final1-marie-curie-final-report
advertisement

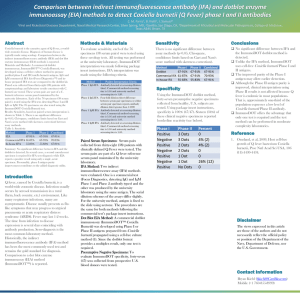
PROJECT FINAL REPORT Grant Agreement number: PCIG09-GA-2011-293731 Project acronym: Q-SCREEN Project title: Large-scale identification of Coxiella burnetii virulence factors Funding Scheme: Period covered: from 03/2011 to 03/2014 Name of the scientific representative of the project's co-ordinator1, Title and Organisation: Matteo Bonazzi, Group Leader, UMR5236 CPBS, CNRS Tel: 33 (0) 434359459 Fax: 33 (0) 434359414 E-mail: matteo.bonazzi@cpbs.cnrs.fr Project websiteError! Bookmark not defined. address: 1 Usually the contact person of the coordinator as specified in Art. 8.1. of the Grant Agreement. 4.1 Final publishable summary report This section must be of suitable quality to enable direct publication by the Commission and should preferably not exceed 40 pages. This report should address a wide audience, including the general public. The publishable summary has to include 5 distinct parts described below: An executive summary (not exceeding 1 page). A summary description of project context and objectives (not exceeding 4 pages). A description of the main S&T results/foregrounds (not exceeding 25 pages), The potential impact (including the socio-economic impact and the wider societal implications of the project so far) and the main dissemination activities and exploitation of results (not exceeding 10 pages). The address of the project public website, if applicable as well as relevant contact details. Furthermore, project logo, diagrams or photographs illustrating and promoting the work of the project (including videos, etc…), as well as the list of all beneficiaries with the corresponding contact names can be submitted without any restriction. Executive summary In the last decade, cellular microbiology has stressed the importance of studying pathogens in relation to their host. However, the effective, global identification of bacterial virulence determinants and their characterization require the development of new, automated approaches. With this project, we have set up protocols for the multi-phenotypic screen of bacterial factors that are involved in host cell invasion and colonization. Our approach integrates transposon mutagenesis, genomics, bioinformatics and fluorescence-based functional assays that have been adapted for the large-scale identification of virulence factors from virtually any intracellular bacterium. The advantage of our screening technique lies in the possibility of analyzing every bacterial mutations for multiple phenotypes, such as 1) internalization within the host/cell; 2) intracellular replication and 3) cytotoxicity, simultaneously. The emerging bacterial pathogen Coxiella burnetii is an excellent model system to apply our strategy. To date, very little is known about the bacterial factors that regulate Coxiella interactions with their host and previous in silico identification of putative Coxiella virulence factors provides an excellent database to cross-reference bioinformatics analysis with our functional assays. With our proof-of-concept screen we have generated and investigated over 1000 Coxiella mutations and identified several bacterial proteins involved in the key steps of host cells colonization. Among these, we have identified the product of the Coxiella gene CBU_1260 as the first Coxiella invasin. Mutations of CBU_1260 severely affected Coxiella internalization and replication within host cells. Predictive analysis on the primary sequence of CBU_1260 revealed the presence of an OmpA-like domain and 4 unstructured loops exposed at the bacterial surface. Membrane fractionation experiments showed that Coxiella OmpA is indeed enriched in the outer membrane of Coxiella and by replacing each extracellular loop with a myc tag, we showed that loop 1 is essential for internalization. Importantly, perturbing the interactions between OmpA and a yet unidentified receptor at the surface of host cells effectively blocked Coxiella internalization. Finally, we have developed non-mammalian animal models to validate the role of Coxiella virulence determinants in vivo. Using Galleria mellonella larvae, we effectively reproduced the OmpA mutant phenotypes observed in cultured cells, demonstrating an essential role of the Coxiella invasin in developing a systemic infection. In summary, multi-phenotypic screening of host/pathogen interactions is an efficient method for the study of infectious diseases. We have applied this method to Coxiella infections and identified a bacterial protein that is essential for Coxiella internalization within non-phagocytic cells. Understanding how intracellular bacteria adhere to and invade their host is essential to 1) understand the cell biology of infection and identify the candidate targets of anti-infectious molecules and 2) to develop targeted vaccines. Of note, bacterial OmpA proteins are considered as new pathogen-associated molecular patterns (PAMPs) and are among the most immunodominant antigens in the outer membrane of Gram-negative bacteria. We are currently investigating the possibility of using OmpA to develop the first synthetic vaccine against Q fever (patent pending: EP 13005536.1). Project context Coxiella burnetii is an obligate intracellular, Gram-negative bacterium, responsible of the worldwide neglected zoonosis Q fever. Acute forms of the disease are characterized by a chronic fatigue syndrome and weight loss, while chronic forms cause severe respiratory distress, hepatitis, endocarditis, miscarriage and neonatal death. Coxiella has the capacity to produce spore-like forms, highly resistant to heat and disinfection, which account for Coxiella persistence in the environment. This, together with its extremely high infectivity, makes of Coxiella a serious health concern, especially in rural areas where outbreaks are likely to occur and are accompanied by heavy economic burdens. The recent outbreak in the Netherlands saw the reported cases of Q fever exploding from 182 in 2007 to more than 2000 in 2009 and led to the slaughter of all pregnant goats in the farms. Moreover, the use of Coxiella as a bioweapon during and since World War II, has ascribed this pathogen among class B biothreats. Despite the obvious interest that Coxiella infections raise, its obligate intracellular nature has hampered the research activity due to the impossibility of genetic manipulation and growth in broth. To date, as little as three research groups actively investigate the cell biology of Coxiella infections and the only virulence factor identified is the bacterial lipopolysaccharide (LPS). Conversely, the intracellular replication cycle of Coxiella has been fairly well characterized and a number of host proteins have been reported to take part in such process. The recent characterization of a specific medium that allows axenic growth of Coxiella opened countless possibilities for its genetic engineering, hence the detailed characterization of Coxiella pathogenesis. A relevant number of outbreaks in the last decade ascribed Q fever among emerging (or reemerging) zoonosis and stressed the need for a deep characterization of Coxiella pathogenesis. However, as mentioned above, despite the health and economic impact that accompany Coxiella infections, very little is known about this pathogen, mainly due to the technical difficulties linked to its obligatory intracellular lifestyle. The sequencing of Coxiella burnetii has revealed a number of genes encoding potential virulence factors and the close relationship between Coxiella and Legionella pneumophila has allowed to use Legionella as a surrogate host to screen these candidates for T4SS-dependent secretion. However, lacking a method of gene inactivation, molecular Koch’s postulates are impossible to fulfill for these putative virulence factors. Today, axenic growth of Coxiella allows the use of well-known screening techniques to identify and characterize virulence factors. We thus propose to generate a bank of mutants of Coxiella burnetii and to set up the first high-throughput screen of Coxiella burnetii virulence factors. This technique will provide an unbiased approach to the identification of virulence factors that will allow the identification of unsuspected genes encoding for proteins with novel function, implicated in the remarkable adaptation of Coxiella to the host cell environment. Indeed, the bioinformatic approaches adapted so far are based on sequence homology with genes of other known bacterial pathogens that are nevertheless characterized by a different intracellular replicative cycle. The approach we propose will of course lead to the isolation and characterization of genes homologous to related pathogens that would result from a bioinformatic analysis. Besides contributing to the characterization of such genes of interest, this subset of data could be used to validate the high-throughput hits. In addition, a global screen for Coxiella virulence factors will lead to the identification of a large number of candidate genes, identifying our group as a source of data that could be investigated together with other teams in the field of cellular microbiology, thus generating potential collaborations. The aim of this project is the large-scale identification and characterization of Coxiella virulence factors. This will be achieved by generating a bank of Coxiella burnetii mutants by transposon mutagenesis, and by setting up a robust high-throughput microscopy-based screen to identify bacterial proteins involved in the intracellular replicative cycle of Coxiella. The emergence of an increasing number of bacterial strains that are resistant to antibiotic treatments has underlined the importance of studying how pathogens interact with host cells. This will allow the development of more specific therapies to fight infections. In parallel, the use of pathogens as a model system to study host cell functions has proven fundamental for remarkable advances in our knowledge of cell biology. Understanding the cell biology of Coxiella infections will be pivotal for the development of novel diagnostic and therapeutic strategies as well as to develop targeted vaccines for animal as well as human use. In addition, Coxiella remarkable adaptation to the lysosomal environment could provide interesting insights in the field of