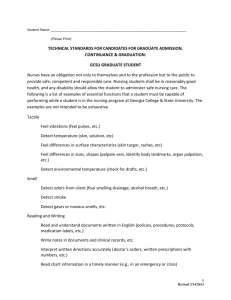
associate degree nursing program
advertisement

REGISTERED NURSING NURR 201 10 Credits Fall 2009 1 Revised 2/9/2016 TABLE OF CONTENTS SECTION A PAGE NO. Course Overview……………………………………………………………….. 4 Topical Outline………………………………………………………………….. 11 Calendar…………………………………………………………………………. 19 Course Objectives……………………………………………………………… 24 Teaching/Learning Lab Objectives…………………………………………… 37 Clinical Objectives……………………………………………………………… 40 SECTION B--ASSIGNMENTS List of Assignments……………………………………………………………. Case Studies…………………………………………………………………… Care Plan/Concept Map Template………………………………………….. Care Plan Grading Rubric……………………………………………………. Teaching Plan Template …………………………………………………….. Teaching Plan Grading Rubric ……………………………………………… Portfolio………………………………………………………………………… Record of Professional Development………………………………………. 43 44 45 56 60 64 70 71 SECTION C—CLINICAL Guidelines for Clinical Activity……………………………………………………. Objectives for Clinical Spinouts…………………………………………………. Criteria for Clinical Journaling……………………………………………………….. Clinical Tally…………………………………………………………. ADN Program Agreement Form………………………………………… Health Insurance Form ………………………………………………… Vehicle Insurance Form…………………………………………………………. Clinical Confidentiality Contract ………………………………….. Dialysis Confidentiality Contract Alcohol/Drug Policy Form Clinical Evaluation Clarification…………………………………………………. Clinical Evaluation Tool…………………………………………………………... 75 76 80 82 86 87 88 89 90 91 92 93 2 Revised 2/9/2016 SECTION A 3 Revised 2/9/2016 ASSOCIATE DEGREE NURSING PROGRAM MISSION STATEMENT “The Associate Degree Nursing Program, being an integral unit of the College of Southern Idaho, educates graduates from diverse populations who: demonstrates knowledge and caring through the nursing process to respond to the holistic needs of individuals in a variety of settings and interacts professionally with patients, families, and coworkers within the community. The graduate promotes optimum health in a costeffective manner, as part of a multidisciplinary workforce, and recognizes that learning is a lifelong endeavor.” COURSE TITLE: ADVANCED NURSING INTERVENTION COURSE DESCRIPTION: NURR 201 Advanced Nursing Intervention (Fall/Spring) 10 credit hours (5Theory/5 Clinical) The focus of this course is the nursing care of patients with medical/surgical health deviations; with emphasis on pathophysiology. This course includes theory, clinical and teaching/learning laboratories. Therapeutic nutrition, pharmacology, and medical terminology are integrated throughout the course Prerequisites: NURR 103, all science courses. Corequisites: MATH 143 or 253, humanities, or other required general education courses. LEVEL OBJECTIVES/OUTCOMES UPON SUCCESSFUL COMPLETION OF NURR 201 THE LEARNER WILL BE ABLE TO: I. PROFESSIONAL BEHAVIORS Demonstrate with supervision, the role of a professional nurse as a member of the healthcare team including legal/ethical responsibilities, accountability, and identification of evidence-based nursing trends. II. III. COMMUNICATION Demonstrate with supervision, beginning skills in the use of verbal and nonverbal communication fostering caring relationships with individuals, families, and members of the health-care team. Demonstrate computer knowledge and skill through the utilization of the internet. ASSESSMENT Demonstrate application of the principles of assessment through collection, analysis, and synthesis of relevant data to meet the basic needs of individuals. 4 Revised 2/9/2016 IV. V. CLINICAL DECISION MAKING Demonstrate application of the nursing process, critical thinking skills, and technology to meet the increasingly complex needs of the individual. CARING INTERVENTIONS Develop and sustains trusting relationships in a diverse population. VI. TEACHING AND LEARNING Apply the steps of the teaching-learning process to patients with more complex needs. VII. COLLABORATION Distinguish between members of the healthcare team and their contributions to promote decisions in client care. VIII. MANAGING CARE Demonstrate the principles of safe, cost-effective, evidence-based, patient-centered nursing care. REQUIRED FOR NURR 201 Lab Kit Clean gloves Blank DVD with recording capability I-Clicker NURR 201 Syllabus The following textbooks: Brooks, M. L. & Brooks, D. L. (2004). Basic medical language (2nd ed.). St. Louis, MO: Mosby. Castillo, S. L. & Werner-McCullough, M. (2002). Calculating