ROTATION SPECIFIC OBJECTIVES
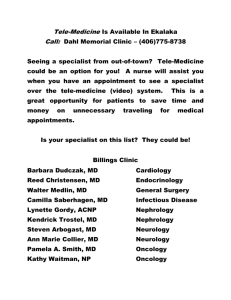
advertisement

DEPARTMENT OF PSYCHIATRY Learning Objectives PGY1 Psychiatry Residents Clinical Rotations & Electives July 2012 – June 2013 POSTGRADUATE EDUCATION DEPARTMENT OF PSYCHIATRY UNIVERSITY OF TORONTO Overview of Psychiatry Residency Training Welcome to psychiatry residency training! This booklet outlines the training objectives for your PGY-1 rotations. The Royal College of Physicians and Surgeons of Canada mandate the training that you must receive in order to be recognized as a specialist in psychiatry in Canada. These objectives are framed in terms of the CanMEDS Roles for physicians: medical expert communicator collaborator scholar health advocate manager professional CanMEDS Roles developed out of a project of the Royal College of Physicians and Surgeons of Canada in 1996 to provide an educational framework for physician competencies. It was subsequently revised in 2005. The CanMEDS roles were created by physicians in response to challenges in contemporary health care and were based on evidence and oriented to societal needs. Further information about CanMEDS Roles is located at the end of this document. What is the Purpose of the PGY1 Year? The PGY1 year of training is designed to consolidate your knowledge, skills and attitudes as a physician prior to embarking on specialty training in psychiatry. The medical knowledge, skills and attitudes you develop during your PGY1 year will inform your ability to provide excellent care to your psychiatric patients. It will also provide the medical foundation that you require in order to successfully complete your mandatory training in geriatric psychiatry, consultation-liaison psychiatry and shared care. Which Rotations Do I Complete in the PGY1 Year? PGY1 Psychiatry residents will complete rotations in: Internal Medicine Family Medicine OR Pediatrics Emergency Medicine Behavioural Neurology Neurology Neuroradiology Palliative Care Psychiatry Psych ER C/L Psych Addictions 2 months 1 month 1 month 1 month 1 month 1 week intensive 1 month 3 months 1 Elective 1 mo & Selective 1 mo 2 months (Elective & Selective months to be determined in discussion with Dr. Abbey. These months should be tailored in order to meet your individual learning needs and career goals. CSS residents must do two months of research with their supervisor other residents tailor their elective experience based on their personal learning needs) How do I organize my elective and selective? You will meet in the summer or early fall with the PGY1 Coordinator, Dr. Susan Abbey, who will help you to sort out opportunities that will meet your individual learning needs. How much time can I spend doing research? Research can be the focus of up to 2 months of training. You will need to complete an application form to spend your time doing research. The form is available on the Department web site and also from Dr. Abbey. PGY1s in the Clinician Scientist Stream are expected to spend two months of elective time doing research with their supervisor. Why Are There Objectives for Training? We have provided you with objectives that will help you to direct your learning and to make choices amongst the many educational opportunities that will be available to you. Please review the rotation specific objectives at the start of each rotation in order to orient you to the goals of training for that rotation. At the end of each rotation, your supervisor(s) will complete an ITER (In-Training Evaluation Report) that evaluates your performance on the rotation and that is based on these objectives. Who Can I Get Help From In Sorting This All Out? Dr. Mark Fefergrad, Director of Post-graduate Education for the Department of Psychiatry will meet with you during the course of the year to ensure that your educational needs are being met. He is very helpful and approachable and you should feel free to contact him if you need anything before your scheduled meeting. Dr. Susan Abbey, PGY-1 Coordinator for the Department of Psychiatry, will meet with you during the summer or early fall to help you sort out electives and to assist you in tailoring your training experiences to your individual needs. She will be happy to organize additional support or mentorship if that would be helpful to you. PGY1 Coordinators at each of the base hospitals are available to help you with site based issues. They are another important source of mentorship and support. 2 The PGY1 Coordinators at the base hospital are as follows: Mt. Sinai Dr. Ellen Margolese - EMargolese@mtsinai.on.ca St. Michael’s Dr. Mark Halman - Halmanm@smh.ca Sunnybrook Dr. Justin Weissglas – justin.weissglas@sunnybrook.ca UHN Dr. Susan Abbey - susan.abbey@uhn.ca Questions If you have any comments or questions about these training objectives, please contact the PGY-1 coordinator, Dr. Susan Abbey at susan.abbey@uhn.on.ca or 416-340-4447. What if My Attending Physician/Supervisor has a Question? If your attending physician/supervisor has any questions about these training objectives, please give them Dr. Abbey’s contact information (susan.abbey@uhn.on.ca or 416-3404447) or send her an email with their contact information and she will follow up with them. 3 CORE MEDICAL ROTATIONS 4 GENERAL INTERNAL MEDICINE Rotation offered at: MSH, SHSC, SMH, UHN Description: General internal medicine is a two-month core rotation for all PGY1 residents in psychiatry that occurs on clinical teaching units (CTUs). PGY1s are assigned to their base hospital whenever possible. The general internal medicine team provides care for patients with a wide spectrum of medical conditions. Each team consists of one senior resident (PGY2-3), two junior residents (PGY1-2), and a maximum of four clinical clerks under the supervision of an attending physician. The general internal medicine rotation provides an opportunity for the PGY1 psychiatry resident to develop knowledge and skills in the assessment and management of patients with a variety of medical illnesses. PGY1s will receive their general internal medicine training through care of inpatients on the clinical teaching units, consultation to the emergency room and through participation in educational opportunities including morning report, noon hour lecture series and medical grand rounds. Rotation Specific Objectives: Medical Expert Develop an approach to the diagnosis and management of a wide variety of clinical problems including patients presenting with the following clinical problems: o Cardiovascular – heart failure, coronary artery disease, atrial fibrillation, hypertensive emergencies, syncope, shock, valvular heart disease o Respiratory – obstructive airway disease, pleural effusion, thromboembolic disease, malignant disease, lower respiratory tract infections, interstitial lung disease o Gastrointestinal – GI bleeding, peptic ulcer disease, acute and chronic liver diseases and their complications, diarrhoea, pancreatitis, undifferentiated abdominal pain o Infectious – fever of unknown origin, complications of HIV infection, appropriate use of antibiotics, acute infectious illness (meningitis, encephalitis, pneumonia, endocarditis, gastroenteritis, sepsis, septic arthritis, cellulitus, pyelonephritis) o Endocrinologic – diabetes and its complications, adrenal disorders, thyroid disorders, complications of steroid use, calcium disorders, osteoporosis o General – weight loss, overdose, drug reactions, fatigue o Ethics – end of life care, informed consent, capacity assessment o Geriatric – frequent falls, incontinence, polypharmacy, failure to cope, the “social admission” 5 Develop technical skills related to in-patient care in general internal medicine including arterial puncture for blood analysis, nasogastric tube insertion, insertion of peripheral venous lines Communicator Obtain a history from patients and family members Effectively convey a management plan to patients and family members Communicate effectively with members of the multidisciplinary team in the general internal medicine setting and to liaise effectively with community practitioners and agencies involved with general internal