cellular microbiology. Project Objectives Generation of a Coxiella bank of mutants by transposon mutagenesis Transposon mutagenesis has been successfully employed to identify virulence factors of several bacterial pathogens, including Campylobacter jejuni, Francisella tularensis, Legionella pneumophila and Listeria monocytogenes. The Himar1 transposon has been optimised by the group of Dr. Heinzen at NIH Rocky Mountain Laboratories (RML, MT), and preliminary experiments showed the efficacy of such tool to generate mutants in Coxiella (9). Furthermore, the modified transposons contain either a GFP or an mCherry fluorescent tag, which will facilitate further analysis of mutants by imaging techniques. All experiments will be performed on Coxiella burnetii Nine Mile Phase II Reference Strain A439 clone 4. Despite being as infective as Nine Mile Phase I and follow the same intracellular replication cycle when used to infect cultured cells, this specific clone has been demonstrated to be totally avirulent, due to a non reversible, spontaneous mutation in the genes coding for the bacterial LPS (1). Consequently, the Center for Disease Control (CDC) has agreed to exempt this clone from the list of Select Agents to which Coxiella burnetii Phase I belongs. In addition, due to its attenuation, the CDC has authorised the manipulation of Nine Mile Phase II Reference Strain A439 clone 4 in a Biosafety Level 2 environment. This would be an additional great advantage once these regulations will be recognised within the EU. However, at present bacteria will be solely manipulated in a Biosafety Level 3 environment until further notice. High throughput screen of Coxiella mutants The development of a synthetic culture medium for the axenic cultures of Coxiella burnetii will allow the isolation of mutant clones by colony picking on Agar plates. Axenic bacterial amplification will automatically exclude mutations in genes involved in metabolic pathways (hence not necessarily involved in host-pathogen interactions) by lack of colony growth. All isolated colonies will be subjected to PCR amplification and sequencing to locate the site of insertion of the transposon and to verify the clonal nature of the isolate. Mutants will be then subjected to a two-step screen based on fluorescence imaging techniques. Mutants will be used to infect epithelial cells in 96-well plates. Vero and HeLa cells have already been successfully used in several studies on Coxiella infections and thus represent a suitable cell line for our high-throughput assay. The presence of an mCherry tag on the transposon and the typical growth of Coxiella in a large parasitophorous vacuole will be exploited to monitor the growth curve of every mutant following the variations of fluorescence accompanying the intracellular replication of Coxiella. The growth curve of every mutant will be compared to that of mCherry-tagged wild type bacteria and significant variations will be indicative of potential mutants of interest. This technique has been already proven successful to study the intracellular replication of Legionella pneumophila (10) that, similarly to Coxiella, replicates in a large vacuole and presents several advantages compared to RT-PCR, the current method used to assess Coxiella growth within host cells. First, imaging allows the repeated acquisition of data from the same sample, which reduces the overall number of samples and reduces sample-to-sample variability. The growth curve data obtained by these techniques will be then verified by RT-PCR on a selected number of mutants, as this method is currently used to assess Coxiella growth within host cells. Mutants selected in the first screen will be used to infect a set of epithelial cells (and occasionally macrophages) stably expressing a number of typical markers of the intracellular cycle of Coxiella (1) in order to have a gene-to-pathway correlation for every mutant (see below for the details of each screen). The development of state-of-the-art fluorescent microscopes allows nowadays the rapid and automated acquisition of high-resolution images from cells cultured on surfaces as small as 0.107 cm2 on 383-well plates. These systems can be adapted for both wide field and confocal microscopy depending on the specific needs and allow the rapid screen of a large number of either fixed or live samples. In addition, automated data acquisition will be coupled to robust and reliable analysis softwares developed for the unbiased quantification of images derived from high-throughput imaging (For details on access to automated microscopy and analysis software see section B4.2). Identification of virulence factors 1) Cell adhesion and internalisation phenotypes screen Previous studies showed that during internalisation, Coxiella recruits αvβ3 integrins at the cell interaction site (11, 12). Macrophages stably transfected with fluorescent αvβ3 integrins will be used to screen for Coxiella mutants unable to recruit such proteins. The isolation of mutants that fail to be internalised in macrophages will allow the identification of the bacterial proteins involved in host-pathogen interaction. The isolation and purification of such bacterial proteins will in turn facilitate the identification of bacterial receptors on the surface of epithelial cells. In parallel, internalisation screens will be carried out on integrin-deficient epithelial cells. As Coxiella is able to invade Vero cells that do not express αvβ3 integrins, mutants that fail to be internalised by Vero cells will be used to identify additional Coxiella receptors at the host cell surface. 