path 25 LO [5-6
advertisement
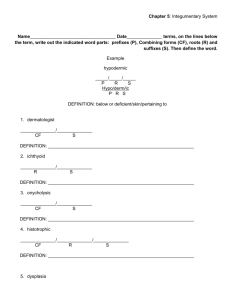
Chapter 25 The Skin 1. Review definitions on 1168 2. What are the two hypotheses for freckle formation? How are café au lait spots different? Focal abnormality in melanocytes Enhanced pigment donation to basal keratinocytes Neurofibromatosis spots have macromelanosomes in melanocytes 3. What does lentiginous mean? How are they different from freckles? Hyperpigmented basal cell layer Don’t darken in the sun 4. Why is melanocytic nevus a misnomer? What is the key feature of melanocytic nevus? 3 subcomponents? Look at the nevus pictures. Nevus=birthmark, but most nevi are acquired Maturation: deep nevus cells stop making pigment, grow in nerve-like fascicles (neuurotization) and have enzymatic changes (loss of tyroinase, acquisition of cholinesterase) 5. Why are many skin neoplasms dead ended? RAS or BRAF expression cause proliferation, but then causes permanent growth arrest 6. What skin lesion often becomes melanoma? Size? Appearance? 3 keys to Recognition? What causes the syndrome? Dysplastic nevi >5 mm Flat macules, pebbly papules, or targetoid lesions Variability, irregular borders, and occur in sun-protected areas; histo: lentiginous Dysplastic nevus syndrome is caused by AD mutations in CDK genes 7. How big are melanomas? 3 growth patterns? Develop from other stuff, usually recognized at 10 mm+ Lentigo maligna: slow growth on face Superficial spreading: most common Acral/mucosal: NOT related to sun exposure (wtf???) 8. What are the two groth phases and how do you quantify spread? What are 5 determinants of a favorable prognosis? What are two genes that are mutated (gets about 1 whole page)? Radial=> vertical growth phase; use Berslow thickness Depth less than 1.7 mm, few mitoses, brisk TIL response, absence of regression (?), female gender CDK (as in dysplastic nevi), BRAF and PTEN mutations cause increases in RAS and PI3K/AKT i. Non sun-exposed sites get c-KIT mutations 9. What is the Leser-Trélat sign? Paraneoplastic syndrome of many seborrheic keratoses, usually due to GI carcinomas 10. What do you call seborrheic keratoses on black people? What do seborrheic keratoses look like? Dermatosis papulosa nigra! That sounds kind of like a high-brow racist joke Pores impacted with keratin, velvety surface 11. What are the two types of acanthosis nigricans? When do each happen Most common is benign i. AD trait ii. Due to obesity, pituitary/pineal tumors, or diabetes iii. Also part of rare congenital syndromes Paraneoplastic i. Usually GI adenocarinomas 12. When do fibroepithelial polpys proliferate? Diabetes, obesity, pregnancy 13. Epithelial Cysts: describe (1) epidermal inclusion cyst, (2) pilar/trichilemmal cyst, (3) dermoid cyst,and (4) steocystoma simplex: Filled with strands of keratin Full of keratin and lipid Like epidermal inclusion cyst, plus appendages like hair follicles Wall resembles sebaceous gland duct i. Often inherited as part of steatocystoma multiplex (keratin mutation) 14. Describe the adnexal/appendage tumors below: Trichilemmomas – associated with Cowden syndrome (mutant PTEN) Eccrine poroma – palms and soles Cylindroma – forehead = turban tumor Syringoma – lower eylides, eccrine differentiation Sebaceous adenoma – associated with malignancy in Muir Torre syndrome (HNPCC) Pilomatriocomas –follicular differentiation Sebaceous carcinoma – eyelid, malignant 15. Which dysplastic change can produce a cutaneous horn? What is a special feature of their histology? Treatment? Actinic keratoses Parakeratosis Use imiquimod 16. Why do squamous cell carcinomas happen? How are SCCs different from actinic keratoses? What is keratoacanthoma? UV and immunosuppression from chemo or organ transplans Nuclear atypia at all levels of the epidermis Well differentiated