Report of the project monitoring and seminar trip to Tanzania
advertisement

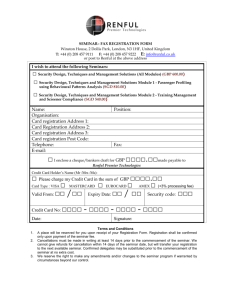
1 “Psychiatry in primary health care – Teaching and support in Tanzania 3” and “Improving Palliative Care in Ilembula Lutheran Hospital” Report of the project monitoring and seminar trip to Tanzania 11.-25.10.2014 Participants: Dr Elina Lind, Secretary for Foreign Mission, FCMS Dr Tapio Pitkänen, Project Coordinator (Psychiatry in PHC) Dr Liisa Laula, Specialist in Psychiatry (Dr Leena Uusitalo participated at her own cost) The purpose of the trip was: 1) to conduct the last annual monitoring visit to the four partnership hospitals of the psychiatric project, Mchukwi, Matema, Itete and Ilembula, 2014 being the final (extension) year of the project 2) to participate in the Mental Health Seminar for Primary Health Providers in Mbeya in the 15th to 17th Oct 3) in Ilembula also to monitor the Palliative Care Project, started this year 11.10. Saturday Departure from Helsinki-Vantaa at 7:00 (via Amsterdam), arrival in Dar es Salaam at 21:45. Overnight at the Double View Hotel in Dar es Salaam. 12.10. Sunday 10 o’clock Sunday service at Kijitonyama Lutheran Church. After the service lunch with Mrs Caroline Shedafa and her family at their home. Mrs Shedafa conducted the evaluation of the psychiatric project in 2012; the recommendations of the evaluation were carefully considered at the time, and have influenced the plans of the two extension years of the project, 2013 and 2014. Consequently, major emphasis has been given on trying to strengthen the sustainability of mental health work within the project catchment areas after the project funding ceases. The original plan was to travel to Mchukwi already on Sunday, but a few days before departure from Finland we were informed that the seminar (for government primary health care workers) that had been planned for 13th to 14th Oct had to be postponed, due to another seminar at Bagamoyo, arranged by the Ministry of Health (MOH). Thus, there was no need to be in Mchukwi by early morning, and the decision was to stay another night in Dar es Salaam. This gave us an opportunity to meet the new scholarship student of the FCMS, Dr Emmanuel Owden Mwalumuli on Sunday evening at the hotel. 13.10. Monday - Mchukwi Picked by Mchukwi Hospital vehicle at 9:30 am from the hotel. Arrived in Mchukwi at around 1 pm. Discussions with various staff members followed by meeting in the afternoon. Present at the meeting: Administrator Hyasinta Maneno, Accountant John Nsongoma, N/O, Mental Health Coordinator Gertruda 2 Kabika, N/O, psychiatric nurse Azory John Nyenza and the FCMS team Drs Elina Lind, Tapio Pitkanen, Liisa Laula and Leena Uusitalo. Dr-in-charge Zacharia Rukeba was busy at the operating theatre and could not attend the meeting, so we had separate discussions with him. General notes: Financial situation of Mchukwi Hospital is still very challenging. Nevertheless, some renovations had been made during the past year (with private donations), and the key staff members that we met were very committed and determined to make a way forward. One example of this is the plan of starting a nursing school at the hospital to help combat the problem of staff shortage in future. At present, quick turnover of qualified staff is a problem. The benefits in government posts are much better, causing qualified staff to leave the hospital for more attractive jobs in government institutions. Since April/May the price of the internet satellite connection that the hospital had raised to about TSH 1 million/month (about 500€). That was far too expensive, and now there is no internet at the hospital. Some staff members use mobile connections, but for bigger files to be sent (or received) by email the accountant has to travel to Kibiti (about 8km). Between July 2013 and May 2014 Mchukwi Hospital had a service agreement with the government; treatment for pregnant mothers, children under 5 and elderly people was supposed to be given free of charge and the costs subsidised by the government. This lead to remarkable increase in patient numbers, especially deliveries. However, the government subsidy was constantly delayed and never to full amount (less than agreed; about 55% of the true costs and even that was several months late). The hospital could not afford treating exempted patient groups free of charge, and decision was made to discontinue the service agreement. Since then services are charged again and the increase in patient numbers has stopped. Prices are moderate and only cover about half of the actual costs, but at least there are no delays in getting the payments. There is a government health insurance scheme; by paying TSH 5000/year/family treatment would be given free. However, many people do not trust the scheme, and therefore are not paying. The coverage is far from being adequate. For service providers the problem is that payments from the insurance, too, often come very late. Hospital management staff would be very keen to continue cooperation with the FCMS in a new project in future. However, the most urgent priority area that they recognize is mother and child health care. It is undoubtedly true that safe deliveries, as well as good care of pregnant mothers and babies, are vitally important, also in preventing complications that may lead to epileptic seizures or even mental retardation. Yet, extending prevention of mental disorders to cover safe motherhood was seen to be beyond the scope of our concept. Moreover, mother