EBOLA ACTION CARD: IN-PATIENTS AND HEALTH CENTRES
advertisement

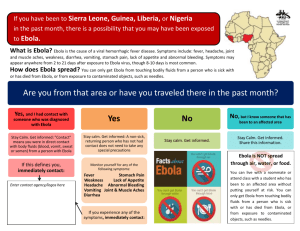
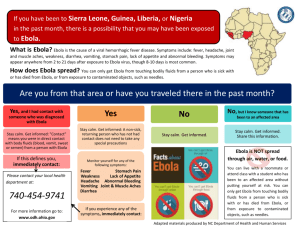
EBOLA ACTION CARD: IN-PATIENTS AND HEALTH CENTRES What to do if you suspect a patient or service user has Ebola: WHO IS THIS ACTION CARD AIM AT? This Action Card has been issued to provide LPT staff and receptionists with instructions on what to do in the event that a patient self presents at a hospital or health centre with Ebola like symptoms (see Identifying Suspected Ebola Patients box below). IDENTIFYING SUSPECTED EBOLA PATIENTS Do any of these conditions apply to the patient / service user? Ebola should be suspected in patients presenting to primary care services who have a fever of ≥37.5°C OR have a history of fever in the past 24 hours AND have recently visited any of the affected areas (Sierra Leone, Guinea and Liberia as of 25th November 2014) within the previous 21 days. OR Have a fever of ≥37.5°C OR have a history of fever in the past 24 hours AND have cared for/come into contact with body fluids of/handled clinical specimens (blood, urine, faeces, tissues, laboratory cultures) from an individual or laboratory animal known or strongly suspected to have VHF. INFECTION RISK Ebola is transmitted by direct contact with the blood or bodily fluids of an infected person (alive or dead). People infected with Ebola can only spread the virus to other people once they have developed symptoms, such as fever. Even if someone has symptoms, it’s important to remember that the virus is only transmitted by direct contact with the blood or body fluids of an infected person. The incubation period of Ebola ranges from 2 to 21 days. In the event of exposure to potentially infectious bodily fluids seek advice: In-hours: Contact the LPT Infection Control Team on 0116 2951668. Out of hours: Contact Public Health England on 0344 225 4524 Also contact your line manager / On-call Manager to inform them. 1 Amanda Hemsley, Senior Nurse Advisor – Infection Prevention and Control Kevin Robotham – Emergency Planning Manager V1 1 December 2014 ACTIONS TO FOLLOW WHAT TO DO IF A PATIENT PRESENTS TO A PREMISES IN PERSON Any patients that identify themselves to reception or clinical staff as being unwell with a fever and having visited an area affected by Ebola in the past 21 days should not sit in the general waiting room. These patients should be directed to and isolated in a side room. Refrain from contact but reassure the patient that medical assistance is on its way. All staff dealing with the patient should follow hand hygiene protocols. If necessary for LPT clinical staff to interact (But do not provide clinical interventions) with the patient, utilise personal protective equipment (PPE) (gloves, face mask and apron). Note: PPE Grab boxes are located in LPT sites where there is an Urgent Care Centre or Minor Injuries Unit. IF NO URGENT CARE CENTRE / MINOR INJURY UNIT / GP PRACTICE ON SITE. IF URGENT CARE CENTRE / MINOR INJURY UNIT / GP PRACTICE ON SITE. Contact the UCC / MIU / GP to inform them that a suspected Ebola patient is on site. IF NOT AVAILABLE Receptionist to alert LPT senior nurse / manager. Senior nurse / manager to Call 111 to seek advice. They should triage the patient to determine risk of Ebola. They will ask you a number of questions in order to establish the likelihood that the patient has Ebola. SUSPECTED EBOLA PATIENT ISOLATE IN A SIDE ROOM DEEMED AS NOT HAVING EBOLA SUSPECTED EBOLA PATIENT ISOLATE IN A SIDE ROOM UCC / MIU / GP may take over responsibility of patient. HOWEVER, FOLLOW ACTIONS ON FOLLOWING PAGES Treat the patient as a non-Ebola patient FOLLOW ACTIONS ON FOLLOWING PAGES 2 Amanda Hemsley, Senior Nurse Advisor – Infection Prevention and Control Kevin Robotham – Emergency Planning Manager V1 1 December 2014 PATIENT TRIAGED AS A SUSPECTED EBOLA PATIENT 111 / Urgent Care Centre will arrange for the transfer by ambulance of the patient to an acute hospital. The patient is to remain in isolation until arrival of the ambulance. Refrain from contact but reassure the patient that medical assistance is on its way. All staff dealing with the patient should follow hand hygiene protocols. If necessary for LPT clinical staff to interact (But do not provide clinical interventions) with the patient, utilise personal protective equipment (PPE) (gloves, face mask and apron). Note: PPE Grab boxes are located in LPT sites where there is an Urgent Care Centre