additional pre-clinical, targeted LC-MS based metabolomic study of serum acylcarnitines involved exposure to APAP to male B6C3F1 mice (200 mg/kg ip), following an overnight fast (Bhattacharyya et al., 2013). This study also revealed statistically significantly increased amounts of palmitoyl, oleoyl and myristoylcarnitine by 2 hours post-treatment with peak levels observed by 4 hours post-treatment. Interestingly, the quantities of these long-chain acylcarnitines fell below those of the controls at 8 hours and up to 48 hours post-treatment. In comparison, L-carnitine was found to be increased at 8 hours post-treatment with reduced levels of acetyl-carnitine found at all time-points. The elevation of acylcarnitines was modest and reflected the reduction in hepatic GSH levels and presence of APAP protein adducts. The reduction in the levels of palmitoylcarnitine relative to controls from 8h posttreatment onwards was not observed in the earlier study (Chen et al., 2009) which may be attributable to differences in the study design such as the mouse strain, dose level, length of fasting or analytical platform and experiments that were utilized. A more recent study evaluated serum acylcarnitines in a pre-clinical model of APAP toxicity together with clinical APAP overdose patients, to assess the role of these metabolites in 18 predicting clinical outcomes and their potential to serve as mitochondrial toxicity biomarkers (McGill et al., 2014a). This study involved a pre-clinical component in which male C57BL/6 mice were treated with APAP (fasted; 300 and fed; 600 mg/kg, ip) and included a treatment group that was given N-acetylcysteine 1.5 hours post APAP-treatment. The study also included administration of furosemide as a negative control, given the known induction of centrilobular necrosis that is similar to that induced by APAP but with no known mitochondrial perturbation. Histopathology revealed the presence of a severe necrotic lesion at 12 hours post-treatment with both dose levels of APAP, together with significantly elevated levels of ALT activity. RP-UPLC-MS analysis revealed the elevation of three serum acylcarnitines; palmitoylcarnitine, linoleoylcarnitine and oleoylcarnitine, within 3 hours of administration of APAP, at both dose levels, until 12 hours post-treatment. Interestingly this elevation was observed for the differential nutritional status groups (fasted; 600 mg/kg, fed; 300 mg/kg) and was not observed following furosemide treatment, suggesting that the increased acylcarnitine levels were reflective of mitochondrial toxicity. However, in this study no elevation of acylcarnitines was found in patients with both normal (n=14) and abnormal liver function (n=16, based on ALT activity) compared to healthy controls (n=6) following APAP overdose. This negative result may simply reflect the late presentation of patients to hospital and the subsequent sampling, that missed an early increase in circulating acylcarnitines. However a more plausible confounding factor in this analysis, discussed by the authors, was the treatment of all patients with N-acetylcysteine (NAC) prior to sampling. NAC is the principal antidote used in APAP-overdose: it restores GSH levels and improves hepatic mitochondrial bioenergetics through supply of Krebs cycle intermediates and restoration of hepatic ALT levels (Saito et al., 2010). The authors studied the effect of supplementation with NAC (140 mg/kg) 1.5 hours post-APAP treatment in mice on serum acylcarnitine levels and found significant depletion in the co-treatment group, reflecting the therapeutic action of NAC. This led to the hypothesis that NAC improved mitochondrial function and hence resulted in a reduction in serum acylcarnitine levels. The underlying assumption was that NAC did not simply scavenge NAPQI or reactive oxygen species (ROS) since NAPQI covalent binding is known to plateau at the time-point chosen. The study represents an important addition to the literature given the comparative and detailed mechanistic analysis between the pre-clinical model and the patient. The clinical element of this study needs to be expanded to larger cohorts and integrated and anchored with recently identified biomarkers of mitochondrial damage that include nuclear DNA fragmentation, mtDNA and glutamate dehydrogenase (GDH) activity (McGill et al., 2012a, 19 McGill et al., 2014b). This would enable improved understanding of the mechanisms underlying clinical APAP-induced toxicity and could be validated in independent cohorts and potentially lead to enhanced stratification of patient with respect to prognosis. The future identification of novel biomarkers that are predictive and prognostic in APAP overdose are ultimately dependent on extensive biobank cohorts that are well phenotyped from multiple perspectives and reflect the patient journey from an early stage. A final example of the targeted study of acylcarnitine perturbation in response to APAP involved the preclinical study of the protective effect of Wuzhi (Schisandra sphenanthera extract) in acute APAP-induced toxicity in C57BL/6 mice, 400 mg/kg APAP and pre-treatment for three days with Wuzhi). This study revealed considerable protection following pretreatment with Wuzhi, with respect to a dramatically reduced ALT response and no histopathological evidence of necrosis. (Bi et al., 2013) The APAP-induced increase in longchain serum acylcarnitines that included palmitoylcarnitine and oleoylcarnitine was ameliorated through Wuzhi pre-treatment at both 2 and 24 hours post-treatment, providing further evidence for the utility of acylcarnitines as biomarkers of APAP-induced hepatotoxicity and mitochondrial dysfunction. Furthermore, a dramatic