Policy No: ANES 3.0 - Tulane University Department of Anesthesiology
advertisement

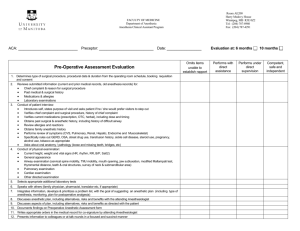
TULANE UNIVERSITY HOSPITAL & CLINIC Policies & Procedures Manual Policy No: ANES 3.0 Page: 1 of 11 Effective Date: February 13, 2006 Supersedes Policy: Policy Origin Date: Last Reviewed: September 1, 2014 Last Revised: September 1, 2014 Dated: November 1993 July 27, 2001/May 17, 2005 Originating Dept./Committee: Anesthesiology April 29, 2003 TITLE: Preanesthesia Assessment PURPOSE: A preanesthesia assessment is performed for each patient before anesthesia induction. POLICY: Prior to anesthesia, the anesthesiologist and the attending surgeon determine if the patient is an appropriate candidate. PROCEDURE: 1. The determination is on the medical and physical history, the pre anesthetic assessment, laboratory, and diagnostic 2. 3. 4. 5. 6. data. The patient and family are apprised of the risks/benefits of anesthesia and the administration of blood and blood products. The responsible anesthesiologist verifies that the above has been properly performed and documented in the patient’s record and reviewed by all anesthesia personnel involved in the case. Preanesthesia patient assessment is performed before the operative procedure by a member of the anesthesia team (CRNA or anesthesia resident and staff anesthesiologist). The plan for anesthesia is discussed with the patient. The patient is reevaluated on the day of the procedure by the anesthesiologist. Consents are obtained. The purpose of the preoperative visit is not only to gather important information and obtain informed consent, it also helps establish a healthy doctor-patient-family relationship where the anesthesiologist, resident or CRNA answers all important questions, allowing the patients and family to know what to expect. The Anesthesiology Department follows Tulane University Medical Center Medical Staff By- Laws, Rules and Regulations Policy and Procedure 11.1-2 “Requirements Prior to Induction of Anesthesia and Operation”, and the “Basic Standards for Pre anesthesia Care” (approved by House of Delegates on October 14, 1987), as follows: In addition, consent is obtained by patient/guardian for anesthesia-refer to ANES 2.0. The standards apply to all patients who receive anesthesia or monitored anesthesia care. Under unusual circumstances, e.g. extreme emergencies, these standards may be modified. When this is the case, the circumstances shall be documented in the patient’s record. The development of an appropriate plan of anesthesia care is based upon: TULANE UNIVERSITY HOSPITAL & CLINIC Policies & Procedures Manual Policy No: ANES 3.0 Page: 2 of 11 Effective Date: February 13, 2006 Supersedes Policy: Policy Origin Date: Last Reviewed: September 1, 2014 Last Revised: September 1, 2014 Dated: November 1993 July 27, 2001/May 17, 2005 Originating Dept./Committee: Anesthesiology April 29, 2003 a. Reviewing the medical record. b. Interviewing and examining the patient to: c. Discuss the medical history, previous anesthetic experiences and drug therapy. d. Assess those aspects of the physical condition that might affect decisions regarding preoperative risk and management. e. Obtaining and/or reviewing tests and consultations necessary to the conduct of anesthesia. f. Determining the appropriate prescription of preoperative medications as necessary to the conduct of anesthesia. g. The responsible anesthesiologist shall verify that the above has been properly performed and documented in the patient’s record. h. The preoperative evaluation is written and documented in the patient’s chart describing medical history, post anesthetic history, the physical examination, drug and alcohol history, allergies, laboratory results, ASA classification and the recommendations of any consultations. 11.1 SURGICAL SERVICES 11.1-1 TIME OF ADMISSION Except in cases of emergency, same day or one-day surgery patients are given a specific time to come prepared for their scheduled surgery. 11.1-2 REQUIREMENTS PRIOR TO INDUCTION OF ANESTHESIA & OPERATION A. Pre-Operative Evaluation and Documentation: 1. Histories and physical examinations shall be completed in accordance with the general regulations set forth in these Rules and Regulations. 2. Prior to all operations, the operating physician or his house officer shall note in the patient’s record the preoperative diagnosis and his reason and plan for the procedure to be performed. The anesthesiologist must document in the record a pre-anesthesia evaluation of the patient including pertinent information relative to the choice of anesthesia and the procedure anticipated, pertinent previous drug history, other pertinent anesthetic experiences, and any potential anesthetic problems. Except in cases of emergency, this evaluation should be recorded prior to the patient’s transfer to the operating area and before preoperative medication has been administered. Immediately prior to induction, the patient is reassessed by the anesthesiologist and documented on the anesthesia record. 