1) Phagosome maturation phenotype screen Following bacterial internalisation, the maturation of Coxiella-containing vacuoles is accomplished through several steps. Metabolically active Coxiella recruits a series of endosomal markers such as LC3, Rab5, Rab7 and cathepsin D (13), eventually leading to the formation of a parasitophorous vacuole (PV) in which bacterial replication occurs. Furthermore, it has been shown that the PV membranes are enriched in cholesterol and contain the lipid-raft marker flotilin-1 (14). Epithelial Vero and HeLa cells stably expressing GFP-tagged LC3, Rab5, Rab7, cathepsin D and flotilin-1 will be infected with Coxiella mutants and the recruitment of the different endosomal markers will be monitored by fluorescent microscopy on either fixed or live samples. The fact that Coxiella protein synthesis is required for phagosome maturation strongly suggests that effectors secreted through the type 4 secretion system (T4SS) play an important role in this phenotype. Mutation of these effector proteins will allow us to identify their role in the phagosome maturation process. 1) Antiapoptotic phenotype screen Due to its relatively slow replication cycle, metabolically-active Coxiella inhibits apoptosis in infected cells to prolong their survival (15). However, Coxiella effector proteins involved in this process are still unidentified. FACS sorting and apoptosis ELISA kits will allow us to screen for mutants that fail to protect macrophages from chemically-induced apoptosis. By FACS, infected cells can be sorted by means of the mCherry signal expressed by the Coxiella mutants, coupling this with a TUNEL assay will give readout of the infected cells that are undergoing apoptosis. Alternatively, several ELISA kits, based on the release of specific apoptotic markers such as cytochrome c, will be used to identify mutants that fail to prevent cell death. Characterisation of virulence factors The screen described above will originate a large set of data that will allow identification and classification of a large number of virulence factors. However, lowthroughput, well-established techniques for the study of host-pathogen interactions will be used on a subset of mutants for further characterisation. Their genes will be subcloned into relevant plasmids and used to screen human cDNA libraries for potential host partners. Interaction between bacterial effectors and host proteins will be confirmed using biochemical methods such as co-immunoprecipitation, far Western blot and co-transfection. Main results Stage n.1 Laboratory setup and the establishment of a work plan This part of the work has been successfully carried out as planned within the first semester of funding. All the essential equipment has been acquired between March and May of year 1 and additional small equipment has been acquired afterwards, according to our needs. At the time of submission of the present project, the manipulation of Coxiella burnetii phase II, which we use as a model for our research, was restricted to bio-safety level 3 environments and Coxiella burnetii was listed among the highly dangerous microorganisms and toxins (MOT, equivalent of Select Agents in the US) in France. Since then, we have been discussing with the two French organization that regulate the manipulation of pathogens and genetically modified organisms at the national level: 1) the Agence Nationale de Securité du medicament et des Produits de Santé (ANSM, web: ansm.sante.fr) and 2) the Génie Génétique (web: www.enseignementsup-recherche.gouv.fr). We have been officially authorised to manipulate Nine Mile Phase II clone 4 (NMIIC4) Coxiella in a bio-safety level 2 environment (Dossier Génie Génétique n.5923) and Coxiella burnetii has been excluded from the list of MOT (Select Agents) in France. Stage n.2 Tools setup and protocols adaptation This part of the work has been very complex and took longer than expected. However, it has been carried out within the first year of funding. From our collaborators at Rocky Mountain Laboratories, we have obtained the reference Coxiella strain Nine Mile Phase II clone 4 (NMIIC4) and a variety of Coxiella-adapted expression vectors and transposon to use in our study. In particular, we have engineered a Himar1-based transposon system by inserting an eGFP gene upstream of the existing chloramphenicol resistance cassette to obtain fluorescent Coxiella mutants. Differently from what we have previously planned, we have optimized an assay protocol that allows to rapidly quantify the concentration of bacteria in a 96-well plate format using the Quant-iT PicoGreen dsDNA assay (Invitrogen) instead of RT-PCR. This approach is less expensive and more reliable than RT-PCR and it has been now adopted by