and child health care are very much a priority of the MOH of Tanzania; thus, the government should be pressed to provide adequate resources. Therefore, although extremely important, it was felt that at present FCMS is not willing to be involved in a project that would mainly focus on mother and child health. About psychiatric services: Village outreach work was discontinued from the beginning of 2014 due to lack of funds. No alternative source of funding could be found to continue services as before. Prior to cessation of the outreach, all villages were informed. The nearby health facilities were informed that mental health patients should visit Mchukwi Hospital OPD for drug collection and evaluation. The psychiatric nurses continue to treat mental patients at the hospital out-patient clinic. Till now, less than 30% of the previous patients (285 out of 971 in 2013; most of them adult epileptic patients) 3 are regularly coming to the hospital to get their medicine. Presumably there are many patients in the villages without care. Some patients were without medication 2-6 months and then returned. Some may have sought treatment from other service providers. Before the outreach was stopped, all patients were given a card telling their diagnosis and treatment; this was to help them get correct treatment in government health posts or other facilities. In 30th August a seminar about mental health was conducted for the Government Village chairpersons (outreach villages), Rufiji Council chairperson, District Medical Officer, District Mental Health Coordinator, Community Health Management Team members and other selected participants within Rufiji District (47 participants, including 11 from Mchukwi Hospital itself). Following the seminar, the Community Health Management Team (CHMT) agreed that mental health will be included in annual budget. Villagers are also encouraged to join in community health fund to be able to finance their health needs, including mental health drugs. Even if the outreach service now has been stopped many achievements could be listed. Overall knowledge and awareness about mental disorders has greatly improved in the villages. People now know that mental disorders are not caused by demons, and that they can be treated. The change of attitude is remarkable compared to what the beliefs were before the project started. Also new patients are still coming to seek help. Hospital staff is more aware and more skilful in diagnosing and treating mental disorders. The seminar for government primary health care workers that now had to be postponed will be held before the end of 2014. There has already been communication between the government health workers and the mental health professionals of Mchukwi, and the seminar aims at strengthening cooperation. One of the problems at government health facilities – apart from lack of skills - is lack of medicines; they are often out of stock. Regarding the seminar, a question was raised by the hospital administrator, whether it would be possible to add funds for follow up/mentoring visits by psychiatric nurses of Mchukwi Hospital to government health posts after the seminar. After some discussion it was decided that TSH 500 000 (about 250€) will be added to the seminar budget (either from the project funds or FCMS own funding) to conduct one follow up visit to all those 14 health posts that will participate in the seminar. After receiving a report with initial feedback about the follow up visits (whether found useful), FCMS may consider funding such follow up/mentoring visits 2-4 times a year even after the project finishes to further facilitate the handing over process. 15 copies of Mental Health in Primary Care (Huduma za Afya ya Akili Ngazi ya Msingi) –books (published by MEHATA) were given to be distributed to the participants of the seminar. 14.10. Tuesday Travelling day from Mchukwi to Mbeya: taken by Mchukwi Hospital vehicle to Dar es Salaam Airport; FastJet flight from there to Songwe airport; shuttle bus from Songwe airport to Mbeya city (about 20km). Dr Paul Lawala, the psychiatrist of Mbeya Referral Hospital, came to meet and welcome us at Mbeya Hotel. 15.-17.10. Wednesday to Friday - Mental Health Seminar for Primary Health Providers in Mbeya The seminar had been planned in close cooperation with Dr Paul Lawala. He, together with clinical psychologist Liness Ndelwa and psychiatrist Francis Benedict from Njombe had prepared most of the lectures. On behalf of our Finnish team Dr Tapio Pitkanen presented an overview about the experiences of 4 the psychiatric project over the years, and psychiatrist Liisa Laula gave lectures about ‘Psychotic disorders’ and ‘Mental development in childhood and adolescence’. All lecture notes had been printed and bound into a booklet that was given to participants, as well as similarly bound WHO Intervention Guide for mental, neurological and substance use disorders in non-specialized health settings. The notes were in English, but the lectures, as well as discussions were mainly held in Swahili. Even without understanding the language it was encouraging to see how actively the participants contributed in sharing experiences, views and ideas. Overall, arrangements for the seminar were excellent, and it seemed that the participants also appreciated it. The seminar was also acknowledged by the Executive Director of Mbeya Referral Hospital, Dr Mpoki M. Ulisubisya, who visited the seminar to welcome the participants on Thursday. A short visit to the Psychiatric