Maple Syrup Diet - Jacqueline Farralls Portfolio
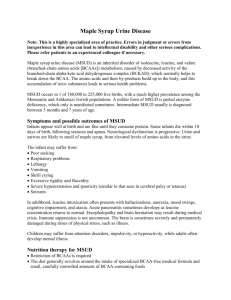
advertisement

MAPLE SYRUP URINE DISEASE (MSUD) Patient Description 27-year old female looking to get pregnant. MSUD runs in family and after genetic screening, finds she is a carrier as well. Her husband is also a carrier. She is consulting with medical professionals, including dietitian, doctor, and genetic counselor to identify risks, complications, and what to expect if she were to have a child with this genetic disease. I. Etiology a. MSUD is a genetic metabolism disorder passed down through families in which the body cannot break down certain parts of proteins. This disorder is caused by a gene defect in which the amino acids leucine, isoleucine, and valine cannot be broken down, resulting in a build up of chemicals within in the blood. MSUD is inherited in an autosomal recessive pattern. For a child to get the disease, he or she must inherit a defective copy of the gene from each parent. If both parents carry the MSUD gene, each of their children has a 25 percent chance of getting the disorder, and a 50 percent chance of being a carrier. b. In most populations, MSUD is an extremely rare disorder; only in 1 in 180,000 babies are born with it. II. Diagnostic Measures a. In some states, all babies are screened for MSUD within 24 hours after birth. A blood sample taken from the baby's heel is analyzed for high leucine levels. Normal leucine levels are less than 4 mg/dL (0.4 mg/ml). Even a slight elevation of plasma leucine in the normal newborn is unusual unless the baby is premature and/or receiving IV amino acid preparations. b. Diagnosis can usually be suspected from the characteristic burnt caramel smell of the urine and is confirmed by abnormal levels of amino acids and keto acids in the blood and urine. Other symptoms may include metabolic acidosis and depressed serum alanine levels. The enzyme defect may also be detected in leukocytes and/or fibroblasts. c. The method screening for birth is for deficiency of branched-chain alpha-ketoacid dehydrogenase activity in cultured chorionic villi. d. Symptoms begin as soon as an infant is fed protein, usually shortly after birth. Some of the first symptoms include: poor appetite, weak suck, weight loss, high pitched cry, urine that smells that like maple syrup or burnt sugar. Babies with MSUD will also have episodes of illness called metabolic crisis, symptoms of which are: extreme sleepiness, sluggishness, irritable mood, and vomiting. III. Treatment a. Medical surgical, psychological i. Prompt treatment is needed to prevent mental retardation and serious medical problems. Children are given a special medical formula as a substitute for milk. This formula gives them the nutrients and protein they need while helping keep their BCAA (branch chain amino acid) levels in a safe range. ii. Regular blood tests to measure amino acid levels are necessary iii. Liver transplantation – the first liver transplantation done in 1997 on an infant with acute liver failure due to a cause outside of MSUD, the infant’s MSUD was metabolically corrected and cured. Infants undergoing liver transplants are able to resume normal liver function and follow an unrestricted diet. iv. Genetic counseling and genetic counselors who have special training in inherited disorders are available to families who have children with MSUD and can answer questions about how the condition is inherited, choices during future pregnancies, and how to test other family members. b. Medical Nutrition Therapy i. Diet is absolutely crucial to healthy development and prevention of further complications in children with MSUD. ii. The primary goal is to maintain BCAA’s, particularly leucine, within normal limits; studies have shown a correlation between cognitive decline and elevated blood leucine levels. Protein from food is digested and broken down into these amino acid components and are necessary for making tissues for the body. BCAA’s are essential and must be consumed from food. Normally, if more protein is eaten than is needed, it will be broken down to make energy. However, in MSUD the enzyme required is either present in inadequate amounts or is not functioning properly. This causes toxic levels of leucine and its ketoacid to accumulate. iii. Maintaining blood BCAA levels within recommended limits while ensuring adequate calories and protein and avoiding nutritional deficiencies is the primary goal of MNT for MSUD patients. To do so, the diet must strictly restrict BCAA. 1. The best way to ensure adequate protein intake is by consuming a metabolic formula with all of the essential amino acids needed by the body without the BCAA. These will provide up to 90 percent of the patient’s protein intake. Formulas include: Analog (infant), Ketonex1 (infant), BCAD1 (infant), Acerflex(teen/adult), Maxamaid MSUD (teen/adult), and BCAD2 (teen/adult). This protein is best used by the body when taken multiple times a day. iv. It is important to keep track of the exact amount of protein and specifically, leucine, content in foods by using a food list. Use one food list consistently. Leucine should be added to the diet in the form of regular formula or table foods when leucine levels are normalized (primarily in infants). Other amino acids (isoleucine, valine) should be supplemented; tyrosine