other laboratories working on Coxiella. We also setup a single-primer colony PCR approach to identify the transposon insertion site of each isolated Coxiella mutant. Our technique allows the amplification of fragments of variable size, all including a 278 bp region upstream of the 3' Inverted Terminal Repeat (ITR) of the inserted transposon. The amplified fragments are then sequenced (by Beckman Coulter, UK) using a specific internal primer and the obtained sequences were aligned on the Coxiella burnetii RSA493 annotated genome using automated sequence analysis software (MacVector, NC, USA). Concerning the generation of stable cell lines expressing typical markers of the Coxiella replicative vacuole, we have used a transduction system to produce non-replicative lentiviral particles carrying mCherry-tagged versions of Rab5, Rab7, Rab11, Lamp-1, CathepsinD and M6PR. Finally, we have developed a FileMaker-based database where all data from our collection of mutants are stored and accessible by the team members. Of note, this database is compatible with web publication for future divulgation of our data. Stage n.3 Generation of a Coxiella bank of mutants by transposon mutagenesis To identify the Coxiella factors that are involved in host-pathogen interactions, we have undertaken the generation of a library of GFP-tagged bacterial mutants by transposon mutagenesis as proposed. To obtain stable mutants, Coxiella NMIIC4 were electroporated using a two plasmid system, where the transposase is encoded by a suicide plasmid that is lost during bacterial replication. The GFP-tagged Coxiella mutants thus generated were grown on ACCMII agar plates in the presence of chloramphenicol, isolated and amplified in ACCMII, always in the presence of chloramphenicol. The Coxiella genome contains 1847 coding sequences (CDS, 1852 in the bacterial chromosome and 31 in a cryptic plasmid. To date, we have isolated 3000 transposon mutants, 1120 of which have been sequenced, annotated and analyzed. Of these, 904 insertions were found within Coxiella annotated CDS and 216 in intergenic regions of the Coxiella genome. Frequency distribution analysis revealed that, overall, mutations occurred in 472 CDS on the Coxiella chromosome and 8 CDS on the QpH1 plasmid (corresponding to 20.3% and 20.5% of the total CDS present on chromosome and plasmid respectively). Transposon insertions were homogeneously distributed throughout the Coxiella chromosome and plasmid, with seven “hot spots” of preferential transposon insertion. Of note, ‘hot spot” n.7 corresponds to the locus that hosts T4SS core genes (dot/icm genes) which are fundamental for host-pathogen interactions. Stage n.3 High/medium/low-throughput screen of Coxiella mutants High throughput screen of Coxiella mutants Each isolated transposon mutant was used to infect epithelial Vero cells cultured in 96-wells plates triplicates. Non-infected Vero cells were used as negative control whereas cells infected with GFP-NMIIC4 were used as positive controls. To identify mutations that affect Coxiella infections, we followed the variations of GFP fluorescence associated with intracellular bacterial growth over 6 days of infection using a micro-plate reader. At 6 days post infection, triplicate plates were fixed in paraformaldehyde, incubated with Hoechst, and imaged using an automated fluorescence microscope. Six fields/well were imaged using a 20X objective in the phase contrast, GFP and Hoechst channels, for an average of approximately 12000 host cells imaged for each bacterial mutant infection. Images were then analyzed using CellProfiler (www.cellprofiler.org) and 15 morphological features were extrapolated from each cell. Host cell nuclei identification and morphology was used to assess the potential cytotoxicity of Coxiella mutations. The morphology (size, shape, granularity index, compactness, etc.) and the fluorescent intensity of GFP-Coxiella colonies were used to score the intracellular replication of bacteria. The number of Coxiella colonies was then divided by the number of identified host cell nuclei to estimate the efficiency of bacterial internalization within cells. To validate our assay, we analyzed the growth curves and morphology of 6 Coxiella mutants carrying independent transposon insertions in the gene CBU_1648 coding for DotA, a T4SS core protein that had previously been reported to be essential for bacterial replication within host cells. All dotA mutations severely inhibited intracellular bacterial growth, as compared to wt GFP-Coxiella, during the 6 days of infection. Morphological analysis indicated a strong reduction in the average size of intracellular Coxiella colonies and an increased number of colonies/cell. This latter phenotype may result from the loss of T4SS functionality, which affects the fusogenicity of Coxiella-containing vacuoles. Our control strain GFP-NMIIC4 carries the GFP and chloramphenicol resistance cassettes within a miniTn7 transposon, which is different from the Himar1-based transposon used to generate our bank of mutants. Hence, we have identified 3 Coxiella mutants that carry Himar1-based transposon insertions in intergenic regions of the genome