increase in serum triglycerides and free fatty acid levels was observed only in the APAP-treated animals and not in the Wuhzi pre-treatment group providing evidence for a lack of disruption to fatty acid -oxidation in the pre-treatment group. However, the APAP-induced depletion of hepatic GSH was not prevented by pre-treatment with Wuzhi although a marginal increase in GSH levels was reported following treatment with Wuzhi alone. However, this perturbation was statistically insignificant which suggested alternative, and as of yet unknown, mechanisms were responsible for the protective effect. The validity and translational relevance of studies that assess the protection of natural products against APAP hepatotoxicity, in which the natural product is administered prior to APAP, have been questioned (Jaeschke et al., 2012). Recent review articles have outlined the generation of pharmacologically and clinically relevant data from carefully designed studies together with detailed assessments of protective mechanisms post-APAP ingestion (Jaeschke et al., 2010, Jaeschke et al., 2013). Translational application of metabolic profiling and pharmacometabonomics The field of pharmacometabonomics was conceptualized in a paper by Clayton et al., and defined as ‘the prediction of the outcome (for example, efficacy or toxicity) of a drug or 20 xenobiotic intervention in an individual based on a mathematical model of pre-intervention metabolite signatures’ (Clayton et al., 2006). The authors reported on the application of NMR spectroscopy to profile urine from both pre-and post-treatment time-points following a single toxic-threshold dose of APAP in rats. Clinical chemistry and histopathology were applied to assess the severity of liver damage with generation of a mean histology score (MHS) for each animal based on microscopic observation of damage in each of five liver lobes. The post-treatment spectra were utilized to quantify the 24 hour excretion of APAP, APAP-S, APAP-G and APAP-NAC. The MHS and the mole ratio of APAP-metabolites revealed considerable inter-animal variability and both end-points were modeled against the predose urinary metabolic profiles reflecting the endogenous metabolic complement. A predictive partial least squares (PLS) model of the mole ratio of APAP-G to APAP revealed a positive correlation (r = 0.48) to the spectral region spanning 5.06-5.14 ppm. This region contained the anomeric proton resonance of APAP-G and would be expected to also reflect the presence of endogenous ether glucuronides. The spectral region was hypothesized to be predictive of the individual glucuronidation capacity of each animal. The authors also explored the separation of the pre-dose urinary profiles based on three discrete post-treatment classes that were identified from the MHS (reflecting no/minimal necrosis (class 1), mild necrosis (class 2) and moderate necrosis (class 3)) using unsupervised principal components analysis (PCA), as shown in Figure 7. Partial separation was observed between class 1 and 3 in principal component 2 (PC2) which was identified as due to differential levels of taurine, trimethylamine N-oxide (TMAO) and betaine. For example, higher amounts of pre-dose urinary taurine were associated with a lower MHS, and higher levels of both TMAO and betaine were associated with increased severity of liver necrosis. The authors hypothesized that taurine levels might reflect the availability of inorganic sulfate and more broadly of phosphoadenosine phosphosulfate (PAPS), which correlated with the observation that animals with more severe liver necrosis showed lower levels of APAP-sulfate. The presence of higher levels of pre-dose urinary TMAO was interpreted as being reflective of differential gut microfloral populations which may have played a role in determination of the extent of APAP-induced liver injury. This work represented the first exemplar of the potential for pharmacometabonomics to predict xenobiotic transformation and toxic outcomes from pre-clinical baseline metabolic phenotypes. The first ‘proof-of-principle’ of the translation of pharmacometabonomics to a human/clinical study also used APAP as the exemplar (Clayton et al., 2009). A clinical trial design involved recruitment of healthy male volunteers (n=99) who were non-smokers and 21 not taking drugs, dietary supplements or herbal medicines, with additional restrictions placed on diet and alcohol intake. A single ‘spot’ urine was collected pre-dose, following which 1g of APAP was ingested orally and urine was collected from 0-3 hours and 3-6 hours post-treatment. NMR spectroscopic urinary profiles were acquired and the excretion of APAP and its major metabolites quantified. The analysis focused on calculation of the excretion ratio of APAP-S to APAP-G from the integral of the N-acetyl spectral peaks in both post-treatment time-points (with the correlation of excretion calculations based on the corresponding aromatic signals also given). The post-dose outcome (APAP-S/APAP-G ratio), that reflected inter-individual variability in the metabolism of a therapeutic dose of APAP was modeled against the pre-treatment creatinine-normalized spot urine profiles. The application of PLS-based approaches did not reveal any significant associations between the pre-treatment profiles and the post-dose outcome, unlike the earlier pre-clinical result (detailed above – Figure 6). The authors proceeded with a detailed visual comparison of the pre-treatment spectra at the extreme ends of the S/G distribution (high and low ratios) and identified two metabolites; p-cresol-sulfate (PCS) and phenylacetylglutamine (PAG), for which higher levels of these metabolites were visually associated