Unit of Mbeya Referral Hospital was made after the second seminar day. There are 8 beds for female and 16 beds (+ a number of mattresses on the floor) for male patients in the psychiatric ward. In psychiatric OPD there are now 5 consultation rooms – the rooms for a social worker and an occupational therapist are still waiting to be occupied by relevant staff members ie. those posts have not been filled yet. The rest, 20 copies of Mental Health in Primary Care (Huduma za Afya ya Akili Ngazi ya Msingi) –books were distributed to the participants of the seminar in the last day. A separate report of the seminar by Dr Paul Lawala, including the list of the participants, is attached, as well as the seminar programme. According to Dr Lawala the lack of support for mental health work is obvious. There are 2 specialized psychiatrists in the area, Dr Lawala in Mbeya and Dr Benedict in Njombe. Because of poor working conditions at Njombe Hospital, Dr Benedict is seriously considering leaving. In the Ministry of Health there is a person nominated to be responsible for mental health work nationwide, yet, he has never visited Mbeya. Therefore, a lot of ‘aggressive advocacy’ is needed both in the national, regional and local level to secure resources and win appreciation for mental health work. After the third seminar day, on Friday afternoon, the vehicle of the Palliative Care Team of Ilembula Hospital came to take us to Ilembula. Arrived in Ilembula just before dark. Before departing we agreed to meet with Dr Paul Lawala once more over lunch at Mbeya Hotel on Friday the 24th on our way to Songwe airport and back to Finland. 18.-19.10. Saturday to Sunday - Ilembula The two days of the weekend were mainly free of official meetings. On Sunday after the church service (7am) in the afternoon we were invited to the home of the hospital treasurer David Kikungwe and the same evening to the home of the administrator Bryceson Mbilinyi. Both visits, although informal, gave us a chance to talk about the situation of the hospital in general, as well as the matters concerning the two projects, psychiatric and palliative. 20.10. Monday – Ilembula Monday was the day for the official meetings, the psychiatric project in the morning and the palliative care project in the afternoon. 5 General notes: The status as a ‘Designated District Hospital of Wanging’ombe’ has made a great difference in the general financial status of Ilembula Hospital. Since July 2014 the agreement, already signed in 2010, has finally been implemented. When fully implemented, the service agreement will cover: - salaries of the staff; the number of staff that are under government payroll is increasing; now 78, in the end will be 265; in addition there are 12 staff members that have been sent and are directly paid by the government/ District Council (including second administrator, which has already remarkably helped in communication with government officials) - provision of drugs (already now the situation is better than before) - provision of food for the patients - ambulance In government plans Ilembula will also become a Zonal Referral Hospital in near future (like 10 other church hospitals). The other nearby hospitals are Njombe Regional Hospital, St Joseph Hospital near Makambako, Mbeya Referral Hospital and Chimala Hospital. ELCT is not providing any financial support to the hospital – yet, is sending auditors every year that have to be paid and accommodated by the hospital The hospital is in the process of installing a quick internet cable (instalment costing TSH 20 million). Two of the three lines can later be sold out, one will serve the hospital. There will be a wireless network in the whole hospital. All wards have computers already (but not necessarily any staff capable of using them). The aim is to computerize both hospital management and patient files (using care2x). There are several insurance schemes in progress. There is a government plan to have community health funds in all regions, but it has not been properly implemented in Ilembula, yet. In community insurance fund the coverage should be more than 50% to be enough. Promotion of community insurance is actively administered. The payment of the insurance is TSH 10000/ year to cover 4 family members (bigger families need to pay more than one insurance fee). The hospital workers are all under national health insurance. About psychiatric services: Present at the meeting of the psychiatric project: Dr-in-Charge Godfrey Ezekiel Mpumilwa, Administrator Bryceson Mbilinyi, Treasurer David Kikungwe, Mental Health Project Coordinator Dr Owden Mwalumuli, Hospital Matron Agnes Lwiva, Acting Principal of Ilembula School of Nursing Anipher Nyunza and the Finnish team, Drs Elina Lind, Tapio Pitkanen, Liisa Laula and Leena Uusitalo There is a dedicated psychiatric team to continue the work even after the project finishes. Hospital has already taken over a lot of the financial responsibility. Until now all outreach clinics have been run as before. Between January and August 2014 (8 months) the total number of patients treated at the outreach clinics was 1674, 58% female, 42% male, 19% under 15 years. However, there are many challenges. Negotiations with the government DMO (District Medical Officer) of Njombe District last year resulted in a promise to include mental health into the basket fund budget, but that did not happen in reality. In the meanwhile, the district has been changed from Njombe to Wanging’ombe. In the newly formed Wanging’ombe district all administration is also new. The priority of the politicians is not health but infrastructure of the new district. 