YKL-40 is correlated to FEV1 and asthma control test (ACT) in
advertisement

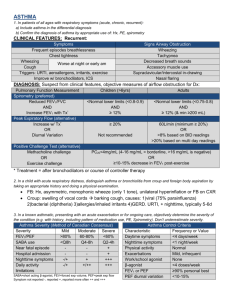
1 2 3 4 YKL-40 is correlated to FEV1 and asthma control test (ACT) in asthmatic patients: influence of treatment 5 Abstract 6 Background: YKL-40, also called chitinase-3-like-1 (CHI3L1) protein, has recently 7 shown its potential as a marker for asthma. The aims of present study were to 8 investigate whether the serum YKL-40 levels are stable or decreased in patients with 9 asthma after appropriate treatment, and to evaluate the correlation of YKL-40 levels 10 to lung function and asthma control test (ACT). 11 Methods: 103 asthmatic patients (mean age 33.1 ± 0.9 years) with newly diagnosed 12 asthma were enrolled in our study. Patients underwent a detailed clinical examination 13 and completed the ACT questionnaire, serum YKL-40 measurement, and spirometry 14 before (visit 1) and 8 weeks after initiation of treatment (visit 2). 15 Results: At visit 2, the median serum YKL-40 level was significantly decreased 16 compared with those at visit 1 (75.2 [55.8-86.8] ng/ml versus 54.5 [46.4-58.4] ng/ml, 17 p<0.001). Serum YKL-40 level was found to have a negative correlation with %FEV1 18 (r=-0.37, p<0.001) and ACT score (r=-0.26, p=0.007) at visit 1. The change in serum 19 YKL-40 levels between two visits were significantly correlated to changes in FEV1 20 (r=-0.28, p=0.006) and ACT score (r=-0.22, p=0.037). Patients with elevated levels of 21 YKL-40 had significantly greater corticosteroid use than patients with lower levels. 22 Conclusions: YKL-40 was found in decreased quantities in the serum of asthmatic 23 patients after appropriate treatment, and its levels correlated with improvements 24 in %FEV1 and ACT. High levels of serum YKL-40 may be refractory to current 25 asthma treatments. 26 27 Trial registration: ChiCTR-OCC-13003316 28 Keywords: asthma, CHI3L1, exacerbation, YKL-40 29 30 31 32 33 1 / 24 34 Introduction 35 36 Asthma is a common chronic disease characterized by acute inflammation of the 37 airways that arises in the context of a complex interaction between genetic factors and 38 the evolving immune system of the infant and the environment to which it is exposed 39 [1,2]. Despite recent guidelines focus on asthma control, many asthmatic patients 40 remains poorly controlled in even under specialist care[3]. The outcomes might have 41 been improved by earlier diagnosis and better monitoring. Therefore, it is urgent to 42 find new biomarkers to measure and monitor the amount of inflammation within the 43 lungs of a patient with asthma and, as a result of better treatment of the disease. 44 Recently, several questions have been put forward on the role of chitinase and 45 chitinase-like proteins in inflammation and tissue remodeling in human disease. 46 The chitinase-like protein YKL-40, also called chitinase 3-like 1 (CHI3L1), is 47 produced at sites of inflammation in many cells and is secreted from macrophages and 48 smooth muscle cells [4]. YKL-40 binds to ubiquitously expressed chitin but is 49 deficient in chitinase activity. Previous studies have demonstrated that YKL-40 was 50 associated with pathologic conditions characterized by aberrant cell growth, tissue 51 inflammation and remodeling, such as several cancers, diabetes, atherosclerosis, 52 rheumatoid arthritis, asthma, chronic obstructive pulmonary disease (COPD), liver 53 fibrosis, idiopathic pulmonary fibrosis and Crohn’s disease [4-14]. For some of these 54 diseases, the measurement of YKL-40 has been proven to be of both diagnostic and 55 prognostic value [5,7,14]. 56 YKL-40 is synthesized in neutrophil precursors and stored in the specific 57 granules of neutrophils. YKL-40 secretion is stimulated by IL-6, IL-17, 58 IL-18-cytokines and released from neutrophils, vascular smooth muscle, macrophages, 59 chondrocytes and cancer cells[15]. YKL-40 has been shown to induce activation of 60 the mitogen-activated protein kinase pathway, nuclear factor-κB transcriptional 61 activity and protein kinase B (Akt) pathway in cell cultures like human colon cell 62 lines and human chondrocytes and synovial cells[16]. YKL-40 also potently 63 stimulates the growth of several types of human fibroblast derived from synovium, 2 / 24 64 adult skin, and fetal lung[15]. Moreover, YKL-40 acts a chemoattractnat for modulate 65 vascular endothelial cell morphology by promoting the formation of branching 66 tubules[17]. A recent study by Tang et al. demonstrated that YKL-40 may be involved 67 in the inflammation of asthma by induction of IL-8 from epithelium, subsequently 68 contributing to BSMC proliferation and migration[18]. Collectively, YKL-40 has a 69 role in inflammation, pathological, fibrosis and tissue remodeling. 70 Chupp et al. demonstrated that YKL-40 was strongly unregulated in the 71 alveolar macrophages and subepithelial basement membrane of asthmatic patients, 72 and that serum YKL-40 level was elevated in asthmatic patients[10]. Duru et al. 73 showed that serum YKL-40 levels were higher in non-smoker asthma patients during 74 acute exacerbation than those of control individuals[19]. Kuepper et al. also indicated 75 that YKL-40 levels were predominantly increased at the site of allergen deposition in 76 response to allergen challenge [20]. A recent study suggested that serum YKL-40 77 levels were significantly elevated in patients with asthma compared with controls, 78 indicating that high levels of serum YKL-40 may be a biological characteristic of the 79 exacerbation of asthma[21]. 