and whose phenotype was indistinguishable from either GFP-NMIIC4 or NMIIC4. These have been used to implement our controls. To identify Coxiella mutations that perturbed host cell invasion and intracellular replication, we plotted the average colony size of mutants against the average number of colonies/cell. Statistical analysis was used to define regions in the scatter charts corresponding mild (z-score ≤ -2) and severe (Z-score ≤ -4) phenotypes. The 1120 analyzed Coxiella mutants were found in 3 welldefined clusters: one cluster included mutants whose phenotype did not vary significantly from that of GFP-NMII and the control mutant 1832. A second cluster was clearly shifted towards a reduction in the size of Coxiella colonies and an increase in the average number of Coxiella colonies/cell. We ascribed to this cluster mutations that affect Coxiella intracellular replication without affecting host cell invasion. Finally, a third cluster was shifted towards a reduced number of colonies/cell, indicating mutations that affect either host cell invasion or survival within infected cells. To identify Coxiella mutants that are potentially involved in protecting of the host cell from apoptosis, the average size of Coxiella colonies was plotted against the total number of host cells surviving the 6 days infection. Doing so, we have identified 7 mutations that are particularly detrimental to host cell survival. For the purpose of our study, we focused our analysis on 1) dot/icm genes, 2) hypothetical proteins with domains potentially involved in host-pathogen interactions and 3) hypothetical proteins without known domains. Intergenic transposon insertions were also retained to identify potential non coding RNA (ncRNAs) involved in Coxiella infections. Cell adhesion and internalization phenotypes screen As an obligate intracellular pathogen, Coxiella invasion of host cells is a priming step of the infection. We were therefore particularly interested in bacterial factors putatively involved in host cell adhesion and invasion. CBU_0053 and CBU_0915 encode for enhA.1 and enhB.1, which are homologues of the respective Legionella pneumophila genes implicated in bacterial uptake by host cells. However, mutants in these genes were affected in intracellular bacterial replication, suggesting an implication in different processes as compared to Legionella infections. Five independent transposon insertions in a gene coding for an hypothetical protein with a predicted Outer Membrane Protein A-like domain (OmpA-like domains) exhibited a strong reduction in the number of Coxiella infected cells, which was also accompanied by a decrease in the size of intracellular Coxiella colonies. Accordingly, growth curve analysis of the 5 transposon mutants revealed a strong reduction of GFP fluorescence during the 7 days of infection. We further investigated this gene, which we named cip1 (Coxiella internalization protein 1) to assess its role in Coxiella adhesion/internalization. cip1 is a 747 bp putative gene on the + strand of the Coxiella chromosome and it encodes a putative protein of a predicted size of 23 kDa. cip1 is not part of an operon, indicating that the phenotype observed for the 5 mutants was indeed due to the inactivation of cip1 alone. Sequence analysis indicated that transposon insertions occurred in the distal part of the CDS, with mutants Tn27 and Tn907 presenting insertions at the same site. The presence of the transposons and their approximate positioning within the CDS were validated by PCR for the 5 isolated mutants. Sequence analysis using the Protein Homology/analogY Recognition Software (Phyre, web: http://www.sbg.bio.ic.ac.uk) identified the 8 beta barrels transmembrane domain which is typical of OmpA-like domain proteins, an intracellular N terminal alpha helix and 4 unstructured loops predicted to be exposed at the cell surface. The extracellular domain was used to raise an anti-Cip1 antibody and verify that indeed this CDS encodes a protein. By Western blot, our anti-Cip1 antibody recognized a band of the expected size of 23 kDa from NMII bacterial lysates. Importantly, this band was missing from all the lanes corresponding to the 5 transposon mutants in cip1. We then focused on a single mutant (Tn208) to investigate the role of this protein in Coxiella adhesion and invasion of host cells. First, we used a GFPprobe to confirms that Tn208 contained a single transposon insertions by Southern blot. Next, THP-1 macrophages and the epithelial cell line A431 were then challenged with either wt Coxiella, the control transposon mutant Tn1832 and the Cip1 mutant Tn208 for 15, 30, 45 and 60 minutes and for 5 days. Differential labeling of extracellular versus intracellular bacteria was used to assess the efficiency of Coxiella adhesion/internalization within host cells. THP-1 macrophages internalized all Coxiella strains with comparable efficiency, suggesting that active uptake of Coxiella by phagocytic cells is independent of Cip1. In non-phagocytic A431 cells however, we observed a marked reduction in the uptake of Tn208. This was due to the precise insertion of the transposon within cip1 as the control mutant