medicine patients and their families Communicate effectively and efficiently with consulting services Scholar Access relevant literature and other resources to guide assessment and management of general internal medicine patients Develop skills in the critical appraisal of literature regarding the diagnosis and treatment of issues in general internal medicine Manager Efficiently assess patients and initiate and tailor management plans for patients in the emergency room or inpatient medical ward setting Develop time management skills to reflect and balance priorities for patient care, sustainable practice, and personal life Collaborator Describe and understand the role of the physician in the general internal medicine setting Describe and understand the roles of allied healthcare professionals, both within the hospital setting and in the community, with respect to the assessment and management of general internal medicine patients and their family and friends Health Advocate Advocate effectively on behalf of general internal medicine patients for the services that they require Identify opportunities for patient counseling and education regarding their medical conditions Educate patients regarding lifestyle modifications that may prevent disease including modification of cardiovascular risk factors Professional Demonstrate professional attitudes in interactions with patients, families and other healthcare professionals Recognize and appropriately respond to ethical challenges in the general internal medicine setting 6 FAMILY MEDICINE OR PEDIATRICS Rotation offered at: Multiple Sites Description: The Royal College mandates that PGY1s in psychiatry spend a month in either family medicine or pediatrics. The U of T offers many different options to fulfill this requirement so that you can tailor your learning environment to your learning preferences and career needs. General objectives for both rotations are show in the pages that follow. 7 FAMILY MEDICINE Rotation offered at: Academic health science centre family medicine units Community family medicine sites including family health teams, community health centres and family health care providers offices. CAMH Family Health Team Rural Ontario Medical Program (ROMP) sites Description: The Royal College mandates that PGY1s in psychiatry spend a month in either family medicine or pediatrics. The U of T offers many different options to fulfill this requirement so that you can tailor your learning environment to your learning preferences and career needs. You have the opportunity to undertake family medicine training in the type of family medicine environment that is most helpful for your leaning needs. All of the family medicine sites provide primary care for patients with a wide spectrum of medical conditions. The composition of the teams varies by site. The family medicine rotation provides an opportunity for the PGY1 psychiatry resident to develop knowledge and skills in the assessment and management of patients in the primary care setting presenting with a variety of medical and psychiatric illnesses and psychosocial dysfunction and distress. Rotation Specific Objectives: Medical Expert Demonstrate a broad, relevant, up-to-date knowledge base in conditions relevant to primary care Demonstrate ability to conduct a focused, accurate and complete history and physical exam Develop an approach to the diagnosis and management to common symptoms in primary care: o Headache o Fatigue o Abdominal pain o Dizziness o Back Pain o Chest Pain Develop an approach to the management of common clinical problems including: 8 o o o o o o o o o Infections Hypertension Diabetes GERD Fatigue Abdominal pain Dizziness Back Pain Chest Pain Demonstrate counseling and psychotherapy skills related to lifestyle issues and psychosocial problems Communicator Obtain a focused history from patients +/or family members Uses a patient centred approach and demonstrating understanding of the patient agenda and illness experience Effectively convey a management plan to patients and family members Effectively communicates and collaborates with the multidisciplinary team in the family medicine setting Effectively communicates and collaborates with community health care providers. Scholar Access relevant literature and other resources to guide assessment and management of primary care patients Develop skills in the critical appraisal of literature regarding the diagnosis and treatment of issues in primary care Manager Develop time management skills related to handling multiple clinical demands and responsibilities Collaborator Describe and understand the role of the physician in the primary care setting Describe and understand the roles of allied healthcare professionals, both within the primary care setting and in the community, with respect to the assessment and management of primary care patients and their family and friends Health Advocate Advocate effectively on behalf of primary care patients for the services that they require Identify opportunities for patient counseling and education regarding their medical conditions Educate patients regarding lifestyle modifications that may prevent disease including modification of cardiovascular risk factors 9 Professional Demonstrate professional attitudes in interactions with patients, families and other healthcare professionals Recognize and appropriately respond to ethical challenges in the primary care setting 10 PEDIATRICS Rotation offered at: Hospital for Sick Children – Emergency room or inpatient ward Community hospitals including North York General Hospital and Toronto East General Hospital Community pediatricians Pediatric programs with a specific focus – e.g. developmental pediatrics, adolescent medicine, Rural Ontario Medical Program (ROMP) sites Description: The Royal College mandates that PGY1s in psychiatry spend a month in either family medicine or pediatrics. The U of T offers many different options to fulfill this requirement so that you can tailor your learning environment to your learning preferences and career needs. You have the opportunity to undertake pediatric training in the type of environment that is most helpful for your leaning needs. All of the pediatric sites provide pediatric care with a wide spectrum of medical conditions. The composition of the teams varies by site. The pediatric rotation provides an opportunity for the PGY1 psychiatry resident to develop knowledge and skills in the assessment and management of pediatric patients in the primary care setting presenting with a variety of medical and psychiatric illnesses and psychosocial dysfunction and distress. Rotation Specific Objectives: Medical Expert To assess pediatric patients and recognize both common illnesses that can be managed at home and those with critical illnesses that require in-patient care Demonstrate ability to conduct a focused, accurate and complete history and physical exam Develop an approach to the pediatric patient with multiple disabilities or multisystem problems Demonstrate counseling and psychotherapy skills related to lifestyle issues and psychosocial problems Communicator Obtain a focused history from patients +/or family members 11 Communicate effectively and empathetically with parents and children and involve families in decision-making Effectively communicate with other physicians as well as members of the multidisciplinary team in the pediatric setting Effectively communicates and collaborates with community health care providers. Scholar Access relevant literature and other resources to guide assessment and management of pediatric patients Develop skills in the critical appraisal of literature regarding the diagnosis and treatment of issues in pediatrics Manager Develop appropriate and cost-effective use of diagnostic and consulting services Develop an understanding of the principles of quality improvement by attending morbidity and mortality rounds Collaborator Develop the attitude of cooperative and collaborative team work and the ability to work with and share responsibilities with other medical and health care professionals including nurses, social