80 Although previous studies have reported the elevated levels of YKL-40 in 81 asthmatic patients, the change in serum YKL-40 levels upon treatment in asthmatic 82 patients and its correlations with lung function and asthma control test (ACT) remain 83 unknown. Therefore, the aim of this study was conducted to estimate whether the 84 serum YKL-40 levels are decreased in patients with asthma after introduction of 85 appropriate treatment. Furthermore, the relationships between the serum YKL-40 86 level, lung function and ACT were also investigated in order to evaluate the clinical 87 significance of serum YKL-40 level during the course of the disease. 88 89 Methods 90 Study subjects 91 103 patients (47 women and 56 men, mean age 33.1 ± 0.9 years) were recruited 92 randomly from Outpatient Clinic, Pulmonary Department, Affiliated Hospital of 93 Guangdong Medical College. Patients with no previous diagnosis of asthma 3 / 24 94 presenting with respiratory symptoms were considered eligible for our study when 95 they were (a) cases who were older than 18 years of age, (b) able to perform 96 spirometry, (c) literate in Chinese. Asthma was diagnosed according to the GINA 97 guidelines based on a history of recurrent episodes of wheezing and chest tightness, 98 with or without cough, and impaired spirometry with reversibility in FEV1 of >12% 99 and 200ml after salbutamol administration or hyperresponsiveness to inhaled 100 methacholine[22]. Exclusion criteria were the following: current smoking or smoking 101 history of >5 pack years; oral corticosteroids or respiratory tract infection within the 102 preceding 4 weeks prior to enrolment; any chronic cardiopulmonary disease other 103 than asthma (including COPD); pregnant. We also obtained the specimens from 104 Clinical Research Center of Guangdong Medical College Tissue Bank. Although these 105 samples were not specifically collected for this study, our study was part of a project 106 that examined the molecular mechanism of inflammation in asthma. Bronchial-biopsy 107 specimens were collected from 5 normal subjects who were nonsmokers, 8 patients 108 with mild asthma, 8 patients with moderate asthma and 7 patients with severe asthma. 109 Their basic characteristics matched those in the present study participants. 110 The study protocol was approved by the Ethics of Research Committee of the 111 Medical College of Guangdong (PJ20130016) and was registered on the Chinese 112 Clinical Trial Database (ChiCTR-OCC-13003316). Written informed consent was 113 obtained from all participants. 114 115 Study design 116 At baseline visit, patients underwent a detailed clinical examination and completed 117 pulmonary function test, skin prick test (SPT), serum YKL-40 measurement, and ACT 118 questionnaire. Patients were treated with appropriate medication according to the 119 GINA guidelines [22] and were reevaluated 8 weeks later (visit 2). Serum YKL-40, 120 spirometry and ACT score were measured at follow-up visit. Intermittent asthmatic 121 patients received inhaled salbutamol 100-400 μg per day (Salbutamol Sulfate for 122 Inhalation, GlaxoSmithKline) as needed. Both mild to moderate and severe asthmatics 123 were treatment with low-to medium-dose budesonide (200-800 μg per day) delivered 4 / 24 124 via turbuhalers (AstraZeneca AB) on a regular basis, plus a beta-2 agonist (either a 125 short-acting beta-2 agonist on an as-needed basis or a long-acting beta-2 agonist 126 (Formoterol Fumarate Powder For Inhalation, AstraZeneca AB) on a regular basis) 127 and/or a third controller (e.g., leukotriene antagonists or aminophylline). Adherence to 128 medical treatment was assessed using the Chinese version of Medication Adherence 129 Report Scale for Asthma (MARS-A10) items (Supplemental Table 1). MARS-A10 130 developed by Horne and collaborators is a brief self-measure that has demonstrated 131 good psychometric properties [23]. 132 133 Pulmonary function tests 134 Spirometry was measured with standard spirometric techniques (Jaeger, Germany) at 135 least 6 hours after a patient’s most recent treatment with albuterol, according to 136 American Thoracic Society (ATS) guidelines[24]. Patients were divided into three 137 groups on the basis of severity of asthma, according to GINA [22]: (1) mild asthma 138 (FEV1 ≥80%); (2) moderate asthma (FEV1 60-79%); and (3) severe asthma (FEV1 139 <60%). 140 141 Skin prick test (SPT) and asthma control test (ACT) 142 Atopy was tested with the SPT. Twelve common animal and aeroallergens 143 (ALK-Abello, Horsholm, Denmark) were tested. The test was considered positive if 144 the wheal diameter of at least 3 mm. The ACT questionnaires administered to the 145 patients of this study had been formally translated into Chinese. Patients were 146 classified into three groups based on ACT scores [25]: completely controlled (ACT 147 score=25), partly controlled (ACT score range=20-24), and uncontrolled (ACT score 148 range=5-19). Asthma-related quality of life (QoL) was also measured by using the 149 Mini-Asthma QoL Questionnaire (MiniAQLQ). The mini AQLQ is a validated 150 15-item questionnaire, which assesses the quality of life specifically in relation to 151 asthma[26]. The questionnaire assesses three domains of asthma interference with 152 daily life (symptoms, environmental limitations, and emotions). The total score 153 obtained in the different domains was divided by 15 to obtain the score for each 5 / 24 154 patient, with higher scores being indicative of better quality of life [26]. 