Tn1832, with a transposon insertion in an intergenic region of the Coxiella chromosome was able to invade host cells with similar dynamics as compared to wt Coxiella. In addition, we observed that Tn208 still adhered to host cells even after thorough washing of samples in PBS before fixation. Finally, to determine whether Cip1 alone was sufficient to mediate Coxiella adhesion/internalization within host cells, we purified Cip1 and used it to coat latex beads. Indeed, Cip1 coating conferred adhesiveness and invasiveness to coated beads as compared to control, GST-coated beads. Conversely, pretreatment of host cells with purified Cip1 prior to infection effectively prevented Coxiella internalization, suggesting that Cip1 interacts with a cognate protein at the surface of host cells and that this interaction can be saturated. We are currently performing pull down assays using purified Cip1 in order to identify the eukaryotic receptor of Cip1. Phagosome maturation phenotype screen The enrichment of mutations in dot/icm genes prompted us to analyze this cluster to assess the relative contribution of T4SS core proteins to Coxiella pathogenesis and to further validate our assay. Coxiella has 26 dot/icm genes and so far we have isolated 41 Coxiella clones carrying single transposon insertions in 17 of these. First, we could confirm the previously reported observations that icmD, dotA and icmL.1 are essential for Coxiella replication within host cells. Our analysis indicated that 12 dot/icm genes (dotA, icmV, E, D, G, J, N, C, P, K, X, L.1) are essential for bacterial replication within the host, whereas mutations in dotB, icmB and icmS showed an intermediate phenotype which corresponded to partial intracellular replication as assessed by morphological analysis. Of note, the phenotypes observed are consistent among dot/icm genes predicted to be part of operons. The icmS phenotype is of particular interest because bacteria seem to replicate and form small colonies enclosed in many, isolated, Lamp-1 positive compartments that fail to coalesce into the classical large Coxiella replicative vacuole. In Legionella pneumophila, which shares with Coxiella a very similar T4SS, IcmS is a chaperone that mediates the secretion of a class of bacterial effectors. In Coxiella, IcmS may be involved in secreting factors involved in conferring fusogenicity to the bacterial replicative vacuole. This issue is being further characterized in collaboration with the laboratory of Robert Heinzen at Rocky Mountain Laboratories (MT, USA). We then focused our analysis on the cluster of 27 mutated CDS corresponding to hypothetical proteins with known domains, potentially involved in host-pathogen interactions. 17 of the retained CDS encode for proteins with predicted eukaryotic-like domains mediating protein-protein interactions. These include ankyrin-domains, coiled-coil domains and tetratricopeptide repeat (TPR). Ankyrin-domain-containing proteins (Anks) have been reported to mediate hostpathogen interactions at several steps of Legionella pneumophila infections. Genome sequencing of Coxiella revealed 15 ank genes (A, B, C, D, F, G, H, I, J, K, L, M, N, O, P) and AnkG has been shown to play a role in protecting the host cell from apoptosis during Coxiella infections. We have isolated mutations in 5 ank genes: ankA, B, F, K and P. Our analysis suggested that AnkA and AnkP are specifically involved in bacterial replication within host cells as 4 out of 5 transposon insertions in these genes resulted in a significantly smaller intracellular colonies. Mutations in AnkB and AnkF did not result in significant phenotypes whereas the phenotypic pattern of the 3 isolated mutants in AnkK was inconclusive and require further analysis. Transposon insertions in CBU_0530 and CBU_1780, which encode proteins with a TPR, resulted in marked intracellular replication phenotypes, whereas the transposon insertion in CBU_1366, which encodes a protein with a coiled-coil domain, is the only mutation in this cluster to produce a host cell survival phenotype. Interestingly, mutations in CBU_0381, CBU_0488 and CBU_1379, which encode hypothetical proteins involved in kinase signaling, resulted in a consistent phenotype of significantly smaller Coxiella colonies. Finally, of the 146 mutated CDS in the cluster of hypothetical proteins without known domains, 122 resulted in significant phenotypes which mostly concerned intracellular bacterial replication and bacterial invasion of host cells and will be further characterized to identify novel Coxiella T4SS effectors. Anti-apoptotic phenotype screen Our multi-phenotypic screen identified 7 transposon mutants that exhibited a strong cytotoxic phenotype when incubated with Vero cells. To further analyze the phenotype of these mutants, we investigated their intrinsic capacity of triggering apoptosis and their potential of protecting infected cells from staurosporine-induced apoptosis. To this aim, HeLa cells were either left unchallenged or incubated with wt Coxiella, the control transposon mutant Tn1832, the DotA mutant Tn270 and the 7 cytotoxic mutants (Tn881, Tn616, Tn946, Tn926, Tn1226, Tn1232, Tn1233). Three days