6 Moreover, within health matters the priority is not mental health but rather women, children and elderly people. Nevertheless, negotiations will be continued. Availability of drugs has improved compared to earlier years. The provision of the MSD has been much better than before, and only occasionally some essential drugs have been out of stock. To reduce the costs of the mental health outreach work two suggestions were made: 1) to share transportation with other outreach teams (not regarded really feasible because of different needs of time or different locations of outreach services); 2) to reduce once a month outreach to once in two months, especially those clinics that are far away. That would save both petrol and manpower without really affecting the quality of care remarkably. Between the two meetings we also visited the Nursing School. Ilembula Nursing School was started in 1963. Since 2003 it has offered accredited certificate and diploma level courses. Currently there are 190 students, 80 in the certificate course and 110 in the diploma course. In the certificate level there is an introduction to mental health, and in the diploma level there is a course about management of mental disorders. Teaching about mental health was started about 3 years ago (nationwide), yet, teaching material is still largely missing. Copies of the lecture notes from the Mbeya seminar and the WHO Intervention Guide were therefore given to the acting principal Anipher Nyunza, with the hope that they might be helpful in preparing lectures about mental health. For practical experience nursing students also participate in psychiatric outreach visits. The principal is currently specializing in mental health (a 2-year postgraduate training). Unlike mental health, palliative care is not yet included in the curriculum. About home based care and palliative care (HBC&PC): Present at the meeting of the palliative care project: Palliative Care Coordinator Aida Mtega, Assistant Coordinator, CO Goodyear G. Pangisa, Administrator Bryceson Mbilinyi, Social worker Regina Joseph, Assistant social worker Ziada Madete and the Finnish team, Drs Elina Lind, Tapio Pitkanen and Leena Uusitalo In the meeting with the responsible persons of PC it turned out that it does not seem to be very clear to them, yet, what it means to run the project together and following the set plans. Communication via emails has been a problem, and to some extent it was a problem also face to face. Most likely this is mainly due to the lack of common language. The coordinator of the palliative care, Aida Mtega, is not very fluent in English and of the Finnish group only Dr Tapio Pitkanen is able to speak Swahili. In the meeting, the administrator Bryceson Mbilinyi was translating. The work has largely been continued as before. However, of the 53 volunteers only 23 are left; 23 have swapped to a government paid project, 2 have died and 5 others quitted. After formation of the new Wangin’ombe District, since August 2014, a government initiated AIDS control programme was launched and the regional coordinator nominated. In that programme, volunteers are being paid TSH 35000/month, whereas the HBC volunteers of Ilembula Hospital only receive TSH 20000/month. Thus, many volunteers have shifted. Many of them may still visit the same patients as they used before, though. The new programme is only focusing on HIV/AIDS patients, but majority of the previous patients, too, were suffering from AIDS. It is not yet clear, how the cooperation and coordination of the two programmes will be organized. Aida Mtega will meet with the AIDS control programme coordinator to discuss about it, but that meeting had not yet happened. Those volunteers that are still within the project continue coming to Ilembula once a month. The day when we met only 6 volunteers had come, the rest were to come in the 23rd Oct. 7 About 4000 patients/year are being looked after by the HBC&PC team and volunteers. Those patients that can are requested to pay a little amount (cost sharing). One volunteer can have as many as 126 patients to care for. Aida Mtega with the PC team from the hospital is going for outreach 1-2 times a week. Among the HBC&PC patients there were currently six cancer patients; one had just died over the weekend at the hospital. Till now at least 20 nearby villages are lacking volunteers, so there is a definite need for recruiting and training new volunteers. To recruit new volunteers means that they first need to have a 3-weeks basic training course. On such course one trainer has to be appointed by government (but paid by the hospital/ PC project) to follow the government protocol. Each village needs to have two volunteers, one male and one female. It is possible to have up to 30 participants in the course, thus covering 15 villages (if all are from new villages and not replacing previous volunteers). When asked about curriculum for the training of volunteers Aida Mtega showed 5 different booklets that are being used, most of them produced by the MOHSW. Two were in Swahili, three in English, including for example national guidelines for voluntary HIV/AIDS counselling and testing (2005). Planned study tour to Muheza Hospice in Tanga Region was conducted in September 14th to 16th. There were two participants from the hospital management team (Dr-in-Charge and Treasurer), the rest were from the Palliative Care