workers, dieticians, physiotherapists and occupational therapists, and respiratory therapists. Health Advocate Demonstrates and promotes active involvement of the family in medical decision making and comprehensive care of the child. Identifies the psychosocial, economic and societal factors that may affect a child’s health and ability to receive care Recognizes and responds appropriately to advocacy situations. Professional Demonstrate professional attitudes in interactions with patients, families and other healthcare professionals Recognize and appropriately respond to ethical challenges in the pediatric setting 12 EMERGENCY MEDICINE Rotation offered at: MSH, SHSC, SMH, UHN Description: Emergency medicine is a one-month core rotation for all PGY1 residents in psychiatry that occurs in the emergency departments of their base hospitals whenever possible. This is a busy rotation during which residents participate in all aspects of patient care in the emergency department including initial stabilization, decision making regarding investigations, treatment and admission/discharge disposition. Rotation Specific Objectives: Medical Expert Perform an accurate and concise history and physical examination in the undifferentiated patient presenting to the emergency department Demonstrate the ability to formulate an appropriate plan for the investigation, treatment, and disposition of the undifferentiated patient presenting to the emergency department Utilize a systematic approach to issues of resuscitation in the patient: o with a compromised airway including indications for intubation of a patient and an understanding of the possible complications of this procedure, understand the various airway adjuncts, ventilation devices and oxygen administration devices o with common cardiac dysrhythmias including ventricular fibrillation, ventricular tachycardia, asystole, bradycardia, supraventricular tachycardias, o in shock including classification of the causes of shock Demonstrate an approach to the emergency diagnosis and management of: o substance abuse and toxic exposures – the poisoned patient including recognition of toxidrome decontamination procedures, laboratory investigations, use of antidotes, utilization of the Regional Poison-Control Centre as a resource; recognition and management of alcohol-related disease including alcohol withdrawal, alcohol withdrawal seizures and delirium tremens o environmental exposures – heat-related illnesses; hypothermia; bite wound (human or animal) including a knowledge of tetanus immunization o central nervous system disorders – coma including classification of the causes of coma, demonstration of a knowledge of the Glasgow Coma Scale; seizure including the use of various anticonvulsant agents; suspected TIA or stroke o cardiovascular diseases – chest pain including acute ischemic syndromes, pericarditis, aortic dissection; indications and contraindications for thrombolytic therapy; hypertensive emergencies and urgencies; acute pulmonary edema 13 o respiratory diseases – acute respiratory distress; acute exacerbation of asthma or COPD and differentiate between mild, moderate and severe exacerbations of asthma; suspected pulmonary embolism; community acquired pneumonia and the indications for admission o genitourinary disease – urinary tract infections; renal colic; urethritis, epididymitis, testicular torsion; vaginal bleeding in the pregnant and nonpregnant patient, management of pelvic inflammatory disease; risk factors for ectopic pregnancy o gastrointestinal diseases – upper and lower gastrointestinal bleeding o domestic violence o behavioural and psychiatric disorders – suicidal behaviour; legal criteria for holding patients in the emergency department against their will, differentiate between functional and organic causes of psychosis, indications and contraindications for using physical and chemical restraints Develop technical skills related to the practice of emergency medicine including: maneuvers used to help maintain a patent airway in the compromised patient; proper technique for infiltration of local anesthetic, technique for performing a digital nerve block, ability to suture a simple skin laceration including wound preparation, anaesthesia, suture material selection, wound closure, dressing, and appropriate follow-up care Demonstrate awareness of and appropriate referral to community resources available to emergency medicine patients and their families Communicator Demonstrate the ability to gather history from patients and their families in the emergency room context Demonstrate the ability to gather collateral information from patients’ families and from community agencies and practitioners Effectively communicate information regarding medications to patients Effectively communicate treatment and follow-up plans to the patient Communicate effectively with members of the multidisciplinary team in the emergency medicine setting and liaise effectively with community practitioners and agencies involved with emergency medicine patients and their families Communicate effectively and efficiently with consulting services Scholar Access relevant literature and other resources to guide assessment and management of emergency medicine patients Develop skills in the critical appraisal of literature regarding the diagnosis and treatment of issues in emergency medicine Manager Develop the ability to perform focused histories and physical examination in the time-limited environment of the emergency room Describe and understand the central role of the physician in overall emergency department management 14 Develop time management skills to reflect and balance priorities for patient care, sustainable practice, and personal life Collaborator Describe and understand the roles of allied healthcare professionals, both within the hospital setting and in the community, with respect to the assessment and management of emergency medicine patients Demonstrate appropriate initiation of specialty consultation Health Advocate Demonstrate the capacity to advocate effectively on behalf of emergency medicine patients for the services that they require Identify opportunities for patient counseling and education regarding their medical conditions Educate patients regarding lifestyle modifications that may prevent emergency room visits for certain medical conditions Professional Demonstrate professional attitudes in interactions with patients, families and other healthcare professionals Recognize and appropriately respond to ethical challenges in the emergency medicine setting 15 BEHAVIOURAL NEUROLOGY (COGNITIVE NEUROLOGY) Rotation offered at: SHSC Description: The behavioural neurology rotation provides an opportunity for the PGY1 psychiatry resident to develop knowledge and skills in the assessment and management of patients with cognitive and behavioural disturbances secondary to neurological disease. PGY1 psychiatry residents will develop an organized approach to undertaking a behavioural neurology assessment including detailed cognitive assessment strategies that they can use at the bedside and in the clinic as well as general neurological assessments. They will learn about dementia and other common neurobehavioural disorders. PGY1s will receive their behavioural neurology training at Sunnybrook Health Sciences Centre where they will participate in outpatient clinics, consultation to psychiatric and geriatric inpatients, and on call duties to general neurology. Rotation Specific Objectives: Medical Expert Develop an organized approach to doing a neurobehavioural examination through: o history taking o neurological physical examination o detailed mental status examination o physician administered cognitive testing including the assessment of memory, aphasia, neglect, and apraxia o completion of structured assessment questionnaires o record-keeping on a structured consultation feedback form Develop skills in eliciting and interpreting abnormal neurobehavioural signs Assess and initiate diagnostic and management plans for neurobehavioural disorders including dementia Interpret the reports of EEG and neuroimaging