SCC? Cup shaped tumor that usualy regresses spontaneously 17. What are the two patterns of basal cell carcinoma? What syndrome causes them? Multifocal growths (wide) Nodular lesion (deep) Both often show palisading on their periphery Gorlin syndrome/nevoid basal cell arcinoma syndrome i. Medulloblastomas/ovarian fibromas, odontogenic keratocysts, pits in the palms and soles, intracranial calcification, cleft lip and palate, abnormal vertebral segmentation, rib abnormalities 18. How do you distinguish fibrous histiocytomas from nodular melanomas? Fibrous hyistiocytomas dimple inward on lateral compression 19. What does dermatofibrosarcoma protuberans look like? What are its behavior and histology? Nodules on the trunk Locally aggressive, but rarely metastasizes Storiform: fibroblasts arranged radially 20. What is mycosis fungiodes d’emblée? 3 features of mycosis fungiodes/T cell lymphoma? Resembles _____ in early stages? What is it called when malignant T cells seed the blood? More aggressive nodular eruptive variant Plaques, patches, and nodules Psoriasis Sézary syndrome 21. What are the two histologic features of mycosis fungoides? Sézary-Lutzner cells Form clusters as Pautrier microabscesses; then they look cerebriform 22. What is urticaria pigmentosa? Localized mastocytosis that affects children 23. 2 signs of mastocytosis? What 3 things are seen in systemic disease? Darier sign (localized edema and wheal [redness]) when rubbed Dermatographism Foods, temp changes, alcohol, painkillers, rhinorrhea all cause pruritus and flushing bleeding bone pain from osteoblast/clast involvement 24. Enzyme deficiency linked to icthyosis? Steroid sulfatase 25. What causes urticaria? Usually IgE dependent reaction i. Opiates, antibiotics, curare, contrast media ii. Chemicals that mess with PGE2 iii. Hereditary angioneurotic edema (C1 deficiency) 26. What do poison ivy/oak cause? What does that mean? What helps to prevent contact dermatitis? Eczema Like urticaria, but edema goes beyond the superficial dermis and causes splaying of cells=> vesicles Chronic UV exposure helps kill Langerhans cells 27. What do you call an array of different lesions, like macules, papules, vesicles, bullae, and target lesions? What are 4 causes? Erythema multipforme 1) Infections of HSV, fungi, typhoid and leprosy 2) Sulfonamides, penicillin, bariturates, salicylates, hydantoins, and antimalarials 3) Malignancy 4) Collagen vascular diseases 28. What is extensive erythema multiforme? Stevens-Hohnson syndrome 29. Is pustular psoriasis dangerous? Either benign and localized or generalized and dangerous 30. What are 4 microscopic characteristics of psoriasis? Downward elongation of rete ridges Stratum granulosum is thinned or absent, overlying parakeratotic scale Auspitz sign caused by underlying blood vessels Spongiform pustules i. Monro microabscesses when within the stratum corneum 31. What is the Koebner phenomenon and in what diseases does it occur? Trauma=> lesions Psoriasis and lichen planus 32. What is Leiner disease? Seborrheic dermatitis in infants plus diarrhea and failure to thrive 33. What microbe can have a role in seborrheic dermatitis? How do we know sebum is involved? Malassezia furfur People with Parkinson disease often get it, levodopa decreases incidence 34. In what disease do Wickham striae occur? What bodies are seen in the dermis? White dot or lines overlying lichen planus Colloid/Civatte bodies, which are dead basal cells 35. Where is pemphigus foliaceus endemic? What is the most severe and common form of pemphigus? When is it a paraneoplastic lesion? Where does the blister form? Brazil (“fogo selvagem”), mildest form of pemphigus; scalp, face, chest, and back Pemphigus vulgaris 36. 37. 38. 39. 40. 41. 42. 43. 44. 45. Hodgkin lymphoma Suprabasally