team (coordinator Aida Mtega, Assistant Coordinator Goodyear Pangisa and PC nurses). Two social workers participated in the meeting. They told about the local government’s initiative to cooperate in a programme targeting to children living with HIV/AIDS. There was a plan to arrange a special gathering of such children and youth in Njombe on the World AIDS Day (1st Dec). The special target group was children and young people between 10-24 years of age, that are neither going to the school nor have an employment. Group of 5-6 was to be selected from Ilembula. In the following financial year (7/20156/2016) 3 million Tanzanian Shillings could be provided for this particular target group with the condition that the 1 million that is available for this year is used in a sensible way. Connection between these children and youth and the HBC&PC did not become very clear. The lack of common language hampered the discussion quite a bit. There was also some discussion about local fund raising. Apart from FCMS project funding, some funds had been received from ELCT Head Office, Arusha. Special collections were also organized in nearby outreach villages; between 2nd and 30th November such collections were planned to be organized in 11 different towns and villages. Lastly we discussed about the plan of Dr Reino Pöyhiä visiting Ilembula again during the first quarter of 2015. The plan was warmly welcomed. Aida Mtega suggested that also the Manager of ELCT Palliative Care Program, Dr Paul Z. Mmbando, should be informed about the dates, and also about our visit at Ilembula. At the time, the decision about further project funding beyond 2014 by the Ministry for Foreign Affairs of Finland had not been received. However, it was clear that all of the funds that were granted for 2014 would not be finished by the end of the year. Therefore, the second visit of Dr Reino Pöyhiä could be financed with remaining funds, although approval of the MFA had to be sought beforehand. 8 21.10. Tuesday Travelling day from Ilembula to Matema (the vehicle of the Palliative Care Team with a driver was hired for the travels again). There was some heavy rain on the way, but luckily that was where the road was paved. We reached Matema just before dark in the evening. 22.10. Wednesday – Matema In the morning we first joined the hospital clinical meeting and morning prayer. The impression of the clinical meeting was that remarkable proportion of all patients were maternal cases, and there had also been several deliveries during the past 24 hours. Total number of inpatients was 53. After a short round in the hospital, we had a meeting about psychiatric work. The meeting was held in the new psychiatric unit/ counselling room that was constructed as part of the project. The rooms were ready, but the unit was still lacking furniture. The Dr-in Charge Christopher Mwasongela was not in Matema during our visit, thus, we did not meet him. One of the two nurses responsible for mental health work, Hezron Ntanjo, was also on leave, but we had met and discussed with him at the seminar in Mbeya. It was not quite clear why only one representative (Hezron Ntanjo) from Matema came to the seminar (and even he a day late). But at least there was a shortage of staff and heavy work load preventing Richard Amasa of leaving the hospital. Present at the meeting: Hospital Secretary Efron Y. Chaula, Acting Dr-in Charge Heinke Schimanowski-Thomsen, Treasurer Fadhili Mwantolwa, Psychiatric nurse Richard Amasa and the Finnish team, Drs Elina Lind, Tapio Pitkanen, Liisa Laula and Leena Uusitalo. In Matema, there were over 8 million Tanzanian Shillings of unused project funds in the beginning of 2014. Thus, the remaining funds of 2200 Euros were not transferred until in the beginning of October. It was highlighted that all project funds have to be used by the end of the year, as the project is ending. Because of funds remaining from previous year, most mental health activities had been continued as before. outreach clinics had been run in all 10 villages (as before), 6 of the villages are reached by land, 4 are along the coast of the Lake Njassa and are reachable by boat (the need for a boat was discussed again). 14 school visits (primary schools) were planned, but only 11 of them conducted; education given was mainly about epilepsy, to raise the awareness and understanding. Lack of funds was the main reason for not visiting all 14 schools. achievements and future prospects: - patients are now aware that they can be treated - yet, most patients cannot afford to pay for their medicines - minimal level of services that can be maintained is to give medication to those patients that come to the hospital and to continue giving mental health education annual mental health budget is about 2.6% of the total budget of the hospital General notes: (Based on discussions at the meeting above and with the hospital secretary Efron Chaula later in the afternoon) 9 financial status of the hospital remains critical there is service agreement with the government covering mother and under-five care and CTC; government is giving 300 million Tanzanian Shillings a year to run these services. However, about double amount would be needed to cover all those costs total number of staff is about 70, 26 of those are under government payroll (increased) to purchase drugs from the MSD, government support is 66 million TSH/ year there is a problem of long delay of getting funds from CHIF (community health insurance fund); no compensation had been received