155 156 Serum YKL-40 and total serum IgE 157 Serum YKL-40 levels were measured using commercially available enzyme-linked 158 immunosorbent assay (ELISA) kit (Uscn Life Science Inc. Wuhan) according to the 159 manufacturer’s instructions. The minimum detection limit of the YKL-40 assay was 160 12.2 pg/ml. Total serum IgE levels were determined using a fluoroenzyme 161 immunoassay from asthmatic patients. The percentage of peripheral blood eosinophils 162 was detected using a routine blood test. 163 164 Immunohistochemistry 165 Deparaffinized sections (5 μm thick) were immersed in citrate antigen retrieval 166 solution, and preheated to 100°C for 20 minutes. After blocking endogenous 167 peroxidase with immunol staining blocking buffer for 60 min, the slides were then 168 incubated either with a rabbit polyclonal Ab against human YKL-40 (Uscn Life 169 Science Inc., Wuhan, China). The immunoreaction was visualized using 170 3,3-diaminobenzidine chromogen solution (DAB substrate kit, Abcam, Cambridge, 171 UK) and counterstained with hematoxylin according to the manufacturer’s 172 instructions. Quantitative measurements of YKL-40 positive cells in the bronchial 173 tissue were performed according to previous described [27]. Briefly, YKL-40-positive 174 and -negative cells were counted in each biopsy specimen separately in the intact 175 epithelium and the submucosa. Bronchial cells positive for the YKL-40 antibody were 176 expressed as a percentage of total cells. 177 178 Statistical analysis 179 Kolmogorov-Smirnov (KS) test was performed to examine normality of distribution. 180 YKL-40 levels were not normally distributed and the values were compared among 181 the study groups with the use of the nonparametric tests, including the Mann–Whitney 182 U–test and the Kruskal–Wallis test. The interrelationships between different 183 parameters were determined using Spearmans correlation. Receiver operating 6 / 24 184 characteristic (ROC) curve analysis was performed to derive the optimal cutoff point 185 for YKL-40 as a predictor for increase in FEV1 and response to steroid treatment. 186 Data are presented as the mean ± SEM or n (%), unless otherwise stated. GraphPad 187 Prism 5.0 software (GraphPad Software Inc., San Diego, CA, USA) was used for the 188 analyses and graphs. Statistical significance was set at a p value < 0.05. 189 190 Results 191 Patient characteristics 192 A total of 103 patients with newly diagnosed asthma (56 men, 47 women, mean age 193 33.1 ± 0.9) were recruited for our study. They included 72 with mild asthma 194 (intermittent or mild), 20 with moderate asthma and 11 with severe asthma. Sixty-nine 195 patients (67.0%) had at least one positive SPT result. Sensitizations to house dust 196 mites and cockroaches were the most common. The mean baseline serum IgE, blood 197 eosinophils in WBC and body mass index (BMI) were 631.7 kU/L, 5.4% and 21.6 198 respectively. The characteristics of participants in our study were shown in Table 1. 199 During the follow-up visit, five patients were removed because they were 200 unwilling to complete the treatment and refused to continue participating. Finally, 98 201 subjects completed the study and were included in the data analyses. There were no 202 significant differences in baseline characteristics between patients who dropped out 203 and patients who completed the treatment (Supplemental table 2). 204 205 Baseline visit 206 At baseline visit, the mean %FEV1 was 84.1 ± 1.4%; 72 patients (69.9%) had FEV1 207 ≥80%, 20 (19.4%) had FEV1 60-79%, and 11 (10.7%) had FEV1<60% (Table 1). The 208 mean ACT score was 20.6 ± 0.5; 26 patients (25.2%) were completely controlled, 52 209 (50.5%) were partly controlled, and 25 (24.3%) were uncontrolled (Table 1). Patients 210 with completely controlled asthma had statistically lower serum YKL-40 levels than 211 patients with partly controlled (p<0.001) and uncontrolled asthma (p< 0.001), but no 212 differences were detected in the serum YKL-40 levels between partially controlled 213 group and uncontrolled group (Fig. 1a). 7 / 24 214 Serum YKL-40 levels for patients in the severe asthma group were higher than 215 those in the moderate asthma group (85.60 [56.2-94.3] ng/ml vs 76.00 [52.9-86.0] 216 ng/ml; p=0.024) and those in the mild asthma group (85.60 [56.2-94.3] ng/ml vs 217 63.05 [53.6-75.3] ng/ml; p<0.001). To confirm this result, bronchial biopsy specimens 218 specifically stained for YKL-40 in patients with asthma were further evaluated. 219 Quantification of lung YKL-40 expression revealed that YKL-40 expression was 220 higher in mild asthma compared to healthy controls (19.15% [14.60-20.75%] vs 11.70% 221 [9.01-13.85%]; p=0.006). Subgroup analysis revealed that YKL-40 expression was 222 higher in both severe and moderate asthma than mild asthma (41.0% [35.8-44.7%] vs 223 19.2% [14.6-20.8%]; p<0.001 and 29.2% [24.4-33.3%] vs 19.2% [14.6-20.8%]; 224 p<0.001 respectively), with severe asthma exhibiting significantly higher YKL-40 225 levels than mild asthma (41.0% [35.8-44.7%] vs 29.2% [24.4-33.3%]; p=0.002) 226 (Figure 2). The serum YKL-40 level negatively correlated with %FEV1 (r=-0.37, 227 p<0.001) and ACT score (r=-0.26, p=0.007) at baseline visit (Fig.3). 