with a lower APAP-S/APAPG ratio. The authors found a statistically significant association between the post-dose excretion of APAP-S/APAP-G to pre-dose levels of PCS/creatinine (Bonferroni correction for multiple testing). P-cresol is produced from tyrosine largely by the colonic microflora and believed to be sulfated by the cytosolic sulfotransferase, SULT1A1, and 3’- phosphoadenosine-5’-phosphosulfate (PAPS). Hence, the authors hypothesized that high production of pre-dose endogenous p-cresol may reduce the capacity of an individual to sulfate APAP through competitive sulfonation, given their structural similarities and suggest this may occur in both the colon and the liver. This study provided novel and interesting data, to support the role of environmental factors such as the gut microflora in the alteration of drug metabolism and may translate to the mechanistic understanding of differential response, for example in drug-induced liver injury. This warrants further research that validates and tests these findings in independent clinical cohorts and that elucidates the mechanism and means of assessment of competitive sulfonation. Indeed, to date metabolic profiling has played a significant role in further understanding the complex interactions between the host and gut microbiome (Holmes et al., 2012, Li and Jia, 2013, Nicholson et al., 2012). An additional clinical metabonomic study of APAP was carried out by Winnike et al., in which 4g of APAP was administered daily and across seven days to healthy volunteers (n=71, male 22 and female,(Winnike et al., 2010)). Based on the serum ALT activity levels the authors identified three sub-classes termed ‘responders’ (n=17) who showed increased ALT (>2.0 times the baseline level) following onset of dosing and ‘non-responders’ (n=18) who showed little change in ALT (< 1.5 times the baseline level) and ‘intermediate responders’ (between 1.5 and 2.0 times the baseline level). The authors focused on discrimination of the spectral profiles of responders from non-responders, both pre-dose and post-dose, using a multivariate approach comprised of both supervised and unsupervised statistical methods. O-PLS-DA models revealed separation of both the day 5 and day 9 urine collections for responders and non-responders based on a combination of endogenous and APAP related metabolites, reflecting perturbations that mirrored the ALT rise (day 9) and those that preceded it and this approach was classified as ‘early intervention pharmacometabonomics’ (day 5). However, generation of a robust O-PLS-DA model that discriminated the pre-dose urinary profiles on the basis of outcome was not possible. An important distinction from the analyses performed by Clayton et al., is that quantification of the excretion of APAP and its metabolites was not carried out by Winnike et al. It would be interesting to quantify the excretion of APAP-S and APAP-G and to test for an association between excretion of these metabolites and endogenous PCS, as was identified by Clayton et al., albeit in a different study design with respect to the clinical cohort and the dose and time-course. This important study, together with the concept of ‘early intervention pharmacometabonomics’, may play a significant role in the clinical setting in understanding the inter-individual balance between efficacy and toxicity of therapies. The growing number of original research contributions to the field of pharmacometabonomics, which span multiple compounds both pre-clinically and clinically, has been reviewed most recently by Everett et al., 2013 (Everett et al., 2013). Future Perspectives The targeted study of classes of metabolites such as long-chain acylcarnitines and metabolites involved in the biosynthesis of GSH represent intriguing exemplars of the power of the approach to identify novel biomarkers that may prove of mechanistic specificity. However, the power of untargeted, global profiling approaches also warrants further study as it presents significant potential for the identification of novel metabolites or classes of metabolites that inform on or predict hepatotoxicity. The continued and expanded study of metabolites that reflect mitochondrial metabolism and dysfunction may provide 23 mechanism-specific markers together with an understanding of the causal or down-stream and up-stream events for a given mechanism of hepatotoxicity. In addition, the extension of current research to encompass wider metabolic pathway coverage is crucial, for example, to profile the totality of sulfur-containing metabolites and sulfur-dependent processes in response to hepatotoxic insult. The study of a CYP2E1 knock-out animal model has provided mechanism-specific understanding of APAP-induced changes on the metabolome, specifically in understanding the role of PPAR- in the inhibition of fatty acid -oxidation following an APAP challenge. It is anticipated that continued application of knock-out models together with newlydeveloped humanized mice models are anticipated to provide further insight into critical pathway perturbations and data of clinical relevance and allow for the testing and validation of hypotheses generated at the early, untargeted experimental stage. The continued development of improved bioinformatics strategies to enhance spectral information recovery and ultimately aid in identification of novel biomarkers will play an important role in the development of this field and its future clinical applications, particularly with respect to information-rich and complex LC-MS data and in large-scale clinical phenotyping. Conclusion In conclusion, the application of metabolic phenotyping to study APAP metabolism and hepatotoxicity has provided a significant contribution to the scientific literature and continues to provide novel mechanistic insight from an ever-growing number of applications. There is immense future potential for the identification of panels of metabolic biomarkers that hold translational clinical relevance for improved patient stratification and the prediction of disease prognosis, with respect to APAP-induced acute liver failure and possibly more broadly to other forms of hepatic disease. Acknowledgements: Professors Ian Wilson and John Lindon are acknowledged for their insightful discussion and for proof-reading the manuscript. Mr Michael Kyriakides is acknowledged for provision of Figure 3 (unpublished data). 