3. Except in cases of emergency so documented in writing by the operating surgeon, pre-operative diagnostic and laboratory value must be ordered and performed prior to any surgical procedure that is to be done under general, regional, or monitored anesthesia care provided by an anesthesiologist or his/her designee. TULANE UNIVERSITY HOSPITAL & CLINIC Policies & Procedures Manual Policy No: ANES 3.0 Page: 3 of 11 Effective Date: February 13, 2006 Supersedes Policy: Policy Origin Date: Last Reviewed: September 1, 2014 Last Revised: September 1, 2014 Dated: November 1993 July 27, 2001/May 17, 2005 Originating Dept./Committee: Anesthesiology April 29, 2003 4. Patient’s history/physical or proposed surgical procedure may modify pre-operative laboratory requirements. 5. Prior diagnostic test results, which meet the medical records format, will be accepted. a. Chest X-Ray: A chest X-Ray showing normal results that was performed within one year of surgery can be used if there has been no intervening clinical event. b. ECG: An ECG showing normal results that was performed within six months of surgery can be used if there has been no intervening clinical event. c. Blood Tests: Tests performed within six weeks of surgery that show normal results can be used if there has been no intervening clinical event. B. Consent: Surgical procedures may be performed only upon written informed consent as provided in Section Eight of these Rules and Regulations. Written, signed, informed surgical consent shall be obtained prior to administration of pre-medication for the operative procedure except in those situations wherein the patient’s life is in jeopardy and suitable signatures cannot be obtained due to the condition of the patient. Patient is reassessed prior to induction and clearly documented in the record. C. Identification: Prior to the induction of anesthesia, the individual responsible for administering anesthesia shall verify the patient’s identity. D. Surgical Procedure: The Operating Surgeon, his designee and/or Nursing shall verify the site and side of the body to be operated upon and ascertain that the information required under paragraphs A and B of this Section 10.1-2 is in the patient’s record. If the required information is not in the record, the procedure shall be canceled or postponed, unless the operating practitioner states in writing that such a delay would constitute a hazard to the patient. 11.1-3 QUALIFIED ASSISTANT In any surgical procedure with unusual hazard to life, there must be a qualified assistant scrubbed and present throughout the operation. TULANE UNIVERSITY HOSPITAL & CLINIC Policies & Procedures Manual Policy No: ANES 3.0 Page: 4 of 11 Effective Date: February 13, 2006 Supersedes Policy: Policy Origin Date: Last Reviewed: September 1, 2014 Last Revised: September 1, 2014 Dated: November 1993 July 27, 2001/May 17, 2005 Originating Dept./Committee: Anesthesiology April 29, 2003 11.1-4 TRANSPORT OF PATIENTS Patients are transported to the surgical suite by litter with safety straps or side rails in place. Moving of patients within the surgical suite and in the recovery room is under supervision of the operating room supervisor. 11.1-5 ATTIRE All personnel entering the operating room are to be dressed in the proper scrub suits, caps, masks and boots. If operating room attire is worn outside the operating suite, it must be covered with a laboratory coat or other appropriate apparel and must be changed prior to the next case. 11.1-6 TRAFFIC PATTERNS Operating room traffic patterns must be strictly observed. Personnel not working in the operating suite are to refrain from entering the area. The operating room supervisor is to report all violations to the Chief of Staff and the Operating Room Committee. 11.1-7 UNUSUAL EVENT REPORTING Any unusual or unexpected incidents that occur during an operative procedure should be reported to the Perioperative Clinical Manager. This includes, without limitation, any serious break of sterile technique occurring during a procedure, equipment breakdown or failure during a procedure, instruments or material lost during an operative procedure, and like incidents including any with respect to the procedure itself. 11.1-8 TISSUE All tissue removed at the operation, with the exceptions mentioned in Section 6.4-2, shall normally be sent to the Hospital’s pathologist who shall make such examination as he may consider necessary to arrive at a tissue diagnosis. His authenticated report shall be made a part of the patient’s medical record. TULANE UNIVERSITY HOSPITAL & CLINIC Policies & Procedures Manual Policy No: ANES 3.0 Page: 5 of 11 Effective Date: February 13, 2006 Supersedes Policy: Policy Origin Date: Last Reviewed: September 1, 2014 Last Revised: September 1, 2014 Dated: November 1993 July 27, 2001/May 17, 2005 Originating Dept./Committee: Anesthesiology April 29, 2003 Table 1. Summary of Pharmacologic Recommendations to Reduce the Risk of Pulmonary Aspiration Medication Type and Common Examples Recommendation Gastrointestinal stimulants No routine use metoclopramide Gastricacid secretion blockers No routine use cimetidine famotidine ranitidine omeprazole lansoprazole Antacids No routine use sodium citrate sodium bicarbonate magnesium trisilicate Antiemetics No routine use droperidol ondansetron Anticholintergics No use atropine scopolamine glycopyrrolate Combinations of the medications above No routine use TULANE UNIVERSITY HOSPITAL & CLINIC Policies & Procedures Manual