228 229 Visit 2 230 At visit 2, the median serum YKL-40 level was 54.5 [46.4-58.4] ng/ml and 231 mean %FEV1 was 87.8 ± 0.9%; 85 patients (86.7%) had FEV1 ≥80%, 10 (10.2%) had 232 FEV1 60-79%, and 3 (3.1%) had FEV1 <60% (Table 1). The mean ACT score was 233 22.1 ± 0.3. Thirty-one patients (31.6%) were completely controlled, 60 (61.3%) were 234 partly controlled, and 7 (7.1%) were uncontrolled (Table 1). 235 statistically significant differences in serum YKL-40 values among patient groups 236 with different ACT score (Fig. 1b). No correlations between serum YKL-40 237 and %FEV1 or ACT score values were observed at visit 2 (r=-0.13, p=0.210 and r= 238 -0.07, p=0.511, respectively) (Fig. 4). There were no 239 240 Baseline visit versus visit 2 241 As shown in Table 1, there were statistically significant differences in serum 242 YKL-40, %FEV1 value and ACT score between visit 1 and visit 2. Statistically 243 significant correlations were observed between changes (Δ) in YKL-40 and ΔFEV1 8 / 24 244 (r=-0.28, p =0.006) (Fig.5a) as well as between ΔYKL-40 and ΔACT (r=-0.22, 245 p=0.037) (Fig. 5b). 246 level and an improvement in %FEV1 and in ACT score. The mean ΔYKL-40, 247 Δ %FEV1 and ΔACT values differed significantly between two medication groups 248 (Fig. 6). 249 response were assessed based on the low-dose administration of ICS (≤400 μg 250 budesonide per day) and medium to high-dose administration of ICS (>400 μg 251 budesonide per day). Patients receiving low-dose ICS have lower YKL-40 and 252 higher %FEV1 and ACT score at baseline versus those patients receiving medium to 253 high-dose ICS (Table 2). Patients with elevated levels of YKL-40 had significantly 254 greater corticosteroid use than patients with lower levels (table2). Patients who received ICS showed a decrease in serum YKL-40 The outcomes and the relationship between treatment with ICS and 255 By ROC curve analysis, the value of the area under the ROC curve (AUC) for 256 FEV1 and steroid treatment were 0.76 (95%CI 0.67 to 0.86, p<0.001) and 0.75 257 (95%CI 0.63 to 0.85, p=0.002), respectively (Fig. 7). 258 Serum YKL-40 levels were positively correlated with blood eosinophils 259 (r=0.29, p=0.003) and were weakly positively correlated with total IgE levels (r=0.18, 260 p=0.058). No correlations between serum YKL-40 level, FEV1/FVC (%), age, SPT 261 and BMI and Mini-AQLQ were found during the study period. 262 263 Discussion 264 In this study, we further explored the potential role of serum YKL-40 measurement in 265 the management of asthma. The main findings of our study were as follows: (i) 266 elevated YKL-40 levels in asthma patients are associated with disease severity. Serum 267 YKL-40 levels were deceased in asthmatic patients after administration of appropriate 268 treatment; (ii) the serum YKL-40 correlated negatively with %FEV1 and ACT score 269 before asthma treatment; (iii) although these correlations were no longer observed 270 after treatment, changes in serum YKL-40, %FEV1 and ACT score continued to 271 correlate significantly; and (iv) patients who received ICS showed a significant 272 improvement in serum YKL-40, %FEV1 and ACT compared with patients without 273 ICS. Patients with elevated levels of YKL-40 had significantly greater corticosteroid 9 / 24 274 use than patients with lower levels. These results provided evidence of YKL-40 level 275 is implicated in the pathophysiology of asthma. 276 At baseline serum YKL-40 levels in the partly controlled group and uncontrolled 277 group were significantly higher than those in the controlled group, but no differences 278 were detected in the serum YKL-40 levels between the partly controlled group and the 279 uncontrolled group. The reason for this is unclear, but may be explained by the 280 well-known individual variability in the perception of symptoms. Those who were 281 ACT remain uncontrolled (≤19)/YLK-40 levels below the median (≤75.5) 282 (Supplemental Fig. 1A) may have adequately addressed the atopic inflammation in 283 their airways after treatment, but continue to have symptom persistence for other 284 reasons, including co-morbidities (e.g., rhinitis, gastroesophageal reflux disease), 285 noneosinofilic asthma and masquerades of asthma. In comparison, those who were 286 ACT controlled (>19)/YLK-40 levels above the median (>75.5) (Supplemental Fig. 287 1B) were symptomatically controlled, but have evidence of persistent inflammation 288 and could be at risk for future asthma problems. Moreover, those who were ACT 289 uncontrolled (≤19)/YLK-40 levels above the median (>75.5) (Supplemental Fig. 1C) 290 may be allocated in the group of symptom controlled/high level of YKL-40 (>75.5) 291 asthmatics. This could be partly explained by a poor symptom-perception due to 292 adaptation to their level of disease. These data were consistent with previous reports 293 which suggested that asthma evaluation cannot be inferred from single measures of 294 ACT score[28-30]. GINA also recommend that questionnaires addressing the level of 295 asthma control need to be considered along with the objective measurements such as 296 lung function, inflammatory cytokines[22]. To reconcile this issue, we further 297 performed a separate analysis whereby the data was reanalyzed using the asthma 298 severity according to GINA. The data showed serum YKL-40 levels for patients in the 299 severe asthma group were higher than those in the moderate asthma group and those 300 in the mild asthma group. To confirm this result, bronchial biopsy specimens 301 specifically stained for YKL-40 in patients with asthma were further evaluated. 