24 Declaration of Interest The MRC ITTP scheme is acknowledged for funding to MC. 25 References: Bales, J. R., Bell, J. D., Nicholson, J. K., Sadler, P. J., Timbrell, J. A., Hughes, R. D., Bennett, P. N. & Williams, R. 1988. Metabolic profiling of body fluids by proton NMR: self-poisoning episodes with paracetamol (acetaminophen). Magn Reson Med, 6, 300-6. Bales, J. R., Higham, D. P., Howe, I., Nicholson, J. K. & Sadler, P. J. 1984a. Use of high-resolution proton nuclear magnetic resonance spectroscopy for rapid multi-component analysis of urine. Clin Chem, 30, 426-32. Bales, J. R., Nicholson, J. K. & Sadler, P. J. 1985. Two-dimensional proton nuclear magnetic resonance "maps" of acetaminophen metabolites in human urine. Clin Chem, 31, 757-62. Bales, J. R., Sadler, P. J., Nicholson, J. K. & Timbrell, J. A. 1984b. Urinary excretion of acetaminophen and its metabolites as studied by proton NMR spectroscopy. Clin Chem, 30, 1631-6. Beckonert, O., Coen, M., Keun, H. C., Wang, Y., Ebbels, T. M., Holmes, E., Lindon, J. C. & Nicholson, J. K. 2010. High-resolution magic-angle-spinning NMR spectroscopy for metabolic profiling of intact tissues. Nat Protoc, 5, 101932. Beckonert, O., Keun, H. C., Ebbels, T. M., Bundy, J., Holmes, E., Lindon, J. C. & Nicholson, J. K. 2007. Metabolic profiling, metabolomic and metabonomic procedures for NMR spectroscopy of urine, plasma, serum and tissue extracts. Nat Protoc, 2, 2692-703. Benton, H. P., Want, E., Keun, H. C., Amberg, A., Plumb, R. S., Goldfain-Blanc, F., Walther, B., Reily, M. D., Lindon, J. C., Holmes, E., Nicholson, J. K. & Ebbels, T. M. 2012. Intra- and interlaboratory reproducibility of ultra performance liquid chromatography-time-of-flight mass spectrometry for urinary metabolic profiling. Anal Chem, 84, 2424-32. Bernal, W., Auzinger, G., Dhawan, A. & Wendon, J. 2010. Acute liver failure. Lancet, 376, 190-201. Bernal, W., Hyyrylainen, A., Gera, A., Audimoolam, V. K., Mcphail, M. J., Auzinger, G., Rela, M., Heaton, N., O'grady, J. G., Wendon, J. & Williams, R. 2013. Lessons from look-back in acute liver failure? A single centre experience of 3300 patients. J Hepatol, 59, 74-80. Bhattacharyya, S., Pence, L., Beger, R., Chaudhuri, S., Mccullough, S., Yan, K., Simpson, P., Hennings, L., Hinson, J. & James, L. 2013. Acylcarnitine profiles in acetaminophen toxicity in the mouse: comparison to toxicity, metabolism and hepatocyte regeneration. Metabolites, 3, 606-22. Bi, H., Li, F., Krausz, K. W., Qu, A., Johnson, C. H. & Gonzalez, F. J. 2013. Targeted Metabolomics of Serum Acylcarnitines Evaluates Hepatoprotective Effect of Wuzhi Tablet (Schisandra sphenanthera Extract) against Acute Acetaminophen Toxicity. Evid Based Complement Alternat Med, 2013, 985257. Calpena, E., Casado, M., Martinez-Rubio, D., Nascimento, A., Colomer, J., Gargallo, E., Garcia-Cazorla, A., Palau, F., Artuch, R. & Espinos, C. 2013. 5Oxoprolinuria in Heterozygous Patients for 5-Oxoprolinase (OPLAH) Missense Changes. JIMD Rep, 7, 123-8. 26 Chan, E. C., Pasikanti, K. K. & Nicholson, J. K. 2011. Global urinary metabolic profiling procedures using gas chromatography-mass spectrometry. Nat Protoc, 6, 1483-99. Chen, C., Krausz, K. W., Idle, J. R. & Gonzalez, F. J. 2008. Identification of novel toxicity-associated metabolites by metabolomics and mass isotopomer analysis of acetaminophen metabolism in wild-type and Cyp2e1-null mice. J Biol Chem, 283, 4543-59. Chen, C., Krausz, K. W., Shah, Y. M., Idle, J. R. & Gonzalez, F. J. 2009. Serum metabolomics reveals irreversible inhibition of fatty acid beta-oxidation through the suppression of PPARalpha activation as a contributing mechanism of acetaminophen-induced hepatotoxicity. Chem Res Toxicol, 22, 699-707. Chen, W., Shockcor, J. P., Tonge, R., Hunter, A., Gartner, C. & Nelson, S. D. 1999. Protein and nonprotein cysteinyl thiol modification by N-acetyl-pbenzoquinone imine via a novel ipso adduct. Biochemistry, 38, 8159-66. Clayton, T. A., Baker, D., Lindon, J. C., Everett, J. R. & Nicholson, J. K. 2009. Pharmacometabonomic identification of a significant host-microbiome metabolic interaction affecting human drug metabolism. Proc Natl Acad Sci U S A, 106, 14728-33. Clayton, T. A., Lindon, J. C., Cloarec, O., Antti, H., Charuel, C., Hanton, G., Provost, J. P., Le Net, J. L., Baker, D., Walley, R. J., Everett, J. R. & Nicholson, J. K. 2006. Pharmaco-metabonomic phenotyping and personalized drug treatment. Nature, 440, 1073-7. Cloarec, O., Dumas, M. E., Craig, A., Barton, R. H., Trygg, J., Hudson, J., Blancher, C., Gauguier, D., Lindon, J. C., Holmes, E. & Nicholson, J. 2005. Statistical total correlation spectroscopy: an exploratory approach for latent biomarker identification from metabolic 1H NMR data sets. Anal Chem, 77, 1282-9. Coen, M. 2010. A metabonomic approach for mechanistic exploration of preclinical toxicology. Toxicology, 278, 326-40. Coen, M., Hong, Y. S., Cloarec, O., Rhode, C. M., Reily, M. D., Robertson, D. G., Holmes, E., Lindon, J. C. & Nicholson, J. K. 2007. Heteronuclear 1H-31P