investigations including CT, MRI, and SPECT scanning Review knowledge of neuroanatomy and neurophysiology that is required to localize lesions and recognize abnormalities of function Refine general neurology skills in assessment, diagnosis and management planning with respect to the evaluation of the emergency room patient presenting with neurological symptoms including: o unexplained coma o status epilepticus o acute bacterial and viral infections of the CNS 16 o acute stroke syndromes o acute paralytic disorders Appropriately utilize community resources available to behavioural neurology patients and families Communicator Deliver understandable information to patients and families regarding common issues in behavioural neurology Identify and appropriately address ethical issues with behavioural neurology patients and their families Communicate effectively with members of the multidisciplinary team in the behavioural neurology setting and liaise effectively with community practitioners and agencies involved with behavioural neurology patients and their families Scholar Access relevant literature and other resources to guide assessment and management of behavioural neurology patients Manager Develop the ability to perform appropriately focused histories, mental status and physical examinations in behavioural neurology patients Develop the ability to prioritize and make appropriate allocation of time in the face of competing clinical priorities Collaborator Describe and understand the role of the physician in the behavioural neurology setting Describe and understand the roles of allied healthcare professionals, both within the hospital setting and in the community, with respect to the assessment and management of behavioural neurology patients and their family and friends Collaborate effectively with other members of the behavioural neurology team and community agencies Health Advocate Demonstrate the capacity to advocate effectively on behalf of behavioural neurology patients for the services that they require Professional Demonstrate professional attitudes in interactions with patients, families and other healthcare professionals Recognize and appropriately respond to ethical challenges in the behavioural neurology setting 17 NEUROLOGY Rotation offered at: MSH, SHSC, SMH, UHN Description: The neurology rotation provides an opportunity for the PGY1 psychiatry resident to develop knowledge and skills in the assessment and management of patients with neurological disease. Most rotations include some combination of inpatient and ambulatory experiences. PGY1 psychiatry residents will develop an organized approach to undertaking a neurology assessment. They will learn about common neurological conditions and the management of common neurological emergencies. Rotation Specific Objectives: Medical Expert Develop an organized approach to assessing a patient with neurological complaints through: o history taking – obtaining a complete neurologic history from adults including a collateral history where necessary o an appropriate physical examination o neurological examination – identify if there is unifocal, multifocal or diffuse involvement of the nervous system and, where possible, appropriately localize the lesion(s) based on neurophysiology and neuroanatomy o mental status examination Formulate an appropriate provisional diagnosis and differential diagnoses Outline an appropriate plan for laboratory investigation Outline an appropriate therapeutic plan Develop the necessary technical skills in neurology o Perform a lumbar puncture o Evaluate the relevance of a specific report of common investigative procedures used in neurology including: CSF analysis, electroencephalogram, evoked responses, angiograms, CT and MRI of the neuraxis Be familiar with and able to recognize, assess and treat patients with the following neurological problems: o Neurological emergencies Acute paralysis Bacterial infections of the CNS Status epilepticus Unexplained coma Subarachnoid hemorrhage 18 Myasthenic crises AIDP/Guillain-Barre syndrome o Acute myelopathy o Acute and chronic neuropathies o Ataxia and gain disorders o CNS infections o Cancer & the CNS including metastatic & nonmetastatic neurologic complications of cancer, tumors of the nervous system o Cervical and lumbosacral radiculopathies o Coma and acute encephalopathies o Dementia o Headache syndromes and craniofacial pain o Neuromuscular disorder including neuromuscular junction syndromes (e.g. myasthenia gravis) and myopathies o Neuro-opthalmological disorder (e.g. optic neuritis) o Cranial neuropathies o Movement disorders: parkinsonism, hypokinetic & hyperkinetic disorders o Epilepsy and seizures o Cerebrovascular diseases o Vertigo and dizziness Describe the indications for, side effects and dosages of the major agents used in neurologic therapeutics Describe the major bacteria causing nervous system infections including classification and antibiotic sensitivities Communicator Establish therapeutic relationships with patients/families including being able to obtain and synthesize relevant history from patients/families, listen effectively and discuss appropriate information with patients/families patients and their families Communicate effectively with members of the multidisciplinary team in the neurology setting and to liaise effectively with community practitioners and agencies involved with neurology patients and their families Scholar Access relevant literature and other resources to guide assessment and management of neurology patients Manager Develop the ability to prioritize and make appropriate allocation of time in the face of competing clinical priorities Develop time management skills to reflect and balance priorities for patient care, education, sustainable practice and personal life Collaborator Describe and understand the role of the physician in the neurology setting 19 Describe and understand the roles of allied healthcare professionals, both within the hospital setting and in the community, with respect to the assessment and management of neurology patients and their family and friends Collaborate effectively with other members of the neurology team and community agencies Health Advocate Demonstrate the capacity to advocate effectively on behalf of neurology patients for the services that they require Know about community resources helpful to neurology patients Counsel patients on the importance of taking responsibility for their own wellbeing and recognize the important determinants predisposing to neurological disorders (e.g. risk factors for TIA and stroke, teratogenic effects of anti-epileptic drugs) Professional Demonstrate professional attitudes in interactions with patients, families and other healthcare professionals Recognize and appropriately respond to ethical challenges in the neurology setting To be punctual when attending clinics, consults, rounds, teaching sessions. If unable to attend for legitimate reasons, to notify the attending staff or the senior neurology resident ahead of time. 20 NEUROIMAGING & NEURORADIOLOGY Centralized Teaching Description: Neuroimaging week is a one-week introduction to neuroimaging for the PGY1 psychiatric resident that includes a day in neuroanatomy. The week provides an opportunity to develop knowledge and skills with respect to the appropriate role of neuroimaging in the investigation and follow-up of patients with psychiatric, neuropsychiatric and neurobehavioural disorders. PGY1 psychiatry residents will review fundamental neuroanatomy relevant to neuroimaging and psychiatry, develop an understanding of the basic principles underlying common neuroimaging techniques, increase their ability to understand neuroradiology reports and develop basic skills in reading CT and MRI scans. 