302 Quantification of lung YKL-40 expression revealed that YKL-40 expression was 303 higher in mild asthma compared to healthy controls. Subgroup analysis revealed that 10 / 24 304 severe asthma exhibiting significantly higher YKL-40 levels than mild and moderate 305 asthma. These findings suggest that the ACT questionnaire may convey something 306 that inflammatory markers and spirometry cannot assess. However, asthma evaluation 307 control cannot be inferred from single measures of ACT score and should be 308 considered along with the objective measurements (e.g., biomarkers, lung function). 309 YKL-40 level is upregulated in human asthma and associated with disease severity, 310 suggesting that high levels of YKL-40 may be a biological characteristic of the 311 asthma severity. 312 Statistically significant correlations were observed between serum YKL-40 level 313 and %FEV1, as well as between serum YKL-40 level and ACT score. Specjalski et al. 314 showed that in Polish population, serum levels of YKL-40 were significantly higher in 315 patients with uncontrolled and party controlled asthma compared to controlled 316 asthmatic patients and healthy subjects[31]. Chupp et al. demonstrated that circulating 317 YKL-40 level was correlated with lung function, asthma severity, and the thickness of 318 the subepithelial basement membrane[10]. Additionally, a recent study by Tang et al. 319 showed that serum YKL-40 levels correlated positively with exacerbation attacks and 320 blood eosinophils, but correlated inversely with lung functions[21]. However, the 321 exact role of the serum YKL-40 level in asthma is still under debate. Specjalski et al. 322 showed that no relations were found between YKL-40 and asthma severity or total 323 serum IgE[31]. A recent study by Sohn et al. suggested that no significant associations 324 between CHI3L1 single nucleotide polymorphisms (SNPs) and asthma were observed 325 in an East Asian population [32]. The basis for these discrepancies may be due to 326 ethnic background and differences in CHI3L1 haplotype structures. A promoter single 327 nucleotide polymorphism in the gene encoding YKL-40, CHI3LI rs495028 (131C/G) 328 has associated with features of asthma and serum YKL-40 levels [33,34]. This 329 suggests that CHI3LI gene polymorphism may be influencing a reduction in YKL-40. 330 At visit 2, no correlations between serum YKL-40 and % FEV1 or ACT score 331 were observed. One explanation may be that a majority of patients in our study were 332 mild asthmatics and showed a response in all three measurements after administration 333 of appropriated therapy, minimizing the range of their distribution. However, the 11 / 24 334 changes in serum YKL-40, %FEV1 and ACT score continued to correlate significantly. 335 Furthermore, serum YKL-40 level was declined in asthmatic patients after appropriate 336 treatment. One possible explanation for this result could be that ACT scores were 337 significantly improved in most patients who presented with a mild or stable condition 338 after treatment. This is consistent with previous studies by Chupp et al. and Tang et al. 339 showed that serum YKL-40 levels were higher in patients with asthma exacerbations 340 than in those in a stable condition[10]. In addition, our data demonstrated, as expected, 341 that patients with asthma receiving regular ICS therapy had a significant improvement 342 in serum YKL-40, %FEV1, and ACT. Previous study demonstrated that serum 343 YKL-40 in patients with active rheumatoid arthritis decreased rapidly during 344 prednisolone therapy, suggesting that steroids may have a direct effect on expression 345 of YKL-40[35]. However, it should be noted that patients were treated with ICS but 346 differences in dosing and compliance existed, and serum YKL-40 level may also be 347 influenced by CHI3LI gene polymorphism or other medications such as 348 bronchodilators. Patients with elevated levels of YKL-40 had significantly greater 349 corticosteroid use than patients with lower levels, suggesting that YKL-40 production 350 may be refractory to current asthma treatments and, therefore, may represent an 351 alternative therapeutic target for severe asthma[36]. 352 There are some limitations that need to be considered. Asthmatic patients with 353 newly diagnosis asthma were enrolled in our study and most of them (69.9%, 72/103) 354 were mild asthma patients. Our results may not fully reflect general population of 355 asthmatic patients, especially patients with severe therapy-resistant asthma. The 356 observation period of our patients was relatively short. Additionally, we did not 357 consider to also using the Asthma Control Questionnaire (ACQ) under the assumption 358 that the ACQ has not been validated in the Chinese population and ACT is easier to 359 score and provides the same screening accuracy[37-39]. 360 361 Conclusions 362 In summary, our current findings demonstrate that elevated YKL-40 levels in asthma 363 patients correlate with disease severity. Patients with elevated levels of YKL-40 had 12 / 24 364 significantly greater corticosteroid use than patients with lower levels, suggesting that 365 high levels of serum YKL-40 may be refractory to current asthma treatments. 