statistical total correlation NMR spectroscopy of intact liver for metabolic biomarker assignment: application to galactosamine-induced hepatotoxicity. Anal Chem, 79, 8956-66. Coen, M., Lenz, E. M., Nicholson, J. K., Wilson, I. D., Pognan, F. & Lindon, J. C. 2003. An integrated metabonomic investigation of acetaminophen toxicity in the mouse using NMR spectroscopy. Chem Res Toxicol, 16, 295-303. Coen, M., Ruepp, S. U., Lindon, J. C., Nicholson, J. K., Pognan, F., Lenz, E. M. & Wilson, I. D. 2004. Integrated application of transcriptomics and metabonomics yields new insight into the toxicity due to paracetamol in the mouse. J Pharm Biomed Anal, 35, 93-105. Dahl, N., Pigg, M., Ristoff, E., Gali, R., Carlsson, B., Mannervik, B., Larsson, A. & Board, P. 1997. Missense mutations in the human glutathione synthetase gene result in severe metabolic acidosis, 5-oxoprolinuria, hemolytic anemia and neurological dysfunction. Hum Mol Genet, 6, 1147-52. Dahlin, D. C., Miwa, G. T., Lu, A. Y. & Nelson, S. D. 1984. N-acetyl-p-benzoquinone imine: a cytochrome P-450-mediated oxidation product of acetaminophen. Proc Natl Acad Sci U S A, 81, 1327-31. 27 Dai, W., Huang, Q., Yin, P., Li, J., Zhou, J., Kong, H., Zhao, C., Lu, X. & Xu, G. 2012. Comprehensive and highly sensitive urinary steroid hormone profiling method based on stable isotope-labeling liquid chromatography-mass spectrometry. Anal Chem, 84, 10245-51. Dempsey, G. A., Lyall, H. J., Corke, C. F. & Scheinkestel, C. D. 2000. Pyroglutamic acidemia: a cause of high anion gap metabolic acidosis. Crit Care Med, 28, 1803-7. Dona, A. C., Jimenez, B., Schaefer, H., Humpfer, E., Spraul, M., Lewis, M. R., Pearce, J. T., Holmes, E., Lindon, J. C. & Nicholson, J. K. 2014a. Precision high throughput proton NMR spectroscopy of human urine, serum and plasma for large-scale metabolic phenotyping. Anal Chem. Dona, A. C., Jimenez, B., Schafer, H., Humpfer, E., Spraul, M., Lewis, M. R., Pearce, J. T., Holmes, E., Lindon, J. C. & Nicholson, J. K. 2014b. Precision highthroughput proton NMR spectroscopy of human urine, serum, and plasma for large-scale metabolic phenotyping. Anal Chem, 86, 9887-94. Dumas, M. E., Maibaum, E. C., Teague, C., Ueshima, H., Zhou, B., Lindon, J. C., Nicholson, J. K., Stamler, J., Elliott, P., Chan, Q. & Holmes, E. 2006. Assessment of analytical reproducibility of 1H NMR spectroscopy based metabonomics for large-scale epidemiological research: the INTERMAP Study. Anal Chem, 78, 2199-208. Dunn, W. B., Broadhurst, D., Begley, P., Zelena, E., Francis-Mcintyre, S., Anderson, N., Brown, M., Knowles, J. D., Halsall, A., Haselden, J. N., Nicholls, A. W., Wilson, I. D., Kell, D. B. & Goodacre, R. 2011. Procedures for large-scale metabolic profiling of serum and plasma using gas chromatography and liquid chromatography coupled to mass spectrometry. Nat Protoc, 6, 1060-83. Ebbels, T. M., Keun, H. C., Beckonert, O. P., Bollard, M. E., Lindon, J. C., Holmes, E. & Nicholson, J. K. 2007. Prediction and classification of drug toxicity using probabilistic modeling of temporal metabolic data: the consortium on metabonomic toxicology screening approach. J Proteome Res, 6, 4407-22. Everett, J. R., Loo, R. L. & Pullen, F. S. 2013. Pharmacometabonomics and personalized medicine. Ann Clin Biochem, 50, 523-45. Geenen, S., Du Preez, F. B., Reed, M., Nijhout, H. F., Kenna, J. G., Wilson, I. D., Westerhoff, H. V. & Snoep, J. L. 2012. A mathematical modelling approach to assessing the reliability of biomarkers of glutathione metabolism. Eur J Pharm Sci, 46, 233-43. Geenen, S., Guallar-Hoyas, C., Michopoulos, F., Kenna, J. G., Kolaja, K. L., Westerhoff, H. V., Thomas, P. & Wilson, I. D. 2011a. HPLC-MS/MS methods for the quantitative analysis of 5-oxoproline (pyroglutamate) in rat plasma and hepatic cell line culture medium. J Pharm Biomed Anal, 56, 655-63. Geenen, S., Michopoulos, F., Kenna, J. G., Kolaja, K. L., Westerhoff, H. V. & Wilson, I. 2011b. HPLC-MS/MS methods for the quantitative analysis of ophthalmic acid in rodent plasma and hepatic cell line culture medium. J Pharm Biomed Anal, 54, 1128-35. Ghauri, F. Y., Mclean, A. E., Beales, D., Wilson, I. D. & Nicholson, J. K. 1993. Induction of 5-oxoprolinuria in the rat following chronic feeding with Nacetyl 4-aminophenol (paracetamol). Biochem Pharmacol, 46, 953-7. 28 Godejohann, M., Tseng, L. H., Braumann, U., Fuchser, J. & Spraul, M. 2004. Characterization of a paracetamol metabolite using on-line LC-SPE-NMRMS and a cryogenic NMR probe. J Chromatogr A, 1058, 191-6. Holmes, E., Kinross, J., Gibson, G. R., Burcelin, R., Jia, W., Pettersson, S. & Nicholson, J. K. 2012. Therapeutic modulation of microbiota-host metabolic interactions. Sci Transl Med, 4, 137rv6. Holmes, E., Loo, R. L., Cloarec, O., Coen, M., Tang, H., Maibaum, E., Bruce, S., Chan, Q., Elliott, P., Stamler, J., Wilson, I. D., Lindon, J. C. & Nicholson, J. K. 2007. Detection of urinary drug metabolite (xenometabolome) signatures in molecular epidemiology studies via statistical total correlation (NMR) spectroscopy. Anal Chem, 79, 2629-40. Jaeschke, H., Williams, C. D. & Mcgill, M. R. 2012. Caveats of using acetaminophen hepatotoxicity models for natural product testing. Toxicol Lett, 215, 40-1. Jaeschke, H., Williams, C. D., Mcgill, M. R. & Farhood, A. 2010. Herbal extracts as hepatoprotectants against acetaminophen hepatotoxicity. World J Gastroenterol, 16, 2448-50. Jaeschke, H., Williams, C. D., Mcgill, M. R., Xie, Y. & Ramachandran, A. 2013. Models of drug-induced liver injury for evaluation of phytotherapeutics and other natural products. Food Chem Toxicol, 55, 279-89. Jimenez, B., Mirnezami, R., Kinross, J., Cloarec, O., Keun, H. C., Holmes, E., Goldin, R. D., Ziprin, P., Darzi, A. & Nicholson, J. K. 2013. 