drug dosages: An interactive approach to learning nursing math. Philadelphia, PA: F.A. Davis. Evolve select. (2007). St. Louis, MO: Elsevier. Grodner, M., Long, S., & Walkingshaw, B. C. (2007). Foundations and clinical applications of nutrition: A nursing approach (3rd ed.). St. Louis, MO: Mosby. Hockenberry, M. J., & Wilson, D. (2009). Wong’s essentials of pediatric nursing (8th ed.). St. Louis, MO: Mosby. Hockenberry, M. J., & Wilson, D. (2009). Study guide to accompany Wong’s essentials of pediatric nursing (8th ed.). St. Louis, MO: Mosby. Lewis, S. M., Heitkemper, M. M., Dirksen, S. R., O’Brien, P. G., & Bucher, L. (2007). Medical-surgical nursing: Assessment and management of clinical problems (7th ed.). St. Louis, MO: Mosby. 5 Revised 2/9/2016 Lilley, L. L., Harrington, S., & Snyder, J. S. (2007). Pharmacology and the nursing process (5th ed.). St. Louis, MO: Mosby. Lilley, L. L., Harrington, S., & Snyder, J. S. (2007). Study guide for pharmacology and the nursing process (5th ed.). St. Louis, MO: Mosby. Mosby’s dictionary of medicine, nursing, and health professions (7th ed.). (2006). St. Louis, MO: Mosby. Mosby’s comprehensive review of NCLEX-RN (19th ed.). St. Louis, MO: Mosby. Mosby’s nursing drug reference (22nd Ed.). (2009) St. Louis, MO: Mosby. O’Brien, P. G., Dirksen, S. R., Lewis, S. L., Heitkemper, M. M., & Bucher, L. (2007). Clinical companion to medical-surgical nursing (7th ed.). St. Louis, MO: Mosby. O’Brien, P. G., Lewis, S. M., Heitkemper, M. M., & Dirksen, S. R., & Bucher, L. (2007). Study guide for medical-surgical nursing (7th ed.). St. Louis, MO: Mosby. Pagana, K. D. & Pagana, T. J. (2007). Mosby’s diagnostic and laboratory test reference (8th ed.). St. Louis, MO: Mosby. Potter, P. A. & Perry, A. G. (2009). Fundamentals of nursing (7th ed.). St. Louis, MO: Mosby. Preusser, B. A. (2009). Winningham and Preusser’s critical thinking in medical-surgical settings (4th ed.). St. Louis, MO: Mosby. Publication manual of the American psychological association (5th ed.). (2002). Washington DC: American Psychological Association. Sole, M. L., Klein, D. G., & Moseley, M. J. (2009). Introduction to critical care nursing (5th ed.). St. Louis, MO: Elsevier. Yoder-Wise, P. S. (2007). Leading and managing in nursing (4th ed.). St. Louis, MO: Mosby. Zerwekh, J., Claborn, J. C., & Gaglione, T. (2005). Mosby’s pharmacology note cards: Visual, mnemonic, and memory aids for nurses. St. Louis, MO: Elsevier. CREDIT/HOURS ALLOCATION Ten (10) hours credit: Theory, clinical experience, experience laboratory class, and practice labs are included in the ten credits. Lab credits are at a ratio of 3 hours of lab/week per one credit 5 credits = 5 theory hours/week 5 lab credits = 14 clinical hours/week and 2 hour teaching/learning lab class hours x 7 weeks during the semester 6 Revised 2/9/2016 The clinical learning experiences will be obtained in various settings: Campus laboratory, various community facilities, and out-patient settings. METHOD OF INSTRUCTION Lecture, discussion, small group work, role playing, games, videotaping, selected computer assisted instruction, power point, reference readings, written assignments workbooks, study guides, simulation, films and clinical instruction, personal journals, poster presentations, and computer assignments. ACADEMIC POLICIES Policies regarding: attendance, plagiarism, required assignments, lateness, uniform dress, and others are identified in the Associate Degree Nursing Program Student Handbook. METHOD OF EVALUATION AND COMPUTATION OF FINAL GRADE The learning for each semester encompasses a variety of assignments designed to develop a sound knowledge/performance foundation for the student. Computation of a final grade for a semester is a multi-step process. Step One requires that the student achieve a minimum of a 70.0% average on theory tests. Step Two averages in quizzes with theory tests; and this must once again average 70.0% or higher. Step Three requires that the student achieve a 70.0% or higher in all written work and an "S" in all clinical performance behaviors (see clinical evaluation form). Step Four requires that the student achieve a minimum of 90.0% on a Dosage Calculation Exam (the student is allowed three attempts at passing a dosage calculation exam during the semester following remediation). Step Five is the final calculation of the semester grade. THEORY STEP ONE Six Exams 