21 PALLIATIVE CARE Rotation offered at: MSH, SHSC, SMH, UHN Description: The palliative care rotation provides an opportunity for the PGY1 psychiatry resident to develop knowledge and skills in the provision of end-of-life care that can be applied in other PGY1 rotations and which are applicable to later training in and the practice of psychiatry. PGY1 psychiatry residents will develop an approach to the assessment and management of common medical issues in palliative care patients including the optimal use of opiate and nonopiate analgesic medications, symptom control strategies for common distressing symptoms in palliative patients, and breaking bad news and working with emotionally distressed patients and their families. PGY1s will receive their palliative care training in palliative care inpatient units and consultation services. While the rotation is a part of core medical training, PGY1s will have the opportunity to participate in educational activities related to the psychosocial aspects of palliative care. The University of Toronto Post-Graduate Medical Education Program has developed a web-based learning module on End-of-Life Care that all PGY1s are required to complete at some point during their PGY1 year. If you have not already completed the module, your palliative care rotation is a good time to do the module and the unit tests. You are required to achieve a minimum score of 70% on all of the unit tests and the post-module test in order to successfully complete the module. Rotation Specific Objectives: Medical Expert Assess pain and symptoms effectively via a pain history, appropriate physical exam and relevant investigations Prescribe opioids effectively including initiating dosage, titration, breakthrough dosing and prevention of side-effects. Prescribe adjuvant modalities and medications for pain. Participate in the development of interdisciplinary management plans for other symptoms including fatigue, anorexia, cachexia, constipation, dyspnea, nausea and vomiting, delirium, anxiety and depression Monitor the efficacy of symptom management plans 22 Develop a management plan that appropriately balances disease-specific treatment and symptom management according to the individual needs of the patient and family Document a holistic management plan Identify and assess psychosocial and spiritual issues in end-of-life care and develop and implement a care plan to address these issues in collaboration with other disciplines Describe the elements of the ESAS tool and the Palliative Performance Scale in relation to ongoing assessment of both the management plan and disease trajectory Self-assess one’s own attitudes and beliefs in caring for the dying and how they impact the care provided Communicator Communicate comprehensive information about the common issues of an advanced illness compassionately and effectively including delivering bad news Initiate and participate in effective patient and family meetings Educate patients and family about end-of-life care issues and pain and symptom management Effectively communicate with the interprofessional team and community resources regarding end of life care issues for patient and family Scholar Access relevant literature and other resources to guide assessment and management of palliative care patients Develop skills in the critical appraisal of literature regarding palliative care Manager Develop the ability to perform appropriately focused histories, mental status and physical examinations in palliative care patients Develop time management skills to reflect and balance priorities for patient care, education, sustainable practice and personal life Collaborator Demonstrate effective consultation skills as part of the interprofessional care in formal and informal teams Effectively arrange and coordinate the care of dying patients with the help of an interprofessional team, including the multiple modalities of care available in the hospital and the community Health Advocate Demonstrate the ability to advocate for palliative care patients and their families 23 Professional Demonstrate professional attitudes in interactions with patients, families and other healthcare professionals Recognize and appropriately respond to ethical challenges in the palliative care setting Be aware of emotional reactions to palliative care patients and families including countertransference and counter-reactions in the palliative care setting, and appropriately use available supports including the clinical supervisor and team debriefings to deal with the emotional challenges of palliative care 24 CORE PSYCHIATRY ROTATIONS 25 ADDICTION PSYCHIATRY Rotation offered at: sites CAMH for base rotation with clinical experiences at a variety of Description: The addiction psychiatry elective rotation provides an opportunity for the PGY1 psychiatry resident to develop an understanding of important areas in addiction medicine and addiction psychiatry that will serve as a basis for their further psychiatric training. The rotation is based at CAMH with clinical experiences at a variety of sites. The focus of the PGY1 addiction psychiatry rotation is on creating a foundation for further training by focusing on addiction assessment and treatment in a variety of modalities and settings with a large focus on addiction medicine. Rotation Specific Objectives: Medical Expert Competency in managing acute intoxication and withdrawal conditions Knowledge of the different levels of care and treatment modalities for substance use conditions with and without concurrent disorders Basic assessment of the addiction patient with and without concurrent disorders Basic understanding of the techniques of Motivational Enhancement Communicator Establish effective relationships with patient and their families Interact with community caregivers and other health resources to obtain and synthesize relevant information about the patient Develop a discharge plan for hospitalized patients and learn to involve the family physician, home care and other caregivers in the development of long-term community health planning Learn to communicate effectively and efficiently with colleagues both verbally and through written records (i.e. the medical record, discharge summaries, consultation notes) Collaborator Know when to consult other caregivers appropriately (Addiction and Concurrent Disorder). Manager Develop the understanding of how to effectively balance patient care and health care resources. 26 Develop a knowledge base for understanding the interplay between governments and the health care sector in allocating finite health care resources as well as understand navigating patients between systems (addiction, mental health, justice etc). When the opportunity arises, to help develop effective and efficient patient management strategies. Health Advocate Ability to adopt a preventive approach in clinical practice Identify important determinants of patients' (and public) health. Scholar Development of reflection and self-assessment skills via reflection journal and reflection paper Opportunity to join the Resident Addiction Curriculum Education committee Professional Development of appropriate professional attitudes toward individuals with addiction and concurrent disorders Understand professional obligations to patients and colleagues Exhibit appropriate personal and interpersonal professional behaviours 27 EMERGENCY PSYCHIATRY Rotation offered at: CAMH, SHSC, SMH, UHN Description: The emergency psychiatry rotation provides an opportunity for the PGY1 psychiatry resident to develop an approach to the assessment of patients with common psychiatric emergencies. There is a strong focus on interviewing skills. Knowledge and skills related to the psychopharmacological and psychotherapeutic management of emergency psychiatric patients are developed and enhanced. Special attention is focused on the legal and ethical aspects of emergency psychiatry. Rotation Specific Objectives: Medical Expert Complete a rapid emergency psychiatric assessment interview and appropriate mental status examination Enhance skills in eliciting and interpreting abnormal mental status findings in the emergency psychiatry setting Assess and initiate diagnostic and management plans for the patient with the following presentations: o acute and chronic psychosis o depression o anxiety o potentially explosive situations or violence o self-harm o suicidality o homicidality o substance intoxication or withdrawal o acute