since August 2013 (well over a year) 23.10. Thursday – Itete It took 1 hour 15 minutes in the morning to travel the 33 kilometres from Matema to Itete. Like in Ilembula, in Itete, too, the designation within the government health care system (Busokelo Council Designated Hospital) has already greatly improved the personnel and financial status of the hospital. Present at the meeting: Dr-in-Charge Lee Mwakalimga, Administrator, Rev. Samwel J. Mwansasu, Matron Tumwitikege Nazareth, NOP Stephen Mwakiyolile, Health Secretary (Busokelo) Luciana Makabila, Social worker Imani D. Mbelimbe, Cashier Noel Meshack and the Finnish team, Drs Elina Lind, Tapio Pitkanen, Liisa Laula and Leena Uusitalo. General notes: service agreement/designation as council hospital means that: - the hospital is still owned by ELCT (Konde Diocese), but the work is shared between the Diocese and the government in collaboration - government policies have been adopted in all work - in addition to hospital’s own staff there are staff members seconded by government - more than 10 of the former staff have been transferred under government payroll - total number of staff including those seconded by government is 135 (need is up to 214, if all posts were filled) - Dr Lee is the only medical doctor; in addition there are 5 clinical officers (3 seconded by Busokelo District/Council) - of the nurses 9 are seconded by the District Council - hospital is eligible to get all medicines from government; both MSD and private pharmacies (through basket fund) - exempted groups include: pregnant woman, children under five, elderly and psychiatric patients with all the changes hospital is still in transition period About psychiatric services: mental health is now included in the budget of the basket fund NOP Stephen Mwakiyolile has been named as the coordinator of mental health in Busokelo District/Council (another psychiatric nurse Simon Mwaitalako has similarly been nominated as coordinator of Home Based Care) some outreach clinics (6 dispensaries in Busokelo) are now also getting medicines from MSD after the project funding ceases, there will be a problem in running the outreach clinics (lack of funds for fuel and allowances) 10 the minimum level of services that can be sustained will be seeing patients at the hospital OPD and home visiting to nearby patients of the total hospital budget, the budget of psychiatric department is about 4% in 2014 Overall impression of Itete Hospital was that there was a lot of new hope for future and enthusiasm to develop the services. Collaboration between the former hospital staff and staff seconded by the District/Council seemed smooth. When asked staff members told that they were happy with the situation now. In the evening we had been invited for dinner at Stephen Mwakiyolile and her newly married wife Tumbe. The hospital treasurer, Yolam Mates Lamsi, was away and only returned after the meeting. We met him briefly the following day before leaving Itete. A donation of 350 000 TSH was made to be used for the audit costs of the psychiatric project in 2015. 24.10. Friday Travelling day; from Itete to Mbeya, Mbeya to Dar es Salaam and leaving for Finland. In the morning we participated the morning meeting and prayer of Itete Hospital before leaving for Mbeya. As agreed before, we had lunch at Mbeya Hotel with Dr Lawala. A week after completing the seminar Dr Lawala was happy with the outcome and cooperation – and so were we. Dr Lawala gave detailed financial report of the seminar with copies of all vouchers as was the agreement. After all costs had been covered there was an excess of 171 440 TSH, which he returned in cash. The FastJet flight from Mbeya/Songwe took us to Dar es Salaam Julius Nyerere International Airport. Before late evening departure for Finland (via Amsterdam) we had dinner together with Dr Manento Ernest Mtango and his wife Mary Ernest Mtango at the airport restaurant. Dr Manento Ernest Mtango’s post graduate studies (Master’s in Obstetrics and Gynaecology) have been supported by a group of Finnish donors through FCMS scholarship programme. The studies were almost finished, and took about 4 years. He and his wife have been invited to visit Finland in March/April 2015. Night flight to Amsterdam followed by flight to Helsinki-Vantaa; arrived at 1:20 pm. Farewell to travelling companions. Summary and conclusions It was encouraging to see that mental health work was still going on in all partner hospitals despite the remarkable reduction in project funding in 2014. In Mchukwi all outreach clinics had been discontinued, though, and patients were only seen at the hospital, with the consequence of about 2/3 drop in patient numbers (by October). All project funding in 2014 had been channelled in trying to hand over the village level psychiatric care to the government health posts and dispensaries in former outreach sites. If successful, this will ensure sustainability and continuous availability of primary level mental health care integrated in the existing government health care structures. The level of the quality of care will initially deteriorate, but if supervision can be provided the situation may gradually improve again. The seminar for health post workers had to be postponed till November. It was agreed that FCMS (with or without funds 11 from MFA) will fund at least one follow up/ mentoring visit by Mchukwi Hospital psychiatric nurses to all health posts attending the seminar. If regarded useful, this kind of follow up/ mentoring visits