260 points total Comprehensive Final exam 75 points 70% or higher average ****STUDENTS MAY MAKE AN APPOINTMENT TO VIEW THEIR EXAMS WITH THEIR CLINICAL INSTRUCTOR. EACH UNIT EXAM CAN ONLY BE VIEWED UNTIL THE NEXT UNIT EXAM. STUDENTS WILL NOT BE ALLOWED TO VIEW EXAMS BEFORE THE FINAL STEP TWO Having achieved a 70% or higher average on all tests, the final theory grade is based on: Theory tests average Quiz average: 120 points 90 % 10 % 7 Revised 2/9/2016 STEP THREE Written Work Journaling Portfolio Clinical Application T & L Labs 70% or higher average S S S S Having achieved a 70% or higher average on all written work, and all "satisfactory" in lab and clinical performance and assignments, the final clinical grade is computed. Please note that Pass/Fail assignments not submitted on time can result in an ‘Unsatisfactory’ grade and the student may not be successful in completing the semester. STEP FOUR The student must successfully complete a dosage calculation exam at a 90% level or higher. The student will be afforded three (3) attempts to accomplish the 90% level and a remediation process will be put in place after each failed attempt. Should the student not pass the dosage calculations exam at a 90% level or higher after remediation and completion of the third exam, Step Five of the computation of the final semester grade will not be completed and the student will not be successful in completing the semester. STEP FIVE Having achieved the above, step five of this process for computation of the final grade is based on: THEORY 70% } = FINAL GRADE CLINICAL 30% **At any step in the grading process, 69.5% to 69.9% will not be rounded to a 70% STEP SIX After a student has achieved a 70% exam grade average, if the student passes the proctored exam at the benchmark, one percentage point per ATI exam will be added to the students’ exam grade average. CLINICAL EVALUATION Evaluations of the student are given at the end of each clinical rotation and at other times as deemed necessary. (See Clinical Evaluation Sheet, Section D). Students will complete a self evaluation and clinical instructor will complete a student evaluation to be discussed during an evaluation meeting, scheduled individually at the end of each clinical rotation. The student will present the Portfolio, including printed journal entries and the Record of Professional Development (Section C) and Clinical Experience Tally (Section D) during the evaluation as well. A Satisfactory or Unsatisfactory clinical evaluation is based on demonstration of skills and applied knowledge. Any student receiving an ‘Unsatisfactory’ final clinical evaluation grade at the end of the second clinical rotation will receive a failing grade for the course. Separate credit is not given for clinical. All written work required for clinical must average 70% for the student to 8 Revised 2/9/2016 progress. Exception: The Intermediate Nursing Interventions Course (NURR 103) is one individual course with two separate clinical components: Medical-Surgical and Mental Health. A student who does not achieve a satisfactory clinical evaluation from either one or both of these clinical components will receive a failing grade for the course. OTHER EVALUATIONS Evaluations for guest speakers, clinical sites, and clinical spin outs are required for each course and can be found under the evaluation tab on individual course blackboard sites. COURSE EVALUATION Course evaluations and instructor evaluations are posted on Blackboard and each student is encouraged to evaluate each instructor as well as the course for future modifications and improvements. COMPUTER USAGE Computers are available for students in the computers labs (Aspen 144 and Library). Internet access is available to students in the library, the computer lab, and the Outreach Centers. All students are required to maintain a CSI e-mail address. Since email is the primary source of written communication with students, all registered CSI students get a college email account. Student e-mail addresses have the following format: <address>@eaglemail.csi.edu where <address> is a name selected by the student as a part of activating his/her account. Students activate their accounts and check their CSI e-mail online at http://eaglemail.csi.edu. Instructors and various offices send messages to these student accounts. Students must check their CSI email accounts regularly to avoid