situational crisis o developmentally delayed patient presenting with psychiatric emergency, Enhance foundational skills in risk assessment for self-harm and risk to others Make a comprehensive diagnosis using DSM-IV including using the diagnostic criteria for the major psychiatric syndromes of schizophrenia, bipolar I and II disorders, major depression, anxiety disorders, personality disorders Construct a psychiatric formulation for crisis intervention with knowledge of models of crisis intervention and brief therapies. Develop a foundational knowledge of the pharmacological agents used in the treatment of psychiatric emergencies including the indications and contraindications, potential side-effects and common serious drug interactions for medications with a focus on antipsychotics and benzodiazepines 28 Demonstrate understanding of the Mental Health Act and the appropriate use of relevant mental health forms for certification of patients and be able to complete Mental Health Act forms and associated documentation accurately Assess for competency to consent to treatment under the Consent to Treatment Act and complete the required forms and documentation accurately Demonstrate appropriate use of commonly used community resources available to emergency psychiatric patients including crisis services at the base hospital, the Gerstein Centre and crisis phone lines Demonstrate foundational understanding of the concept of institutional transference Describe major medical conditions relevant to the differential diagnosis of behavioural disturbance in the ER and recognize urgent medical problems in psychiatric patients and make appropriate referrals Communicator Develop therapeutic relationships with patients Deliver understandable information to patients and families regarding common psychiatric disorders and common psychiatric emergencies Discuss medicolegal and ethical issues related to psychiatric emergencies with patients and their families Communicate effectively with members of the multidisciplinary team in the emergency setting and liaise effectively with community agencies involved with patients Succinctly present relevant information to supervising staff psychiatrists Scholar Access relevant literature and other resources to guide assessment and management of emergency psychiatric patients Develop skills in the critical appraisal of literature regarding common psychiatric emergencies Actively participate in and contribute to educational environment (e.g. attending and participating in educational rounds, teaching medical students) Manager Demonstrate the ability to prioritize amongst competing clinical priorities Collaborator Describe and understand the role of the psychiatrist in the emergency setting and the systemic issues involved in emergency psychiatry including the gatekeeper function of the emergency department, the consulting role of emergency physicians and psychiatrists, and the pressures from community and institutional systems Demonstrate an understanding of the roles of allied healthcare professionals, both within the hospital setting and in the community, with respect to the assessment and management of psychiatric patients and psychiatric emergencies 29 Collaborate effectively with other members of the health care team and community agencies Know when and how to initiate specialty consultation Health Advocate Demonstrate the capacity to advocate effectively on behalf of psychiatric patients Identify opportunities for patient education regarding their psychiatric conditions Professional Fulfill medical, legal and professional obligations of the psychiatrist Demonstrate responsibility, dependability, self-direction, and punctuality Accept and make constructive use of supervision and feedback Demonstrate collaborative and respectful interactions with patients, families and other health care staff that demonstrates gender and cultural awareness Identify and respond to ethical challenges in the care of emergency psychiatric patients 30 CONSULTATION-LIAISON PSYCHIATRY Rotation offered at: MSH, SHSC, SMH, UHN Description: The consultation-liaison psychiatry rotation provides a one month introduction to the psychiatric care of the medically ill. It provides the PGY1 Psychiatry Resident with the opportunity to gain skills in the management of patients with co-morbid medical and psychiatric illnesses. It allows the trainee the opportunity to reflect on the psychological experience of medical illness and the group dynamics of the health care system. Rotation Specific Objectives: Medical Expert Develop foundational skills in completing focused psychiatric assessment interview and appropriate mental status examination in medical patients with comorbid psychiatric disturbances Develop skills in eliciting and interpreting abnormal mental status findings Assess and initiate diagnostic work-up and management plans for the medical patient with the following psychiatric presentations: o agitation, confusion and delirium o dementia o depression o anxiety o self-harm and suicidality o acute situational crises o behaviour which is difficult for the medical team to manage o personality disorder Foundational knowledge of the pharmacological agents used in the management of psychiatric symptoms in the medically ill with particular emphasis on the management of delirium, anxiety and depression. There is a particular focus on the indications for medication use, potential side-effects and relevant drug interactions and interactions with the co-morbid medical illness(es). Develop or enhance basic skills in providing supportive psychotherapy Demonstrate knowledge and skills related to the use of the Mental Health Act and the Consent to Treatment Act in medically ill patients Communicator Deliver understandable information to patients and families regarding common psychiatric disorders and common psychiatric emergencies in the context of medical illness 31 Discuss medicolegal and ethical issues with patients and their families related to psychiatric issues in the medically ill. Communicate effectively with members of the multidisciplinary team in the medical setting and liaise effectively with community practitioners and agencies involved with patients to obtain collateral information or to develop disposition plans Develop skills in succinct case presentations in the consultation-liaison context Scholar Access relevant literature and other resources to guide assessment and management of psychiatric patients with medical co-morbidities Develop skills in the critical appraisal of literature regarding common psychiatric issues in the medically ill Manager Develop the ability to perform focused histories in patients presenting with psychiatric symptoms in the context of medical illness Prioritize and appropriately allocate time in the face of competing clinical priorities Collaborator Describe and understand the role of the psychiatrist in the medical setting and the pressures from community and institutional systems Describe and understand the roles of allied healthcare professionals, both within the hospital setting and in the community, with respect to the assessment and management of patients with co-morbid medical and psychiatric diagnoses Collaborate effectively with other members of the health care team and community agencies Appropriately initiate specialty consultation Health Advocate Advocate effectively on behalf of psychiatric patients Identify opportunities for patient education regarding their psychiatric conditions Professional Demonstrate professional attitudes in interactions with patients, families and other healthcare professionals Recognize and appropriately respond to ethical challenges in the consultationliaison psychiatry setting Display an ability to appraise oneself and to utilize supervision appropriately Monitor emotional reactions to patients, be aware of countertransference and counter-reactions in the C/L setting and make use of available supports and supervision to deal with the emotional challenges of working with seriously ill and dying patients 32 SELECTIVE & ELECTIVE ROTATIONS 33 SELECTIVE & ELECTIVE ROTATIONS PGY-1 psychiatric residents will choose or develop a one month selective rotation and a one month elective rotations that meets their self-identified learning needs. There are a wide range of selective rotations – you will tailor your learning objectives to meet the rotation that you choose. Elective rotations may be organized in any area of psychiatry or clinical medicine or may be used to gain exposure to research or other academic or scholarly pursuits. 