366 Prospective studies will be required to determine the role of YKL-40 in patients with 367 severe therapy-resistant asthma and whether the YKL-40 gene expression is under the 368 direct control of the corticosteroid. 369 370 Abbreviations 371 ACT: asthma control test; ICS: inhaled corticosteroids; CHI3L1: chitinase 3-like 1; 372 COPD: chronic obstructive pulmonary disease; GINA: Global Initiative for Asthma; 373 SPT: skin prick test; LABA: long acting β2-agonist; SABA: short acting β2-agonist; 374 ATS: American Thoracic Society; FEV1: forced expiratory volume in one second; 375 FVC: forced vital capacity; AQLQ: Asthma QoL Questionnaire. 376 377 Competing interests 378 None of the authors has any conflict of interest with the data published in this 379 manuscript. There are also non-financial competing interests to declare in relation to 380 this manuscript. 381 382 Authors’ Contributions 383 TWL: Performed experiments, analyzed data, wrote manuscript; YYL: performed 384 analyses and assisted in procuring human blood sample, reviewed manuscript; MC: 385 aided in data collection and analyses; DW and DML: performed ELISA and produced 386 graphs and tables; BW and DZC: designed the study and assisted in generating the 387 final manuscript. All authors have read and approved the final manuscript. 388 389 Authors’ information 390 1. Department of Respiratory and Critical Care Medicine, Affiliated Hospital, Institute 391 of Respiratory Diseases, Guangdong Medicine College, Zhanjiang, China. 392 2. Department of Respiratory Medicine, Affiliated Hospital of School of Medicine, 393 Ningbo University, Ningbo, China. 13 / 24 394 395 Acknowledgements 396 This work was supported by grant of the Medical Scientific Research Project of 397 Guangdong Province, China (No. A2012430) and Natural Science Foundation of 398 Ningbo (No. 2012A610257). 399 400 References 401 1. Wark PA, Murphy V, Mattes J. The interaction between mother and fetus and 402 the development of allergic asthma. Expert Rev Respir Med 2014,8:57-66. 403 2. Collison A, Li J, Pereira de Siqueira A, Zhang J, Toop HD, Morris JC, Foster PS, 404 Mattes J. Tumor necrosis factor-related apoptosis-inducing ligand regulates 405 hallmark features of airways remodeling in allergic airways disease. Am J 406 Respir Cell Mol Biol 2014,51:86-93. 407 408 3. Gaga M, Papageorgiou N, Zervas E, Gioulekas D, Konstantopoulos S: Control of asthma under specialist care: is it achieved? Chest 2005, 128:78-84. 409 4. Boot, G. R., A. E. van Achterberg, B. E. van Aken, G. H. Renkema, M. J. H. M. 410 Jacobs, J. M. Aerts, C. J. de Vries. Strong induction of members of the chitinase 411 family of proteins in atherosclerosis. Arterioscler. Thromb. Vasc. Biol 1999, 412 19:687-694. 413 5. Johansen, J. S., B. V. Jensen, A. Roslind, D. Nielsen, P. A. Price. Serum YKL-40, a 414 new prognostic biomarker in cancer patients? Cancer Epidem. Biomarkers 415 Prev 2006, 15:194-202. 416 6. Johansen, J. S., P. Chrisoffersen, S. Moller, P. A. Price, J. H. Henriksen, C. 417 Garbarsch, F. Bendtsen. Serum YKL-40 is increased in patients with hepatic 418 fibrosis. J. Hepatol 2006, 32:911-920. 419 7. Kucur, M., F. K. Isman, B. Karadag, V. A. Vural, S. Tavsanoglu. Serum YKL-40 420 levels in patients with coronary artery disease. Coron Artery Dis 2007, 18: 421 391-396. 422 423 8. Kim, S. H., K. Das, S. Noreen, F. Coffman, M. Hameed. Prognostic implications of immunohistochemically detected YKL-40 expression in breast cancer. World 14 / 24 424 J Surg Oncol 2007, 5:17. 425 9. Rathcke, C. N., J. S. Johansen, H. Vestergaard. YKL-40, a biomarker of 426 inflammation, is elevated in patients with type 2 diabetes and is related to 427 insulin resistance. Inflamm Res 2006, 55:53-59. 428 10. Chupp GL, Lee CG, Jarjour N, Shim YM, Holm CT, He S, Dziura JD, Reed J, 429 Coyle AJ, Kiener P, Cullen M, Grandsaigne M, Dombret MC, Aubier M, Pretolani 430 M, Elias JA. A chitinase-like protein in the lung and circulation of patients 431 with severe asthma. N. Engl. J. Med 2007, 357:2016-2027. 432 11. Furuhashi K, Suda T, Nakamura Y, Inui N, Hashimoto D, Miwa S, Hayakawa H, 433 Kusagaya H, Nakano Y, Nakamura H, Chida K. Increased expression of YKL-40, 434 a chitinase-like protein, in serum and lung of patients with idiopathic 435 pulmonary fibrosis. Respir Med 2010, 104:1204-1210. 436 12. Létuvé S, Kozhich A, Arouche N, Grandsaigne M, Reed J, Dombret MC, Kiener 437 PA, Aubier M, Coyle AJ, Pretolani M. YKL-40 is elevated in patients with 438 chronic obstructive pulmonary disease and activates alveolar macrophages. 439 J Immunol 2008, 181:5167-5173. 440 13. Fantino E, Gangell CL, Hartl D, Sly PD, AREST CF. Airway, but not serum or 441 urinary, levels of YKL-40 reflect inflammation in early cystic fibrosis lung 442 disease. BMC Pulm Med 2014, 14:28. 443 14. Holmgaard DB, Mygind LH, Titlestad IL, Madsen H, Pedersen SS, Johansen JS, 444 Pedersen C. Plasma YKL-40 and all-cause mortality in patients with chronic 445 obstructive pulmonary disease. BMC Pulm Med 2013, 13:77. 446 15. Zhu Z, Zheng T, Homer RJ, Kim YK, Chen NY, Cohn L, Hamid Q, Elias JA. 447 Acidic mammalian chitinase in asthmatic Th2 inflammation and IL-13 448 pathway activation. Science 2004, 304:1678-1682. 449 16. Rathcke CN, Johansen JS, Vestergaard H. YKL-40, a biomarker of 450 inflammation, is elevated in patients with type 2 diabetes and is related to 451 insulin resistance. Inflamm Res 2006, 55:53-59. 