1H HR-MAS NMR spectroscopy of tumor-induced local metabolic "field-effects" enables colorectal cancer staging and prognostication. J Proteome Res, 12, 959-68. Johnson, C. H., Athersuch, T. J., Wilson, I. D., Iddon, L., Meng, X., Stachulski, A. V., Lindon, J. C. & Nicholson, J. K. 2008. Kinetic and J-resolved statistical total correlation NMR spectroscopy approaches to structural information recovery in complex reacting mixtures: application to acyl glucuronide intramolecular transacylation reactions. Anal Chem, 80, 4886-95. Jollow, D. J., Mitchell, J. R., Potter, W. Z., Davis, D. C., Gillette, J. R. & Brodie, B. B. 1973. Acetaminophen-induced hepatic necrosis. II. Role of covalent binding in vivo. J Pharmacol Exp Ther, 187, 195-202. Keun, H. C., Athersuch, T. J., Beckonert, O., Wang, Y., Saric, J., Shockcor, J. P., Lindon, J. C., Wilson, I. D., Holmes, E. & Nicholson, J. K. 2008. Heteronuclear 19F-1H statistical total correlation spectroscopy as a tool in drug metabolism: study of flucloxacillin biotransformation. Anal Chem, 80, 1073-9. Keun, H. C., Ebbels, T. M., Antti, H., Bollard, M. E., Beckonert, O., Schlotterbeck, G., Senn, H., Niederhauser, U., Holmes, E., Lindon, J. C. & Nicholson, J. K. 2002. Analytical reproducibility in (1)H NMR-based metabonomic urinalysis. Chem Res Toxicol, 15, 1380-6. Lau, S. S., Monks, T. J. & Gillette, J. R. 1984. Multiple reactive metabolites derived from bromobenzene. Drug Metab Dispos, 12, 291-6. Lee, W. M. 2012. Recent developments in acute liver failure. Best Pract Res Clin Gastroenterol, 26, 3-16. Li, F., Lu, J. & Ma, X. 2011. Profiling the reactive metabolites of xenobiotics using metabolomic technologies. Chem Res Toxicol, 24, 744-51. Li, H. & Jia, W. 2013. Cometabolism of microbes and host: implications for drug metabolism and drug-induced toxicity. Clin Pharmacol Ther, 94, 574-81. 29 Lindon, J. C., Keun, H. C., Ebbels, T. M., Pearce, J. M., Holmes, E. & Nicholson, J. K. 2005. The Consortium for Metabonomic Toxicology (COMET): aims, activities and achievements. Pharmacogenomics, 6, 691-9. Lindon, J. C., Nicholson, J. K., Holmes, E., Antti, H., Bollard, M. E., Keun, H., Beckonert, O., Ebbels, T. M., Reily, M. D., Robertson, D., Stevens, G. J., Luke, P., Breau, A. P., Cantor, G. H., Bible, R. H., Niederhauser, U., Senn, H., Schlotterbeck, G., Sidelmann, U. G., Laursen, S. M., Tymiak, A., Car, B. D., Lehman-Mckeeman, L., Colet, J. M., Loukaci, A. & Thomas, C. 2003. Contemporary issues in toxicology the role of metabonomics in toxicology and its evaluation by the COMET project. Toxicol Appl Pharmacol, 187, 137-46. Madsen, R., Lundstedt, T. & Trygg, J. 2010. Chemometrics in metabolomics--a review in human disease diagnosis. Anal Chim Acta, 659, 23-33. Mcgill, M. R., Li, F., Sharpe, M. R., Williams, C. D., Curry, S. C., Ma, X. & Jaeschke, H. 2014a. Circulating acylcarnitines as biomarkers of mitochondrial dysfunction after acetaminophen overdose in mice and humans. Arch Toxicol, 88, 391-401. Mcgill, M. R., Sharpe, M. R., Williams, C. D., Taha, M., Curry, S. C. & Jaeschke, H. 2012a. The mechanism underlying acetaminophen-induced hepatotoxicity in humans and mice involves mitochondrial damage and nuclear DNA fragmentation. J Clin Invest, 122, 1574-83. Mcgill, M. R., Staggs, V. S., Sharpe, M. R., Lee, W. M. & Jaeschke, H. 2014b. Serum mitochondrial biomarkers and damage-associated molecular patterns are higher in acetaminophen overdose patients with poor outcome. Hepatology, 60, 1336-45. Mcgill, M. R., Williams, C. D., Xie, Y., Ramachandran, A. & Jaeschke, H. 2012b. Acetaminophen-induced liver injury in rats and mice: comparison of protein adducts, mitochondrial dysfunction, and oxidative stress in the mechanism of toxicity. Toxicol Appl Pharmacol, 264, 387-94. Mirnezami, R., Jimenez, B., Li, J. V., Kinross, J. M., Veselkov, K., Goldin, R. D., Holmes, E., Nicholson, J. K. & Darzi, A. 2014. Rapid diagnosis and staging of colorectal cancer via high-resolution magic angle spinning nuclear magnetic resonance (HR-MAS NMR) spectroscopy of intact tissue biopsies. Ann Surg, 259, 1138-49. Nelson, S. D. 1982. Metabolic activation and drug toxicity. J Med Chem, 25, 753-65. Nicholls, A. W., Caddick, S., Wilson, I. D., Farrant, R. D., Lindon, J. C. & Nicholson, J. K. 1995. High resolution NMR spectroscopic studies on the metabolism and futile deacetylation of 4-hydroxyacetanilide (paracetamol) in the rat. Biochem Pharmacol, 49, 1155-64. Nicholls, A. W., Farrant, R. D., Shockcor, J. P., Unger, S. E., Wilson, I. D., Lindon, J. C. & Nicholson, J. K. 1997. NMR and HPLC-NMR spectroscopic studies of futile deacetylation in paracetamol metabolites in rat and man. J Pharm Biomed Anal, 15, 901-10. Nicholson, J. K., Connelly, J., Lindon, J. C. & Holmes, E. 2002. Metabonomics: a platform for studying drug toxicity and gene function. Nat Rev Drug Discov, 1, 153-61. Nicholson, J. K., Holmes, E., Kinross, J., Burcelin, R., Gibson, G., Jia, W. & Pettersson, S. 2012. Host-gut microbiota metabolic interactions. Science, 336, 1262-7. 30 Nicholson, J. K., Lindon, J. C. & Holmes, E. 1999. 