34 PSYCHIATRIC RESEARCH Rotation offered at: site of supervisor identified by resident Description: Psychiatric research is a two month elective rotation for PGY1 residents in the CSS stream. It is arranged with their CSS supervisor. PGY1s who are not in the CSS stream may request one or two months of research time in their PGY1 year. Rotation Specific Objectives: Medical Expert Gain specialized knowledge in a subspecialty area of psychiatry. Communicator Develop academic writing skills related to the design and implementation of a research project Effectively communicate with research supervisors Scholar Access relevant literature and other resources to guide the development of a research project and develop skills in the critical appraisal of literature relevant to the research project Develop an understanding of and foundational skills for preparing applications to research ethics boards Manager Develop time management skills to reflect and balance priorities for scholarly work and personal life Utilize research resources appropriately Collaborator Collaborate effectively with other members of the research team or group Health Advocate To be specified based on project – may not be relevant for all elective rotations Professional Demonstrate professional attitudes in interactions with supervisors and members of the research team Recognize and appropriately respond to ethical challenges in the psychiatric research setting 35 CanMeds 2005 Medical Expert Definition: As Medical Experts, physicians integrate all of the CanMEDS Roles, applying medical knowledge, clinical skills, and professional attitudes in their provision of patient-centered care. Medical Expert is the central physician Role in the CanMEDS framework. Description: Physicians possess a defined body of knowledge, clinical skills, procedural skills and professional attitudes, which are directed to effective patient-centered care. They apply these competencies to collect and interpret information, make appropriate clinical decisions, and carry out diagnostic and therapeutic interventions. They do so within the boundaries of their discipline, personal expertise, the healthcare setting and the patient’s preferences and context. Their care is characterized by up-to-date, ethical, and resource efficient clinical practice as well as with effective communication in partnership with patients, other health care providers and the community. The Role of Medical Expert is central to the function of physicians and draws on the competencies included in the Roles of Communicator, Collaborator, Manager, Health Advocate, Scholar and Professional. Elements: • Integration and application of all CanMEDS Roles for patient care • Core medical knowledge • Patient problem identification • Diagnostic reasoning • Clinical judgment • Clinical decision-making • Application of appropriate therapies • Procedural skill proficiency • Humane care • Application of ethical principles for patient care • Functioning as a consultant • Knowing limits of expertise • Maintenance of competence • Principles of patient safety and avoiding adverse events Communicator Definition: As Communicators, physicians effectively facilitate the doctor-patient relationship and the dynamic exchanges that occur before, during, and after the medical encounter. 36 Description: Physicians enable patient-centered therapeutic communication through shared decision-making and effective dynamic interactions with patients, families, caregivers, other professionals, and other important individuals. The competencies of this Role are essential for establishing rapport and trust, formulating a diagnosis, delivering information, striving for mutual understanding, and facilitating a shared plan of care. Poor communication can lead to undesired outcomes, and effective communication is critical for optimal patient outcomes. The application of these communication competencies and the nature of the doctor-patient relationship vary for different specialties and forms of medical practice. Elements: • Patient-centered approach to communication • Rapport, trust and ethics in the doctor-patient relationship • Therapeutic relationships with patients, families23 and caregivers • Diverse doctor-patient relationships for different medical practices • Shared decision-making • Concordance • Mutual understanding • Empathy • Capacity for compassion, trustworthiness, integrity • Flexibility in application of skills • Interactive process • Relational competence in interactions • Eliciting and synthesizing information for patient care • Efficiency • Accuracy • Conveying effective oral and written information for patient care • Effective listening • Use of expert verbal and non-verbal communication • Respect for diversity • Attention to the psychosocial aspects of illness • Breaking bad news • Addressing end-of-life issues • Disclosure of error or adverse event • Informed consent • Capacity assessment • Appropriate documentation • Public and media communication, where appropriate Key Competencies: Physicians are able to… 1. Develop rapport, trust and ethical therapeutic relationships with patients and families; 2. Accurately elicit and synthesize relevant information and perspectives of patients and families, colleagues and other professionals; 3. Accurately convey relevant information and explanations to patients and families, colleagues and other professionals; 37 4. Develop a common understanding on issues, problems and plans with patients and families, colleagues and other professionals to develop a shared plan of care; 5. Convey effective oral and written information about a medical encounter. EDS 2005 Physician Collaborator Definition: As Collaborators, physicians effectively work within a healthcare team to achieve optimal patient care. Description: Physicians work in partnership with others who are appropriately involved in the care of individuals or specific groups of patients. This is increasingly important in a modern multi-professional environment, where the goal of patient-centred care is widely shared. Modern healthcare teams not only include a group of professionals working closely together at one site, such as a ward team, but also extended teams with a variety of perspectives and skills, in multiple locations. It is therefore essential for physicians to be able to collaborate effectively with patients, families, and an interprofessional team of expert health professionals for the provision of optimal care, education and scholarship. Elements: • Collaborative care, culture and environment • Shared decision making • Sharing of knowledge and information • Delegation • Effective teams • Respect for other physicians and members of the healthcare team • Respect for diversity • Team dynamics • Leadership based on patient needs • Constructive negotiation • Conflict resolution, management, and prevention • Organizational structures that facilitate collaboration • Understanding roles and responsibilities • Recognizing one’s own roles and limits • Effective consultation with respect to collaborative dynamics • Effective primary care – specialist collaboration • Collaboration with community agencies • Communities of practice • Interprofessional health care • Multiprofessional health care • Learning together • Gender issues 38 Key Competencies: Physicians are able to… 1. Participate effectively and appropriately in an interprofessional healthcare team; 2. Effectively work with other health professionals to prevent, negotiate, and resolve interprofessional conflict. Manager Definition: As Managers, physicians are integral participants in healthcare organizations, organizing sustainable practices, making