post-inoculation, cells were either fixed in paraformaldehyde or incubated with 1μM staurosporine for 4 h prior to fixation. The percentage of apoptotic cells was then evaluated for each condition by the TUNEL assay. Very few TUNEL-positive cells were observed among untreated cells, these were increased to 50% of the total cell population upon staurosporine treatment. As expected, incubation of cells with wt Coxiella did not increase the number of TUNEL-positive cells as compared to untreated cells and wt Coxiellacolonized cells were efficiently protected from staurosporine-induced apoptosis. Cells challenged with the control transposon mutant Tn1832 presented the same phenotype as cells incubated with wt Coxiella and conversely, the DotA mutant Tn207 failed to protect infected cells from induced apoptosis. Mutant Tn881, which carries a transposon insertion in CBU_0485, exhibited a partial protection of infected cells from induced apoptosis whereas the remaining mutants failed to effectively protect cells from the effects of staurosporine. Interestingly, incubation of HeLa cells with mutants carrying transposon insertions in CBU_1639, CBU_1366 and CBU_0307a significantly increased the number of TUNELpositive cells also in the absence of staurosporine, indicating that these mutants may possess intrinsic cytotoxic properties. 4.2 Use and dissemination of foreground The novelty of the proposed research subject and the recent set up of the host laboratory, imply that a particular emphasis has been given to dissemination activities. Locally, the UMR 5236-CPBS organizes weekly internal and external work-in-progress seminars where every team presents and discuss recent data. In addition, the CPBS website (www.cpbs.cnrs.fr) represents each team in the institute and their members, with an adequate space to describe their research, recent advancements and publications. In addition, our team has set up their own website to give more emphasis on our research and increase our visibility. Our research has been presented by either myself or Dr. Martinez at national and international meetings such as EMBO courses and workshops (“Integrating omic approaches to host-pathogen interactions” held in Leeds, UK, in June 2013 and Subversion of Host Cellular Organization and Functions by Pathogens held in Villars-sur-Ollon, Switzerland, in May 2012), the American Society of Rickettsiology Meetings (Park City, Utah, 2012 and Portland, Maine, 2013), the American Society for Cell Biology meeting (San Francisco, California, December 2012), Club Exocytosis-Endocytosis meeting (La Grande Motte, France, April 2013) as well as in the context of several invited seminars and lectures. Importantly, the work supported by Marie Curie Actions has been recently published on PLoS Pathogens (March 2014). Publications Eric Martinez, Franck Cantet, Laura Fava, Isobel Norville and Matteo Bonazzi. Identification of OmpA, a Coxiella burnetii protein involved in host cell invasion, by multiphenotypic high-content screening. PLOS Pathogens 10.1371/journal.ppat.1004013. Isobel H Norville, Margaret G Hartley, Eric Martinez, Franck Cantet, Matteo Bonazzi, and Timothy P Atkins. Galleria mellonella as an alternative model of Coxiella burnetii infection. Microbiology. 2014 Mar 27. doi: 10.1099/mic.0.077230-0. [Epub ahead of print]. List scientific conferences for Eric Martinez 25-03-14: Selected speaker at the 5th meeting of the “host/microorganisms network”. Montpellier, France. 29-10-13: Invited speaker at the colloquium within the framework of the Marie Curie training network FishForPharma, Nîmes, France. 26-06-13: Selected speaker at the EMBO workshop “Integrating omic approaches to study host-pathogen interactions”, Liverpool, United Kingdom. 17-06-13: Invited lecturer at the Department of Microbiology and Immunology external seminar, McGill University, Montréal, Canada. 05-04-13: Selected speaker at the 16th Annual meeting of the Endocytose-Exocytose club, La Grande Motte, France. 26-10-12: Selected speaker at the INRA 5th Effectome meeting, Lauret, France. List scientific conferences for Matteo Bonazzi 28-10-13: Invited seminar at Biozentrum, Basel, Switzerland 16-06-13: Selected speaker at the American Society of Rickettsiology Meeting, Portland, (US-ME). 30-11-12: Invited seminar at Pasteur Institute, Lille, France. 16-11-12: Invited seminar at La Timone Hospital, Marseille, France. 30-7-12: Speaker at the American Society of Rickettsiology Meeting, Park City, (US-UT). 18-6-12: Invited seminar at Univeristy of Geneva School of Medicine, Geneva, Switzerland. 13-3-12: Invited seminar at Sanofi/Aventis, Toulouse, France. 21-2-12: Invited seminar at the Institute of Molecular Life Sciences, Zurich, Switzerland. 30-11-11: Speaker at the symposium on “Intracellular Trafficking and Membrane Dynamics”, Montpellier, France. 18-11-11: Invited speaker at the Eurobiomed Meeting, Inserm Transfert “journée d'échange académiques-industriels, maladie infectieuses”, Aix-en-Provence, France. 8-9-11: Invited speaker at the “Journées de l’Ecole Doctorale de Nice”, Nice, France. 18-4-11: Invited speaker at the “Montpellier Infectious Disease Network Talks”, Montpellier, France.