also helps decrease leucine brain levels. v. Despite dietary compliance, illness can cause elevated levels of BCAA. Pushing fluids and calories during this time helps flush out toxins; parents are also asked to monitor metabolic control by checking the urine for ketones. vi. Because of the restrictive nature of this diet, nutritional deficiency is a possibility. Deficiencies in trace minerals, like sodium, have been reported; marginal calcium intake along with chronic acidosis related to elevated branch chain ketone levels can lead to decreased bone mineralization (increasing risk for osteoporosis); deficient levels of essential fatty acids, found primarily in the restricted protein sources, can occur. vii. Over-restriction of protein can develop, causing poor growth, fat deposits in the muscle, decreased REE, skin rashes, decreased immunity and appetite, and decreased hair loss. Valine deficiency can lead to poor growth, irritability, drowsiness, and decreased blood protein levels. Therefore it is essential that MSUD patients are receiving sufficient amounts of all EFAs. viii. Diet also depends on the type of MSUD. With classic MSUD, there is less than 2 percent of normal activity of the enzyme branched-chain a-Keto acid Dehydrogenase (BCKD) and is the most severe and most common; leucine is more elevated than other BCAA’s. Intermediate MSUD is less severe and less common than classic and has about 3 to 30 percent of normal BCKD activity. All BCAA levels are elevated, but leucine is less. Intermittent MSUD has about 5 to 20 percent of normal enzyme activity and is also less common. 1. Thiamine-responsive MSUD responds to thiamine in daily doses of 100 to 150 grams and abnormal BCAA’s are only present with metabolic episodes. Thirty to 40 percent of enzyme activity is present. ix. Long term treatment requires the use of special medical food to provide protein intake of 2 to 2.5 grams/kg daily. A diet low in leucine, 300 to 600 mg established by age 2 to 3 is maintained daily for the rest of the individuals life. x. Dietary treatment changes with age. It is important to have regular follow up meetings to make sure that treatment is adjusted appropriately to account for growth and metabolic stability. 1. Around 6 months, babies need to eat mainly fruits and vegetables and certain baby foods. Later on, they can eat a wider range of low protein foods, including special bread and pasta. xi. Physical activity is important; with more muscle, a better tolerance of leucine in the diet is created. xii. The effectiveness of treatment is monitored by nutritional status, metabolic control and compliance. Strict dietary control is needed for life. c. Prognosis i. If untreated, MSUD is life threatening. ii. With prompt and lifelong treatment, children with MSUD often have healthy lives with typical growth and development. However, even with treatment, some may still develop swelling of the brain and have episodes of metabolic crisis that may develop permanent brain damage. This can cause lifelong learning problems, mental retardation or spasticity. iii. Even with dietary treatment, stressful situations and illness can still cause high levels of certain amino acids. References “Amino Acid Disorders.” (2010). STAR-G: Screening, Technology, and Research in Genetics. Retrieved from http://www.newbornscreening.info/Parents/aminoaciddisorders/MSUD.html. Online. Internet. Jan. 24, 2013. Australasian Society for Inborn Errors of Metabolism (2005). The ASIEM low protein handbook for MSUD. Nutriticia. Retrieved from http://www.hgsa.org.au/website/wp-content/uploads/2010/02/MSUD2.pdf. Online. Internet. Jan. 23, 2013. “Diagnostics for MSUD.” (n.d.) Clinical Cases in Biochemistry. Retrieved from http://www.uic.edu/classes/phar/phar332/Clinical_Cases/aa%20metab%20cases/MSUD/ Diagnostics_of_MSUD.html. Online. Internet. Jan. 26, 2013. Genetic Science Learning Center (2012). Maple syrup urine disease (MSUD). Learn Genetics. Retrieved from http://learn.genetics.utah.edu/content/disorders/whataregd/msud/. Online. Internet. Jan. 25, 2013. Jurecki, Elaina (2009). Nutritional management of MSUD. MSUD Family Support Group. Retrieved from http://www.msudsupport.org/index.php?option=com_content&view=article&id=352%3Anutritionalmanagement-of-msud&Itemid=120. Online. Internet. Jan. 24, 2013. Nelms, Sucher, Lacey, & Roth. (2011). Nutrition therapy and pathophysiology. Belmont, CA: Madsworth, Cengage Learning. “Maple Syrup Urine Disease.” (2012). National Institutes of Health: Office of Rare Diseases Research. Retrieved from http://rarediseases.info.nih.gov/GARD/Condition/3228/QnA/25358/Maple_syrup_urine_ disease.aspx. Online. Internet. Jan. 23, 2013. “Maple Syrup Urine Disease: MSUD.” (2011). PubMed Health. Retrieved from http://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0001411/. Online. Internet. Jan. 23, 2013. Mazariegos, George (2013). Maple syrup urine disease. Children’s Hospital of Pittsburgh. Retrieved from http://www.chp.edu/CHP/maple+syrup+urine+disease+liver. Online. Internet. Jan. 26, 2013. Wappner, Rebecca (2001). Description and treatment of maple syrup urine disease. MSUD Family Support Group. Retrieved from http://www.msud support.org/index.php?option=com_content&view=article&id=219%3Adescription-atreatment-of-maple-syrup-urine-disease&Itemid=120. Online. Internet. Jan. 23, 2013.