452 453 17. Malinda KM, Ponce L, Kleinman HK, Shackelton LM, Millis AJ. Gp38k, a protein synthesized by vascular smooth muscle cells, stimulates directional 15 / 24 455 migration of human umbilical vein endothelial cells. Exp Cell Res 1999, 250:168-173. 456 18. Tang H, Sun Y, Shi Z, Huang H, Fang Z, Chen J, Xiu Q, Li B. YKL-40 induces 457 IL-8 expression from bronchial epithelium via MAPK (JNK and ERK) and 458 NF-κB pathways, causing bronchial smooth muscle proliferation and 459 migration. J Immunol 2013, 190: 438-446. 454 460 19. Duru S, Yüce G, Ulasli SS, Erdem M, Kizilgün M, Kara F, Ardıc S. The 461 Relationship between Serum YKL-40 Levels and Severity of Asthma. Iran J 462 Allergy Asthma Immunol 2013, 12:247-2453. 463 464 20. Kuepper M, Bratke K, Virchow JC. Chitinase-like protein and asthma. N Engl J Med 2008, 358:1073-1075. 465 21. Tang H, Fang Z, Sun Y, Li B, Shi Z, Chen J, Zhang T, Xiu Q. YKL-40 in 466 asthmatic patients, and its correlations with exacerbation, eosinophils and 467 immunoglobulin E. Eur Respir J 2010, 35:757-760. 468 22. Global Initiative for Asthma. GINA Report: Global strategy for asthma 469 management and prevention 470 (accessed 20 December 2012). (2011 Update). http://www.ginasthma.com 471 23. Mora PA, Berkowitz A, Contrada RJ, Wisnivesky J, Horne R, Leventhal H, Halm 472 EA. Factor structure and longitudinal invariance of the Medical Adherence 473 Report Scale-Asthma. Psychol Health 2011; 26:713-727. 474 475 24. American Thoracic Society. Standardization of spirometry (1994 update). Am J Respir Crit Care Med 1995, 152:1107-1136. 476 25. Nathan RA, Sorkness CA, Kosinski M, Schatz M, Li JT, Marcus P, Murray JJ, 477 Pendergraft TB. Development of the asthma control test: a survey for 478 assessing asthma control. J Allergy Clin Immunol 2004, 113:59-65. 481 26. Juniper EF, Guyatt GH, Cox FM, Ferrie PJ, King DR. Development and validation of the Mini Asthma Quality of Life Questionnaire. Eur Respir J 1999, 14:32-38. 482 27. Xanthou G, Alissafi T, Semitekolou M, et al. Osteopontin has a crucial role in 483 allergic airway disease through regulation of dendritic cell subsets. Nat Med 484 2007, 13: 570-578. 479 480 16 / 24 485 28. Jia CE, Zhang HP, Lv Y, Liang R, Jiang YQ, Powell H, Fu JJ, Wang L, Gibson PG, 486 Wang G. The Asthma Control Test and Asthma Control Questionnaire for assessing asthma control: Systematic review and meta-analysis. J Allergy Clin Immunol 2013, 131:695-703. 29. Piacentini GL, Peroni DG, Bodini A, Bonafiglia E, Rigotti E, Baraldi E, Liu AH, Boner AL. Childhood Asthma Control Test and airway inflammation evaluation in asthmatic children. Allergy 2009, 64:1753-1757. 30. Senna G, Passalacqua G, Schiappoli M, Lombardi C, Wilcock L. Correlation 487 488 489 490 491 492 494 among FEV1, nitric oxide and asthma control test in newly diagnosed asthma. Allergy 2007, 62:207-208. 495 31. Specjalski K, Jassem E. YKL-40 protein is a marker of asthma. J Asthma 2011, 493 496 48:767-772. 497 32. Sohn MH, Lee JH, Kim KW, Kim SW, Lee SH, Kim KE, Kim KH, Lee CG, Elias 498 JA, Lee MG. Genetic variation in the promoter region of chitinase 3-like 1 is 499 associated with atopy. Am J Respir Crit Care Med 2009, 179: 449-456. 500 33. Ober C, Tan Z, Sun Y, Possick JD, Pan L, Nicolae R, Radford S, Parry RR, 501 Heinzmann A, Deichmann KA, Lester LA, Gern JE, Lemanske RF Jr, Nicolae DL, 502 Elias JA, Chupp GL. Effect of variation in CHI3L1 on serum YKL-40 level, 503 risk of asthma, and lung function. N Engl J Med 2008, 358:1682-1691. 504 34. Konradsen JR, James A, Nordlund B, Reinius LE, Söderhäll C, Melén E, 505 Wheelock AM, Lödrup Carlsen KC, Lidegran M, Verhoek M, Boot RG, Dahlén B, 506 Dahlén SE, Hedlin G. The chitinase-like protein YKL-40: a possible biomarker of 507 inflammation and airway remodeling in severe pediatric asthma. J Allergy Clin 508 Immunol 2013, 132:328-335. 509 35. Johansen JS, Stoltenberg M, Hansen M, Florescu A, Hørslev-Petersen K, 510 Lorenzen I, Price PA. Serum YKL-40 concentrations in patients with 511 rheumatoid arthritis: relation to disease activity. Rheumatology 1999, 512 38:618-626. 513 36. Hartl D, Lee CG, Da Silva CA, Chupp GL, Elias JA. Novel biomarkers in 514 asthma: chemokines and chitinase-like proteins. Curr Opin Allergy Clin 515 Immunol 2009, 9:60-66. 516 37. Jia CE, Zhang HP, Lv Y, Liang R, Jiang YQ, Powell H, Fu JJ, Wang L, Gibson PG, 17 / 24 517 Wang G. The Asthma Control Test and Asthma Control Questionnaire for 518 assessing asthma control: Systematic review and meta-analysis. J Allergy Clin 519 Immunol 2013,131:695-703. 520 38. Zhou X, Ding FM, Lin JT, Yin KS. Validity of asthma control test for asthma 521 control assessment in Chinese primary care settings. Chest 2009,135:904-910. 522 39. Zhou X, Ding FM, Lin JT, Yin KS, Chen P, He QY, Shen HH, Wan HY, Liu CT, Li 523 J, Wang CZ. Validity of Asthma Control Test in Chinese patients. Chin Med J 524 (Engl) 2007, 120:1037-1041. 525 526 527 528 529 530 531 532 533 534 535 536 537 538 539 540 541 542 543 544 545 546 547 548 549 550 551 552 553 554 555 556 18 / 24 557 Figure legends 558 559 Fig. 1 Classification of patients based on ACT score at baseline visit (a) and visit 2 (b). 560 Note: ***p < 0.0001; NS: not significant. Horizontal bars indicate mean values. 561 562 Fig. 2 YKL-40 is unregulated in the bronchial tissue of patients with asthma. Specific 563 staining for YKL-40 is brown, whereas nuclei are stained blue. Representative 564 photomicrographs are present from A) a healthy individual and B) a patient with mild 565 asthma and C) a patient with moderate asthma, and D) a patient with severe asthma. 