decisions about allocating resources, and contributing to the effectiveness of the healthcare system. Description: Physicians interact with their work environment as individuals, as members of teams or groups, and as participants in the health system locally, regionally or nationally. The balance in the emphasis among these three levels varies depending on the nature of the specialty, but all specialties have explicitly identified management responsibilities as a core requirement for the practice of medicine in their discipline. Physicians function as Managers in their everyday practice activities involving co-workers, resources and organizational tasks, such as care processes, and policies as well as balancing their personal lives. Thus, physicians require the ability to prioritize, effectively execute tasks collaboratively with colleagues, and make systematic choices when allocating scarce healthcare resources. The CanMEDS Manager Role describes the active engagement of all physicians as integral participants in decision-making in the operation of the healthcare system. Elements: • Physicians as active participants in the healthcare system • Physician roles and responsibilities in the healthcare system • Collaborative decision-making • Quality assurance and improvement • Organization, structure and financing of the healthcare system • Managing change • Leadership • Supervising others • Administration • Consideration of justice, efficiency and effectiveness in the allocation of finite healthcare resources for optimal patient care • Budgeting and finance • Priority-setting • Practice management to maintain a sustainable practice and physician health • Health human resources • Time management • Physician remuneration options • Negotiation • Career development • Information technology for healthcare 39 • Effective meetings and committees Key Competencies: Physicians are able to… 1. Participate in activities that contribute to the effectiveness of their healthcare organizations and systems; 2. Manage their practice and career effectively; 3. Allocate finite healthcare resources appropriately; 4. Serve in administration and leadership roles, as appropriate. 05 Physi Health Advocate Definition: As Health Advocates, physicians responsibly use their expertise and influence to advance the health and well-being of individual patients, communities, and populations. Description: Physicians recognize their duty and ability to improve the overall health of their patients and the society they serve. Doctors identify advocacy activities as important for the individual patient, for populations of patients and for communities. Individual patients need physicians to assist them in navigating the healthcare system and accessing the appropriate health resources in a timely manner. Communities and societies need physicians’ special expertise to identify and collaboratively address broad health issues and the determinants of health. At this level, health advocacy involves efforts to change specific practices or policies on behalf of those served. Framed in this multi-level way, health advocacy is an essential and fundamental component of health promotion. Health advocacy is appropriately expressed both by individual and collective actions of physicians in influencing public health and policy. Elements: • Advocacy for individual patients, populations and communities • Health promotion and disease prevention • Determinants of health, including psychological, biological, social, cultural and economic • Fiduciary duty to care • The medical profession’s role in society • Responsible use of authority and influence • Mobilizing resources as needed • Adapting practice, management and education to the needs of the individual patient • Patient safety • Principles of health policy and its implications • Interactions of advocacy with other CanMEDS Roles and competencies Key Competencies: Physicians are able to… 1. Respond to individual patient health needs and issues as part of patient care; 2. Respond to the health needs of the communities that they serve; 40 3. Identify the determinants of health of the populations that they serve; 4. Promote the health of individual patients, communities and populations. Scholar Definition: As Scholars, physicians demonstrate a lifelong commitment to reflective learning, as well as the creation, dissemination, application and translation of medical knowledge. Description: Physicians engage in a lifelong pursuit of mastering their domain of expertise. As learners, they recognize the need to be continually learning and model this for others. Through their scholarly activities, they contribute to the creation, dissemination, application and translation of medical knowledge. As teachers, they facilitate the education of their students, patients, colleagues, and others. Elements: • Lifelong learning • Moral and professional obligation to maintain competence and be accountable • Reflection on all aspects of practice • Self-assessment • Identifying gaps in knowledge • Asking effective learning questions • Accessing information for practice • Critical appraisal of evidence • Evidence-based medicine • Translating knowledge (evidence) into practice • Translating knowledge into professional competence • Enhancing professional competence • Using a variety of learning methodologies • Principles of learning • Role modeling • Assessing learners • Giving feedback • Mentoring • Teacher-student ethics, power issues, confidentiality, boundaries • Learning together • Communities of practice • Research / scientific inquiry • Research ethics, disclosure, conflicts of interests, human subjects and industry relations Key Competencies: Physicians are able to… 1. Maintain and enhance professional activities through ongoing learning; 2. Critically evaluate information and its sources, and apply this appropriately to practice decisions; 3. Facilitate the learning of patients, families, students, residents, other health 41 professionals, the public, and others, as appropriate; 4. Contribute to the creation, dissemination, application, and translation of new medical knowledge and practices. Professional Definition: As Professionals, physicians are committed to the health and wellbeing of individuals and society through ethical practice, profession-led regulation, and high personal standards of behaviour. Description: Physicians have a unique societal role as professionals who are dedicated to the health and caring of others. Their work requires the mastery of a complex body of knowledge and skills, as well as the art of medicine. As such, the Professional Role is guided by codes of ethics and a commitment to clinical competence, the embracing of appropriate attitudes and behaviors, integrity, altruism, personal well-being, and to the promotion of the public good within their domain. These commitments form the basis of a social contract between a physician and society. Society, in return, grants physicians the privilege of profession-led regulation with the understanding that they are accountable to those served. Elements: • Altruism • Integrity and honesty • Compassion and caring • Morality and codes of behaviour • Responsibility to society • Responsibility to the profession, including obligations of peer review • Responsibility to self, including personal care in order to serve others • Commitment to excellence in clinical practice and mastery of the discipline • Commitment to the promotion of the public good in health care • Accountability to professional regulatory authorities • Commitment to professional standards • Bioethical principles and theories • Medico-legal frameworks governing practice • Self-awareness • Sustainable practice and physician health • Self-assessment • Disclosure of error or adverse events Key Competencies: Physicians are able to… 1. Demonstrate a commitment to their patients, profession, and society through ethical practice; 2. Demonstrate a commitment to their patients, profession, and society through participation in profession-led regulation; 3. Demonstrate a commitment to physician health and sustainable practice. 42