'Metabonomics': understanding the metabolic responses of living systems to pathophysiological stimuli via multivariate statistical analysis of biological NMR spectroscopic data. Xenobiotica, 29, 1181-9. O'brien, L. M., Hooper, M., Flemmer, M. & Marik, P. E. 2012. Chronic acetaminophen ingestion resulting in severe anion gap metabolic acidosis secondary to 5-oxoproline accumulation: an under diagnosed phenomenon. BMJ Case Rep, 2012. Ramautar, R., Nevedomskaya, E., Mayboroda, O. A., Deelder, A. M., Wilson, I. D., Gika, H. G., Theodoridis, G. A., Somsen, G. W. & De Jong, G. J. 2011. Metabolic profiling of human urine by CE-MS using a positively charged capillary coating and comparison with UPLC-MS. Mol Biosyst, 7, 194-9. Ramautar, R., Somsen, G. W. & De Jong, G. J. 2014. CE-MS for metabolomics: Developments and applications in the period 2012-2014. Electrophoresis. Robinette, S. L., Lindon, J. C. & Nicholson, J. K. 2013. Statistical spectroscopic tools for biomarker discovery and systems medicine. Anal Chem, 85, 5297-303. Saito, C., Zwingmann, C. & Jaeschke, H. 2010. Novel mechanisms of protection against acetaminophen hepatotoxicity in mice by glutathione and Nacetylcysteine. Hepatology, 51, 246-54. Sands, C. J., Coen, M., Ebbels, T. M., Holmes, E., Lindon, J. C. & Nicholson, J. K. 2011. Data-driven approach for metabolite relationship recovery in biological 1H NMR data sets using iterative statistical total correlation spectroscopy. Anal Chem, 83, 2075-82. Shi, Z. Z., Habib, G. M., Rhead, W. J., Gahl, W. A., He, X., Sazer, S. & Lieberman, M. W. 1996. Mutations in the glutathione synthetase gene cause 5-oxoprolinuria. Nat Genet, 14, 361-5. Shipkova, P., Vassallo, J. D., Aranibar, N., Hnatyshyn, S., Zhang, H., Clayton, T. A., Cantor, G. H., Sanders, M., Coen, M., Lindon, J. C., Holmes, E., Nicholson, J. K. & Lehman-Mckeeman, L. 2011. Urinary metabolites of 2bromoethanamine identified by stable isotope labelling: evidence for carbamoylation and glutathione conjugation. Xenobiotica, 41, 144-54. Shockcor, J. P., Unger, S. E., Wilson, I. D., Foxall, P. J., Nicholson, J. K. & Lindon, J. C. 1996. Combined HPLC, NMR spectroscopy, and ion-trap mass spectrometry with application to the detection and characterization of xenobiotic and endogenous metabolites in human urine. Anal Chem, 68, 4431-5. Soga, T., Baran, R., Suematsu, M., Ueno, Y., Ikeda, S., Sakurakawa, T., Kakazu, Y., Ishikawa, T., Robert, M., Nishioka, T. & Tomita, M. 2006. Differential metabolomics reveals ophthalmic acid as an oxidative stress biomarker indicating hepatic glutathione consumption. J Biol Chem, 281, 16768-76. Spraul, M., Freund, A. S., Nast, R. E., Withers, R. S., Maas, W. E. & Corcoran, O. 2003. Advancing NMR sensitivity for LC-NMR-MS using a cryoflow probe: application to the analysis of acetaminophen metabolites in urine. Anal Chem, 75, 1536-41. Spraul, M., Hofmann, M., Lindon, J. C., Farrant, R. D., Seddon, M. J., Nicholson, J. K. & Wilson, I. D. 1994. Evaluation of liquid chromatography coupled with high-field 1H NMR spectroscopy for drug metabolite detection and characterization: the identification of paracetamol metabolites in urine and bile. NMR Biomed, 7, 295-303. 31 Sun, J., Schnackenberg, L. K. & Beger, R. D. 2009. Studies of acetaminophen and metabolites in urine and their correlations with toxicity using metabolomics. Drug Metab Lett, 3, 130-6. Sun, J., Schnackenberg, L. K., Holland, R. D., Schmitt, T. C., Cantor, G. H., Dragan, Y. P. & Beger, R. D. 2008. Metabonomics evaluation of urine from rats given acute and chronic doses of acetaminophen using NMR and UPLC/MS. J Chromatogr B Analyt Technol Biomed Life Sci, 871, 328-40. Trygg, J., Holmes, E. & Lundstedt, T. 2007. Chemometrics in metabonomics. J Proteome Res, 6, 469-79. Want, E. J., Coen, M., Masson, P., Keun, H. C., Pearce, J. T., Reily, M. D., Robertson, D. G., Rohde, C. M., Holmes, E., Lindon, J. C., Plumb, R. S. & Nicholson, J. K. 2010a. Ultra performance liquid chromatography-mass spectrometry profiling of bile acid metabolites in biofluids: application to experimental toxicology studies. Anal Chem, 82, 5282-9. Want, E. J., Masson, P., Michopoulos, F., Wilson, I. D., Theodoridis, G., Plumb, R. S., Shockcor, J., Loftus, N., Holmes, E. & Nicholson, J. K. 2013. Global metabolic profiling of animal and human tissues via UPLC-MS. Nat Protoc, 8, 17-32. Want, E. J., Wilson, I. D., Gika, H., Theodoridis, G., Plumb, R. S., Shockcor, J., Holmes, E. & Nicholson, J. K. 2010b. Global metabolic profiling procedures for urine using UPLC-MS. Nat Protoc, 5, 1005-18. Waters, N. J., Waterfield, C. J., Farrant, R. D., Holmes, E. & Nicholson, J. K. 2006. Integrated metabonomic analysis of bromobenzene-induced hepatotoxicity: novel induction of 5-oxoprolinosis. J Proteome Res, 5, 1448-59. Wilson, I. D. & Nicholson, J. K. 1988. Solid phase extraction chromatography and NMR spectroscopy (SPEC-NMR) for the rapid identification of drug metabolites in urine. J Pharm Biomed Anal, 6, 151-65. Winnike, J. H., Li, Z., Wright, F. A., Macdonald, J. M., O'connell, T. M. & Watkins, P. B. 2010. Use of pharmaco-metabonomics for early prediction of acetaminophen-induced hepatotoxicity in humans. Clin Pharmacol Ther, 88, 45-51. Woolbright, B. L., Mcgill, M. R., Staggs, V. S., Winefield, R. D., Gholami, P., Olyaee, M., Sharpe, M. R., Curry, S. C., Lee, W. M. & Jaeschke, H. 2014. Glycodeoxycholic Acid Levels as Prognostic Biomarker in Acetaminopheninduced Acute Liver Failure Patients. Toxicol Sci. Yamazaki, M., Miyake, M., Sato, H., Masutomi, N., Tsutsui, N., Adam, K. P., Alexander, D. C., Lawton, K. A., Milburn, M. V., Ryals, J. A., Wulff, J. E. & Guo, L. 2013. Perturbation of bile acid homeostasis is an early pathogenesis event of drug induced liver injury in rats. Toxicol Appl Pharmacol, 268, 7989. 