could be supported with FCMS’s own funding in future, too. Alternatively, a specific project to support handing over period could be planned and applied. In Ilembula and Itete the designation of the hospitals as district/council hospitals had remarkably strengthened their financial situation, as the government health authorities were taking increasing responsibility of funding. Both hospitals were still in transition period; positive steps were already taken, but the agreements with the government had not yet fully materialized. In Ilembula the hospital had already taken over funding of ongoing psychiatric outreach work (after project funding had finished) even though that had not been included in the hospital budget. In Itete, psychiatric unit was already included in the general budget, as well as in the district/council basket fund budget. The long term coordinator of the psychiatric team in Itete had also been appointed the coordinator of mental health in the new Busokelo District/Council. In Matema the reduction of project funding had been somewhat minor, due to funds carried over from the previous year. The general financial situation of the hospital remains critical, thus, despite dedicated staff members running the psychiatric services, future seems very challenging. The construction of the psychiatric unit had been completed, but the furniture was still missing. In all four hospitals worries were expressed about future funding. Yet, all shared the view that during the project years at least awareness about mental disorders within the communities has greatly increased; patients and their relatives now know that treatment is available, and many false beliefs have become less strong. The cooperation in arranging the seminar with Mbeya Referral Hospital Psychiatric Unit/ Dr Paul Lawala was also very encouraging, both beforehand and during the seminar. Arrangements of the seminar were excellent and also financial matters were dealt proficiently and trustworthy by the hospital administration. The option of continuing collaboration in a new project, largely focusing in promoting mental health through advocacy, education and strengthening existing services, will be seriously considered. Application to MFA of Finland for a new project can be submitted at earliest in May 2015. If accepted, the new project could start in 2016. The palliative care project at Ilembula has only been running since the beginning of 2014, although the work itself has been going on much longer. There seemed to be some confusion about following the plans set for the project, as well as about the meaning of partnership with FCMS in the project in general. Communication has not been easy by emails, and was a bit complicated even face to face, presumably largely due to lack of common language. Another trip of Dr Reino Pöyhiä to Ilembula in early 2015 was agreed mutually important, both for training purposes and for clarifying and strengthening the idea of true partnership in aiming at improving (not only funding) palliative care services at Ilembula. Prepared by: Elina Lind Attachments: 1) Report of the Seminar in Mbeya by Dr Paul Lawala 2) TIME TABLE FOR MENTAL HEALTH SEMINAR AT MBEYA REFERRAL HOSPITAL, 15TH TO 17TH OCTOBER 2014 (plan and actual combined) 3) Group photo of the seminar participants 12 Attachment 1. REPORT: MENTAL HEALTH SEMINAR FOR PRIMARY HEALTH PROVIDERS 15th TO 17th OCTOBER 2014. INTRODUCTION The service and friendship link has been established between Finish Christian Medical Society (FCMS), Ministry for Foreign Affairs of Finland and the Department of Psychiatry and Mental Health in Mbeya Referral Hospital. This link was made possible by some members of the FCMS making a visit to Mbeya Referral Hospital in 2013. The three parties facilitated to conduct 3 days mental health seminar in Mbeya. The similar programs have run in collaboration with the church Hospital for the past 13 years until 2013. This is the first time the seminar to be organized by Mbeya Referral Hospital. The seminar was successfully conducted by involving 18 mental health staff from Mbeya and Njombe health facilities. Participants came from Mbeya Regional Hospital, Mbeya Referral Hospital, Njombe Town Hospital, Ileje District Hospital, Rungwe District Hospital, Kyela District Hospital, Mbozi District Hospital, Ilembula Hospital, Bulongwa Hospital, Itete Hospital, Matema Hospital, and Mbarali District Hospital. The seminar coordinator went on by giving training protocols and logistics after introducing everyone to each other. Then facilitators guided the participants to select the leaders, secretariat with the ground rules to be followed during the training. Names of the participants and their respective facilities. S/no 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. 15. 16. 17. 18. NAME OF THE PARTICIPANT DR. TRIOALA NYENZA DASHUD MWAKABANJE DAINA IFWANI JOAKIM LUOGA EXAUD MWEMUTSI HURUMA DOTO EVETA MCHOMBA GEOFREY ZOMBE EMERENSIANA MTEGA DEBORA DIKOKO SOFIA MFUNGATI DR O. MWALUMULI JOHN MATARA ROSE PELES SIMON MWAITALAKO STEVEN MWAKYOLILE HEZRON NTANJO DR. FRANSIS BENEDICT TITLE MED. OFFICER DNO NO RN RN RN RN RN RN RN NO AMO RN RN RN RN RN PSYCHIATRIST HEALTH FACILITY MBEYA REF. HOSPT ILEJE DH MBEYA REF HOSPT MBOZI DH MBEYA REF. HOSPT. RUNGWE DH MBARALI DH KYELA DH MBEYA DC MBEYAREG HOSPT ILEMBULA HOSPT ILEMBULA HOSPT BULONGWA HOSPT. BULONGWA HOSPT ITETE HOSPITAL ITETE HOSPITAL MATEMA HOSPTAL NJOMBE HOSPITAL 13 SEMINAR METHODS Power point presentation slides Small group discussions Individual presentations, pre and end of the day tests Visiting mental health services at Mbeya referral hospital BUDGET ESTIMATIONS The budged estimation was 8,150,000.00. The money transfer from FCMS account was completed on 26th September 2014 amounted 7,973,840.00. As summarized in the table below SUMMARY OF BUDGET ESTIMATIONS Items Unit cost (TZS) Total (TZS) 1. Venue 70,000 210,000 Participants 80,000 4,800,000 Facilitators 80,000 960,000 20,000 280,000 1,000,000 1,000,000 50,000 150,000 10,000 Total 750,000 8,150,000/= 2. 