or Minor Injuries Unit. A record should be taken of any patients, visitors or staff who was present and may have been exposed to bodily fluids. If the patient’s conditions deteriorate (vomiting, diarrhoea) having spoken to 111, alert 111 immediately. Inform the ambulance crew on their arrival. ALERT SENIOR MANAGERS / INFECTION CONTROL Inform your line manager (out of hours ensure the on call manager is informed). In hours - Inform LPT Infection Control Team on 0116 295 1668. Notify Public Health England on 0344 225 4524. USE OF ROOMS FOLLOWING SUSPICION OF EBOLA Once the suspected case has been transferred to an acute hospital, the room in which the patient has been isolated or any potentially contaminated areas should not be used until a diagnosis of Ebola has been excluded. If the diagnosis is confirmed, specific advice on decontamination must be sort from the LPT Infection Control Team (out of hours from Public Health England). if the patient has symptoms limited to fever with no vomiting or diarrhoea, then high contact surfaces such as door handles or touch screens should be wiped using standard disinfectants using standard precautions but the premises does not need to be closed The room in which the patient was isolated and the toilets if they have been used by the patient should not be used pending discussion with the LPT Infection Control Team or local Public Health England team. However, rest of the premises can be used. If the patient meets the criteria for a suspected case and has symptoms such has vomiting, diarrhoea and or bleeding. Close the affected area and contact LPT Infection Control Team (or Public Health England out of hours) for advice. Ensure the cleaning / domestic staff have been informed so that they do not clean up any waste bodily fluids until further advice is sought from LPT Infection Control Team or Public Health England. 3 Amanda Hemsley, Senior Nurse Advisor – Infection Prevention and Control Kevin Robotham – Emergency Planning Manager V1 1 December 2014 DEALING WITH SOILED CLOTHING If the patient spills bodily fluids on their clothing: Wear PPE (gloves, face masks, apron, eye protection). Leave a clinical waste bag and gown in room. Instruct them to place the soiled clothing in the clinical waste bag. Instruct them to put on the gown. If the patient has vomited, bled or had diarrhoea since alerting 111 or Urgent Care Centre / Minor Injury Unit, inform them immediately of the change in the patient’s condition. Inform the Ambulance Crew on their arrival of changes / deterioration in the patient’s condition, especially if potentiality infectious bodily fluids are present. The waste bag is to be left in the room (Inform the Ambulance Crew as they may need to take it with them). Otherwise leave in the room and seek advice from LPT Infection Control Team / Public Health England DECONTAMINATION OF ROOM Cleaning and decontamination of any rooms in which a patient suspected of having Ebola has been isolated, or any facilities used by the patient, should be discussed with the LPT Infection Prevention and Control Team (or out of hours with the Public Health England). Once the suspected case has been transferred to an acute hospital other patients and staff must not use the room in which the patient has been isolated or any potentially contaminated areas until they have been decontaminated. This includes toilets and other high contact surfaces such as door handles and telephones used by the suspected case. The full risk assessment and initial investigations at hospital may rapidly exclude Ebola (though may take at least 24 hours); at which point it may be clear that specific decontamination of the room is not required. The room must be quarantined if the patient is being tested for Ebola. If the diagnosis is confirmed, then specific advice on decontamination will be provided by the LPT Infection Prevention and Control Team or Public Health England. Public areas where the suspected case has passed through and spent minimal time in (such as corridors) but which are not visibly contaminated with bodily fluids do not need to be specially cleaned and disinfected. KEY CONTACT NUMBERS For the Public - NHS 111 111 LPT Infection Prevention and Control 0116 2951668 Public Health England 0344 225 4524 LPT Divisional On-Call Managers Via 0116 225 6000 4 Amanda Hemsley, Senior Nurse Advisor – Infection Prevention and Control Kevin Robotham – Emergency Planning Manager V1 1 December 2014