Ethical Argument Paper
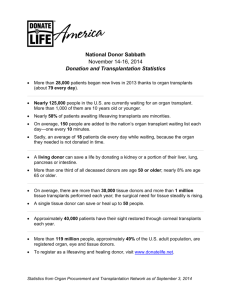
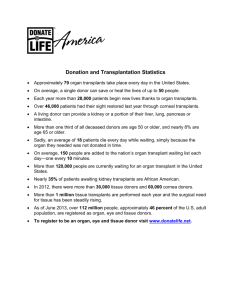
advertisement

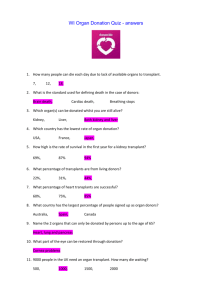
WHO SHOULD RECEIVE ORGAN TRANSPLANTS? Who Should Have Priority in Receiving an Organ Transplant? Kathleen Jones Virginia Commonwealth University Author Note This paper was prepared for Focused Inquiry 112 taught by Professor Nelson. 1 WHO SHOULD RECEIVE ORGAN TRANSPLANTS? 2 What’s the problem? In 2013, there were over 120,000 candidates waiting to receive donor organs. Only about 29,000 transplants were received from about 14,000 donors (“The Need Is Real: Data”, n.d.). That being said, it is obvious that there are not enough donors or organs to give every person who needs a transplantation surgery a compatible organ. With this shortage, who should have priority in receiving these donor organs? Who has the authority to decide which candidates have priority? What does it mean to be a candidate? For clarification, being a candidate means that you have a condition that qualifies you for transplant surgery. To be considered a candidate, most transplant surgeons recommend that you be under the age of 65, be generally healthy, lead a responsible lifestyle after the surgery, that at all other treatment options have been tried or ruled out and that death will be the result of not receiving the donor organ (“Who is a Candidate for Cardiac Transplantation?, n.d.). Who are the donors? Abouna (2003) stated that there are two main types of donors: living donors and cadavers. Living donors can donate a kidney, parts of the liver, lungs, pancreas, and intestines (“Organ and Tissue Donation From Living Donors”, n.d.). Cadavers, as long as they have been registered as donors, can donate just about any other organ in the body as long as the organs are recovered in time. WHO SHOULD RECEIVE ORGAN TRANSPLANTS? 3 Why shouldn’t everyone have an equal opportunity? You might have some preconceptions about organ transplants and think that the process should be completely fair and as indiscriminative as possible. Why should someone who has been on a waiting list for a donor organ be put on the back burner just so someone else can cut ahead? Think about the situation this way: Is it still fair if someone who smokes two packs of cigarettes a day was deemed more eligible for a lung transplant than someone who is otherwise healthy simply because of placing on a list? Would it be fair for an otherwise healthy man to have to risk shortening his life dramatically by waiting for a kidney transplant while an athlete with kidneys damaged from steroid use receives a transplant because he was first on the list? The answer is undeniably no. One of the guidelines for being a candidate for an organ transplant is that the patient has to be responsible after surgery. I do not believe that previous drug abusers can be trusted to be responsible enough after surgery to be deemed worthy of something as valuable as an organ donation. This being said, the ethical issue of organ donation lies in the question of how to prioritize the system of organ allocation. While I understand that prioritizing who receives organs can be seen as unfair, there are solutions that ultimately equalize the entire system. Solutions? I believe one solution is to give those who are registered as organ donors priority if they are ever in need of a donor organ. I think it is only fair that someone who is willing to save lives with their organs should be allowed to receive organs. Not only would this help prioritize organ allocation, but it would also help eliminate the extreme shortage of WHO SHOULD RECEIVE ORGAN TRANSPLANTS? 4 donors. Using organ donor status as a basis of prioritization also removes the question “Who has the authority to decide who receives organs?” from the equation because people are deciding for themselves by making the choice to be an organ donor. Some may argue that this solution is not fair because not everyone can be an organ donor due to diseases such as HIV and cancer. I do not believe it is fair that people who are undeserving are receiving such a valuable, life-saving gift, but I can understand that each situation is different. This leads me to my next solution: stem cells. In a 2012 article, Alois Gratwhol suggested that hematopoietic stem-cell transplantation could be the solution to organ trafficking, which is the sale of organs, and fraud on organ waiting lists (Gratwohl, "Organ Donation: Stricter management of organ transplants", 2012). Stem-cells are cells that can regenerate to create specialized cells and tissues. In this case, hematopoietic stem-cells are bloods cells that can be transplanted to repair bone marrow, but they can also be used to repair certain parts of damaged organs through their specialized regeneration. This encourages people in need of organs to turn to their own bodies for solutions first. I think this same idea could be used to prioritize donor lists. Using stem cells from the recipient’s own body would not only reduce the risk of organ rejection, but it would also increase the amount of organs available to other people in need. I believe that prioritizing organ allocation for transplants and my solutions are the ethical options based on the principle of beneficence. This means that these options are the wisest choices because they create the greatest amount of good for everyone involved. This principle is beneficial for the organ donors because it ensures that their organs are put WHO SHOULD RECEIVE ORGAN TRANSPLANTS? 5 to the best use by granting them to the most worthy candidates. It also benefits anyone who may need an organ transplant because there would be more organs available for allocation. People are also encouraged to register as organ donors so that they may receive priority in the event that they must have an organ transplant. Overall, the principle of beneficence proves the ethicality of this issue. Conclusion In conclusion, organ allocation should be prioritized to ensure that those who deserve the organs the most are the ones who get transplantation surgery. In order to prioritize the donor lists, those who are organ donors themselves should be the first to receive organs for transplant. This idea acts as almost a reward for being a donor while helping to fix the growing gap between the amount of donors and people who need organ transplantation surgery. Stem cells offer another solution to the ethical dilemma by giving patients a way to possibly help themselves by using their own blood before turning to one of many donor lists. Although some may argue that prioritizing the system for organ allocation isn’t fair, I do not think its fair for perfectly good organs to go to waste on an individual who is going to abuse to the opportunity by being irresponsible after the transplant just because they came first on a list. As a closing thought, everyone should consider becoming an organ donor, but not only for the personal benefit I previously discussed. When we die, our organs serve us no purpose, but for someone else, they could save a life. WHO SHOULD RECEIVE ORGAN TRANSPLANTS? 6 References Abouna G.M. (2003) . Ethical Issues in Organ Transplantation. Medical Principles and Practice, 12(1), 53-69. (DOI:10.1159/000068158) Gratwohl, A. (2012). Organ Donation: Stricter management of organ transplants. Nature, 488(7412), 1489-1492. Retrieved November 23, 2014, from doi:10.1038/488459b Organ and Tissue Donation from Living Donors. (n.d.). Retrieved November 24, 2014, from http://organdonor.gov/about/livedonation.html The Need Is Real: Data. (n.d.). Retrieved November 24, 2014, from http://www.organdonor.gov/about/data.html Who is a Candidate for Cardiac Transplantation? (n.d.). Retrieved November 24, 2014, from http://hearttransplant.com/candidate.html