Policy No: ANES 3.0 Page: 6 of 11 Effective Date: February 13, 2006 Supersedes Policy: Policy Origin Date: Last Reviewed: September 1, 2014 Last Revised: September 1, 2014 Dated: November 1993 July 27, 2001/May 17, 2005 Originating Dept./Committee: Anesthesiology April 29, 2003 GUIDELINES FOR PATIENT CARE IN ANESTHESIOLOGY (Approved by House of Delegates on October 3, 1967 and last amended on October 23, 1996) I. Definition of Anesthesiology: Anesthesiology is a discipline within the practice of medicine specializing in: A. The medical management of patients who are rendered unconscious and/or insensible to pain and B. C. D. E. F. emotional stress during surgical, obstetrical and certain other medical procedures (involves preoperative, intraoperative and postoperative evaluation and treatment of these patients); The protection of life functions and vital organs (e.g., brain, heart, lungs, kidneys, liver) under the stress of anesthetic, surgical and other medical procedures; The management of problems in pain relief; The management of cardiopulmonary resuscitation; The management of problems in pulmonary care; The management of critically ill patients in special care units. II. Anesthesiologist's Responsibilities: Anesthesiologists are physicians who, after college, have graduated from an accredited medical school and have successfully completed an approved residency in anesthesiology, and, in addition, may have had additional training in critical care medicine and pain management. Anesthesiologists' responsibilities to patients should include: A. B. C. D. Preanesthetic evaluation and treatment; Medical management of patients and their anesthetic procedures; Postanesthetic evaluation and treatment; On-site medical direction of any nonphysician who assists in the technical aspects of anesthesia care to the patient. TULANE UNIVERSITY HOSPITAL & CLINIC Policies & Procedures Manual Policy No: ANES 3.0 Page: 7 of 11 Effective Date: February 13, 2006 Supersedes Policy: Policy Origin Date: Last Reviewed: September 1, 2014 Last Revised: September 1, 2014 Dated: November 1993 July 27, 2001/May 17, 2005 Originating Dept./Committee: Anesthesiology April 29, 2003 III. Guidelines for Anesthesia Care: A. The same quality of anesthetic care should be available for all patients: 1. 24 hours a day, seven days a week; 2. Emergency as well as elective patients; 3. Obstetrical, medical and surgical patients. B. Preanesthetic evaluation and preparation means that an anesthesiologist: 1. Reviews the chart. 2. Interviews the patient to discuss medical history, including anesthetic experiences and drug therapy. 3. Perform any examinations that would provide information that might assist in decisions regarding risk and management. 4. Orders necessary tests and medications essential to the conduct of anesthesia. 5. Obtains consultations as necessary. 6. Records impressions on the patient's chart. C. Perianesthetic care means: 1. Re-evaluation of patient immediately prior to induction. 2. Preparation and check of equipment, drugs, fluids and gas supplies. 3. Appropriate monitoring of the patient. 4. Selection and administration of anesthetic agents to render the patient insensible to pain during the procedure. 5. Support of life functions under the stress of anesthetic, surgical and obstetrical manipulation. TULANE UNIVERSITY HOSPITAL & CLINIC Policies & Procedures Manual Policy No: ANES 3.0 Page: 8 of 11 Effective Date: February 13, 2006 Supersedes Policy: Policy Origin Date: Last Reviewed: September 1, 2014 Last Revised: September 1, 2014 Dated: November 1993 July 27, 2001/May 17, 2005 Originating Dept./Committee: Anesthesiology April 29, 2003 6. Recording the events of the procedure. D. Postanesthetic care means: 1. A member of the anesthesia care team remains with the patient as long as necessary. 2. Availability of adequate nursing personnel and equipment necessary for safe postanesthetic care. 3. Informing personnel caring for patients in the immediate post-anesthetic period of any specific problems presented by each patient establishing baseline physiologic status, and ensuring the patient’s stability before relinquishing the care of the patient to the post-anesthesia care giver. 4. Assurance that the patient is discharged in accordance with policies established by the Department of Anesthesiology. 5. The period of post-anesthetic surveillance is determined by the status of the patient and the judgment of the anesthesiologist. The anesthesia provider must remain in the facility at all times until the patient is discharged. IV. Additional Areas of Expertise: A. B. C. D. E. V. Resuscitation procedures. Pulmonary care. Critical (intensive) care. Diagnosis and management of pain. Trauma and emergency care. Quality Assurance: The anesthesiologist should participate in a planned program for evaluation of quality and appropriateness of patient care and resolving identified problems. TULANE UNIVERSITY HOSPITAL & CLINIC Policies & Procedures Manual Policy No: ANES 3.0 Page: 10 of 11 Effective Date: February 13, 2006 Supersedes Policy: Policy Origin Date: Last Reviewed: November 19, 2010 Last Revised: November 19, 2010 Dated: November 1993 July 27, 2001/May 17, 2005 Originating Dept./Committee: Anesthesiology April 29, 2003