32 Abbreviations: APAP, Acetaminophen, paracetamol, N-acetyl-p-aminophenol ALF, acute liver failure ALT, alanine aminotransferase APAP-G, APAP-glucuronide APAP-CG, APAP-cysteinyl-glycine APAP-Cys, APAP-L-cysteinyl APAP-NAC, APAP-N-acetyl-L-cysteinyl APAP-S, APAP-sulfate AST, aspartate aminotransferase; BSO, buthionine sulfoximine CE, capillary electrophoresis CV, coefficient of variation COMET, Consortium for Metabonomic Toxicology COSY, correlation spectroscopy CYP450, cytochrome P450 DEM, diethylmaleate GCS, gamma-glutamylcysteine synthetase GC, gas-chromatography GLDH, glutamate dehydrogenase GSH, reduced glutathione GSSG, oxidized glutathione HLM, human liver microsomes HILIC, Hydrophilic interaction chromatography IP, intra-peritoneal LC, liquid-chromatography MAS, magic angle spinning MHS, mean histology score MS, mass spectrometry NAPQI, N-acetyl-p-benzoquinone imine NMR, nuclear magnetic resonance spectroscopy O-PLS-DA, orthogonal-projection on latent structures discriminant analysis OA, ophthalmic acid PAPS, 3’-phosphoadenosine-5’-phosphosulfate PCA, principal components analysis PLS, partial least squares PPAR-, peroxisome proliferator-activated receptor alpha QC, quality control ROS, reactive oxygen species RP-LC, reversed-phase liquid chromatography STOCSY, statistical total correlation spectroscopy TOCSY, total correlation spectroscopy HMBC, Heteronuclear Multiple Bond Correlation HSQC, Heteronuclear Single Quantum Correlation UGT, UDP-glucuronosyltransferase UPLC–MS, ultra-performance liquid chromatography–mass spectrometry 5-OP, 5-Oxo-proline 33 Figure 1 Figure 2 34 Figure 3 Figure 4 35 Figure 5 36 Figure 6 Figure 7 37 Figure Legends Figure 1: Typical experimental UPLC-MS based workflow for urine samples, including quality control (QC) sample preparation and data analysis. CV, coefficient of variation; PCA, principal components analysis; QC, quality control; UPLC-MS, ultra-performance liquid chromatography coupled with mass spectrometry. Adapted from (Want et al., 2013) Figure 2: Scheme of hepatic acetaminophen (APAP) metabolism. (Nelson, 1982) Figure 3: 600 MHz 1H NMR spectrum of an aqueous-soluble liver extract from a control and APAP-treated C57BL/6 mouse (300 mg/kg, ip) at 2 hours post-treatment revealing the presence of APAP metabolites (red) and numerous endogenous metabolites representing a wide chemical space (unpublished data). APAP, acetaminophen Figure 4: Statistical total correlation spectroscopy (STOCSY): (A) one-dimensional (1D) and (B) two-dimensional (2D) STOCSY correlation/covariance plots of a urinary NMR data set. Here, lineshapes are calculated by covariance ([−∞,∞]) while colors are set by correlation ([−1,1]). One-dimensional STOCSY plots (A) are traces of the two-dimensional STOCY (B, black box) at a given chemical shift taken from the “driver” peak. For the maxima of the doublet of 3-hydroxybutryic acid at 1.2 ppm (“driver” peak), high positive correlation coefficients are both sensitive and specific indicators of structural connectivity, and “pathway” connectivities show mostly negative correlations. For other metabolite signals seen in the 2D STOCSY, high positive correlations such as those between lactate (1.33 ppm), alanine (1.48 ppm), and glucose (∼3.5–4 ppm) indicate coordinated excretion rather than structural relationships. From (Robinette et al., 2013) Copyright approved. Figure 5: Hepatic metabolic changes induced by APAP (2 hours post-dose in male C57BL/6 mice) and identified through a CE-TOF-MS metabolic profiling study. Metabolic perturbations are mapped onto the glutathione biosynthesis pathway. (Soga et al., 2006) Copyright approved. Figure 6: Time-dependent changes in wild-type and Cyp2e1-null mice following 400 mg/kg APAP treatment and comparison of the biomarkers of APAP toxicity. Serum and liver samples were collected at 0, 0.5, 1, 2, 4, 8, 16 and 24 hours after APAP treatment. A, Scores plot of PCA analysis on serum metabolomes. Details of data acquisition, processing and model construction were described in the Experimental procedures. Each data point represents the average of 4-8 samples in each sample group (wild-type mice: • and Cyp2e1null mice: ○). The timing of sample collection was labeled beside the data point. The t[1] and t[2] values represent the scores of each sample group in principal component 1 and 2, respectively. Fitness (R2) and prediction power (Q2) of this PCA model are 0.388 and 0.251, respectively. B, Quantitation of serum palmitoylcarnitine level in wild-type and Cyp2e1-null mice (mean ± SD, n=4 mice/group). Palmitoylcarnitine levels in serum was measured using the multiple reactions monitoring mode in LC-MS. [2H3]palmitoylcarnitine was used as internal standard. C, Time course of AST activity in wild-type and Cyp2e1-null mice (mean ± SD, n=4). D, Time course of hepatic glutathione level in wild-type and Cyp2e1-null mice (mean ± SD, n=4). Glutathione level in liver was measured using the multiple reactions monitoring mode in LC-MS. From (Chen et al., 2009) Copyright approved. APAP, acetaminophen; AST, aspartate transaminase; LC-MS, liquid chromatography coupled with mass spectrometry; PCA, principal component analysis. 38 Figure 7: Pre-dose discrimination of the degree of liver damage obtained in paracetamoldosed rats. a, A scores plot from PCA of the pre-dose NMR data. Each point represents a single rat and is colour-coded by its histology class (with increasing severity of damage, class 1 is green, class 2 is blue, class 3 is red; see Table 1). b, Plot of mean histology score (MHS) versus the PC score obtained from the above PCA, with colour-coding as before. c, A scores plot from PCA of the pre-dose NMRdata for rats in histology classes 1 and 3. Each point represents a single rat,with colour-coding as before. d, A loadings plot corresponding to c, showing the variables making the largest contributions to PC2, and the direction of each contribution. Individual 0.04 p.p.m.-wide spectral segments are identified by the chemical shifts at their midpoints, and variables corresponding to particular compounds are identified by name. Tau, taurine; Citr, citrate; Oxog, 2-oxoglutarate; TMAO, trimethylamine-N-oxide; Bet, betaine. ‘2Tau’ indicates doubling of the Tau values. From (Clayton et al., 2006) 39