3. 4. Tickets 5. Training materials 6. Car hire 7. Food & drinks 14 SUMMARY OF ACTUAL EXPENDITURE S/No 1. 2. 3. 4. 5. 6. 7. 8. 9. ITEM RECEIPTS Stationery Venue Food Participants Tickets refund Facilitators Supporting staff Report writing Total expenditure Balance AMOUNT 7,973,840.00 991,800.00 210,000.00 756,600.00 3,927,500.00 234,000.00 1,200,000.00 97,500.00 385,000.00 7,802,400.00 171,440.00 15 FUTURE PLANS FOR MENTAL HEALTH PROGRAMS The department of Psychiatry and Mental Health has planned to conduct the following programs which will in short and long terms expected to significantly improve services in primary mental health. The resources to accomplish goals of these programs are presumed to be internally and externally supported. The chance for internal support is still lacking. For this reason external support if made available will be highly appreciated. Among the following listed programs, any external support to implement them will be acknowledged. Service area Recommended program Current status Supervision Mentorship and supportive supervision Outreach clinics Not done Outpatient clinics Estimated cost per year 7,000,000/= Not done 5,000,000/= Mental health promotion Psychiatry and mental health skills for service providers Psychiatry & Mental health knowledge and skills for primary care clinicians Public exhibitions Research Rehab services Primary and secondary school education programs Annual seminars Teaching of primary care clinicians (Mbeya AMOs School) Nane nane public exhibition Conducting collaborative research with Universities in Finland Development of Uyole rehab village Prepared by: Dr. Paul S. Lawala (MD, MMED) Psychiatry and Mental Health Specialist Mbeya Referral Hospital P O BOX 419, TEL: +255716 388 124 / +255755866363 MBEYA TANZANIA Attachment 2. Not done 10,000,000/= Have been going on for some years now Thanks for October 2014 seminar Not existing 25,000,000/= Done periodically 1,000,000/= Planned to select areas of interest, drafting a proposal Very poor level of development to suit rehab services 16 TIME TABLE FOR MENTAL HEALTH SEMINAR AT MBEYA REFERRAL HOSPITAL, 15TH TO 17TH OCTOBER 2014 DAY 1, 15TH OCTOBER 2014 TIME 8.30 – 9.00 am 9:00-9:50* 9.00-9.15 am 9:50-10:00 9.15 - 9.50 am 10:00-11:00 11:00-11:30 11:00-11:15 9.50- 10.20 am 11:15-12:00 EVENT Official opening, introduction to each other RESPONSIBLE PERSON All Day 1 Pretest Participants Finnish colleagues experience in conducting mental health services in Tanzania Tea break Dr Tapio Pitkänen Mental health services in Tanzania, strengths, challenges and opportunities. Dr Paul Lawala 10.50-11.30 12:05-1:10 Community perspectives of mental illness in TZ and their effects to treatment of mental disorders Ms Liness Ndelwa MSc, Clinical Psychology 11.30-12.30 pm 1:10-1:40, cont. 2:15-2:50 1.10-2.00 pm 1:40-2:15 12.30-1.10 pm 2:50-3:40 Participants experiences in managing mentally ill patients, case scenarios. Their views on how to improve services at primary levels Lunch break Participants Introduction to mental illness, assessment of mentally ill patients. Common and severe mental disorders Treatment of mental disorders – general considerations Community involvement in care of mentally ill patients in Tanzania End of day 1 test Dr Francis Benedict End of Day one All 2.00-2.30 pm 3:40-4:40 2.30-3.00 pm 4:40-5:40 3.00-3.30 pm 5:40-6:00 3.30-4.00 pm 6:00 *Actual timetable in italics All All Dr Francis Benedict Ms Liness Ndelwa Participants 17 DAY 2, 16TH OCTOBER 2014 TIME 8.30 – 9.00 am 9.00-10.30 am EVENT Recap for day 1 Mood disorders 1. Depression: Identifying symptoms and management interventions Tea break 10.30-11.00 am 10:10-10:50 11.00- 12.00 pm Mood disorders 2. Bipolar disorder 10:50-12.00 12.00-12.40 pm Psychotic disorders 12:00-1:00 1:00-1:15 Visit of the Executive Director of Mbeya Referral Hospital 12.40-1.30 Seizure disorders 1:20-2:30 1.30 -2.00 pm Lunch break 2:30-3:10 3:10-3:30 Mental development in childhood and adolescence 2.00-2.50 pm Developmental disorders 3:30 – 4:30 2.50-3.20 End of day 2 test 4:30-4:40 Visit to Mbeya Referral Hospital, Psychiatric Unit RESPONSIBLE PERSON Dr Paul Lawala and Ms Liness Ndelwa All Ms Liness Ndelwa Dr Liisa Laula Dr. Mpoki M. Ulisubisya, MD, MMED, MBA Dr Paul Lawala All Dr Liisa Laula Dr Francis Benedict Participants All DAY 3, 17th OCTOBER 2014 8.30- 9.00 am 9.00- 10.30 am 10.30-11.00 am 11.30-1.30 pm 10:45-11:40 11.20-12.00 pm 11:40-1:00 12.00- 12.40 pm 1:10-1:40 2:05-2:40 12.40-1.10 pm 1:40-2:05 1.10-1.40 pm 2:40-3:05 1.40- 1.50 pm 3:05-3:15 1.50-2.00 pm 3:15-3:30 Recap for day 2 Behavioral disorders Tea break Dementia Participants Dr Francis Benedict Substance related disorders Dr Francis Benedict Somatoform disorders Ms Liness Ndelwa Dr Paul Lawala Lunch break Future plans for mental health programs MRH End of day 3 test Dr Paul Lawala Closure: Remarks All Participants 18 Attachment 3. Participants of the Mental Health Seminar in Mbey 15th – 17th October, 2014 (Photo E. Lind)