566 YKL-40 positive and negative cells were counted in the epithelium and submucosa 567 (expressed as a percentage of total cells). Data are presented as medians. E) YKL-40 568 is increased in both severe and moderate asthma compared with mild asthma, with 569 significant difference found between the two patient groups. 570 571 Fig. 3 Correlation of serum YKL-40 levels to FEV1 (a) and ACT score (b) at baseline 572 visit. Note: FEV1, forced expiratory volume in one second; ACT, asthma control test. 573 574 Fig. 4 Correlations of serum YKL-40 levels to (a) FEV1 and (b) ACT score at visit 2. 575 Note: FEV1, forced expiratory volume in one second; ACT, asthma control test. 576 577 Fig. 5 Correlation of changes (Δ) in three parameters between the two visits. 578 Statistically correlations were observed (a) between ΔYKL-40 and ΔFEV1; (b) 579 between ΔYKL-40 and ΔACT. Note: FEV1, forced expiratory volume in one second; 580 ACT, asthma control test. 581 582 Fig. 6 Changes in asthma parameters in patient groups according to medication. 583 Note: FEV1, forced expiratory volume in one second; ACT, asthma control test. ICS, 584 inhaled corticosteroids; ICS (+), patients with ICS treatment; ICS (-), patients without 585 ICS treatment. 586 19 / 24 587 Fig.7 Receiver operating characteristic curve showing YKL-40 as a predictor for 588 increase in FEV1 after treatment (black line) and predict response to steroid treatment 589 (red line). Sens, sensitivity; Spec, specificity; AUC, area under the ROC curve. 590 591 Supplemental Fig. 1 Correlation of serum YKL-40 levels to ACT score at baseline 592 visit. A: ACT remain uncontrolled (≤19)/YLK-40 levels below the median (≤75.5); B: 593 ACT controlled (>19)/YLK-40 levels above the median (>75.5); C: ACT uncontrolled 594 (≤19)/YLK-40 levels above the median (>75.5). 595 596 597 598 599 600 601 602 603 604 605 606 607 608 609 610 611 612 613 614 615 616 617 618 619 620 621 622 623 624 625 626 20 / 24 Table 1 Characteristic of the study participants* Characteristic Visit 1 (n = 103) P-value Visit 2† (n = 98) Female, n (%) 47 (45.6) 45 (45.9) NS Age, yrs 33.1 ± 0.9 33.2 ± 0.9 NS Body mass index 21.6 ± 0.3 21.4 ± 0.2 NS Nonsmokers, n (%) 81 (78.6) NA Ex-smokers, n (%) 22 (21.4) NA Atopic by skin prick, n (%) 69 (67.0) NA Total IgE, kU/L 631.7 ± 94.1 568.4 ± 86.8 NS Eosinophil in WBC% 5.4 ± 0.4 4.0 ± 0.3 < 0.001 FEV1/FVC, % 72.1 ± 0.6 74.9 ± 0.8 0.0026 FEV1, % predicted 84.1 ± 1.4 87.8 ± 0.9 0.0270 ≥80%, n (%) 72 (69.9) 85 (86.7) 60-79%, n (%) 20 (19.4) 10 (10.2) < 60%, n (%) 11 (10.7) 3 (3.1) YKL-40, ng/ml 75.2 (55.8-86.8) 54.5 (46.4-58.4) < 0.001 AQLQ 5.19 ± 0.11 5.35 ± 0.10 0.2937 ACT score 20.6 ± 0.5 22.1 ± 0.3 0.0101 25, n (%) 26 (25.2) 31 (31.6) 20-24, n (%) 52 (50.5) 60 (61.3) 5-19, n (%) 25 (24.3) 7 (7.1) *Data are presented as mean ± SEM or n (%), except for YKL-40, median (IQR). Note: FEV1, forced expiratory volume in one second; FVC, forced vital capacity; AQLQ, Asthma Quality of Life Questionnaire; ACT, asthma control test; NS, not significant; NA, not assessed. † Five patients were dropped out. 627 628 629 630 631 632 633 634 635 636 637 638 639 640 641 642 21 / 24 Table 2 Efficacy results in asthma patients at baseline and after treatment with budesonide Variable ≤400 μg budesonide per day (n=50) Baseline >400 μg budesonide per day (n=31) Visit 2 Baseline Visit 2 (2.3) * 82.0 (1.8) ♯ § FEV1, % predicted 90.8 (0.8) 91.2 (0.6) 71.6 ACT score 21.3 (0.7) 22.4 (0.5) 19.1 (0.6) 22.5 (0.4) ♯ 59.1 (54.3-86.6) 47.5 (40.3-55.3) ♯ 86.2 (56.4-96.7) * 55.7 (43.8-63.7) ♯ YKL-40, ng/ml Data are presented as mean ± SEM, except for YKL-40, median (IQR). ♯p< 0.001 vs. baseline. § p< 0.001 vs. baseline (≤400 μg budesonide per day). *p< 0.01 vs. baseline (≤400 μg budesonide per day). 643 644 645 646 647 648 649 650 651 652 653 654 655 656 657 658 659 660 661 662 663 664 665 666 667 668 669 670 671 672 673 674 675 676 677 22 / 24 Supplemental Table 1 The Medication Adherence Report Scale for Asthma (MARS-A10) Item 1. I only use my [Name of Medicine] when I need it 2. I only use it when I feel breathless 3. I decide to miss out a dose 4. I try to avoid using it 5. I forget to take it 6. I alter the dose 7. I stop taking it for a while 8. I use it as a reserve, if my other treatment doesn’t work 9. I use it before doing something which might make me breathless 10. I take it less than instructed 678 679 680 681 682 683 684 685 686 687 688 689 690 691 692 693 694 695 696 697 698 699 700 701 702 703 704 705 706 707 708 709 23 / 24 Supplemental table 2 Characteristics of the study participants and participants excluded* Study participants Participants excluded Characteristic P-value (n = 98) (n = 5) Female, n (%) 45 (45.9) 2 (40.0) 0.63 Age, yrs 32.7 ± 0.8 34.1 ± 0.3 0.69 BMI 21.8 ± 0.3 21.5 ± 0.2 0.82 Total IgE, kU/L 633.5 ± 93.6 618.3 ± 36.1 0.97 Eosinophil in WBC% 5.3 ± 0.4 5.0 ± 0.2 0.86 FEV1/FVC, % 71.6 ± 0.6 72.8 ± 0.3 0.65 FEV1, % predicted 84.6 ± 1.4 83.9 ± 0.7 0.91 YKL-40, ng/ml 75.7 (56.1-85.3) 74.6 (52.4-83.7) 0.60 ACT score 20.1 ± 0.5 20.9 ± 0.2 0.72 AQLQ 5.11 ± 0.11 5.41 ± 0.09 0.54 *Data are presented as mean ± SEM or n (%), except for YKL-40, median (IQR). Note: BMI, Body mass index; FEV1, forced expiratory volume in one second; FVC, forced vital capacity; ACT, asthma control test; AQLQ, Asthma Quality of Life Questionnaire. 710 711 712 713 714 715 716 717 718 719 720 721 722 723 724 725 726 727 728 24 / 24