missing important messages and deadlines. At the beginning of each semester free training sessions are offered to students who need help in using their accounts. LIBRARY USAGE The college library contains many recent acquisitions both in book form and current subscriptions to professional journals. This resource is for student utilization for study or when writing required papers. Books and articles in great demand are placed on reserve "for library use only" to make them available to a greater number of students. DISABILITIES: Any student with a documented disability may be eligible for related accommodations. To determine eligibility and secure services, students should contact the coordinator of Disability Services at first opportunity after registration for a class. Student Disability Services is located on the second floor of the Taylor Building on the Twin Falls Campus. 208-732-6260 (voice) or 209734-9929 (TTY) 9 Revised 2/9/2016 ATI EXAMS Total Testing Program The ADN program utilizes a total testing program from Assessment Technologies Institute (ATI), Inc. to help the student and the program evaluate the effectiveness with which they are meeting the objectives of the educational program. The cost of these exams is the student's responsibility and payable with tuition each semester. These required exams must be completed by the deadline dates listed in course syllabi. The student will take the proctored exam and attempt to pass at the benchmark proficiency level. If the Level II benchmark is not met, a written remediation plan must be submitted to the course coordinator and completed before another exam is administered. Attempts to pass exams at the benchmark must be taken at least 24 hrs. apart. The benchmark is 90% for the nonproctored exams. Failure to complete the ATI test requirements specified in each individual course calendar will result in a failing grade for the course. Various exams, including a Virtual ATI NCLEX success package, are part of the total testing program. 10 Revised 2/9/2016 TOPICAL OUTLINE AND CALENDAR NURR 201 Advanced Nursing Intervention Class 1 Focus: Fluid and Electrolyte and Acid Base Review Fluid and electrolyte imbalances Acid base imbalances Readings: Lewis et al., 2007, Chapter 17 with associated study guide Adams & Koch, Chapter 42 Assignment: Fluid & Electrolyte practice in assignment section of Blackboard Objectives: A-B Instructor: Laurie Anne Silva, RN BS Class 2 Focus: Readings: Objectives: Instructor: Class 3 Focus: Readings: Objectives: Instructor: Class 4 Focus Readings: Objectives: Instructor: Genitourinary Genitourinary disorders in the adult and pediatric patient Lewis, 2007 Chapters 45 & 46 with associated study guides Associated study guide for Lewis Hockenberry, Chapter 27 Adams & Koch, Chapter 51 A-K Gay Bondelid, RN MS Renal Renal disorders; acute and chronic renal failure, ESRD Lewis, 2007 Chapter 47 with associated study guide Sole, Chapter 14 Grodner Chapter 21 Murphy study guide for Chapter 27 (Hockenberry) Adams & Koch, Chapter 35 A-D Gay Bondelid, RN MS Guest speaker(s) from DaVita Dialysis Center Burns Burns; care of the adult and pediatric burn patient Lewis, 2007 Chapter 25 with associated study guide Hockenberry, Chapter 30: pp. 1091-1104 Grodner, 2007 pp. 351-355 Sole, Chapter 20 ATI Adult medical-surgical nursing, pp. 1085-1095 A-F Laurie Anne Silva, RN BS EXAM #1 11 Revised 2/9/2016 Class 5 Focus: Readings: Objectives: Instructor: Class 6 Focus: Readings: Objectives: Instructor: Class 7 Focus: Readings: Objectives: Instructor: Class 8 Focus: Readings: Objectives: Instructor: Class 9 Focus: Readings: Objectives: Video: Instructor: Respiratory System Structure and function of the respiratory system, pathophysiology, assessment of the respiratory system, diagnostic studies of the respiratory system Lewis et al., 2007, Chapter 26 with associated study guide ATI Nursing care of children, pp. 139-152 ATI Adult medical-surgical nursing, pp.29-79 5 A, B Laurie Anne Silva, RN BS Respiratory System Upper respiratory problems, pulmonary function volumes and capacities, pathophysiology, nursing care of patients with upper respiratory conditions, arterial blood gases Lewis et al., 2007, Chapter 27 with associated study guide Sole et al., 2009, pp. 173-193 ATI Adult medical-surgical nursing, pp. 22-28 and pp. 172-180. 5 C-F Laurie Anne Silva, RN BS Respiratory System Lower Respiratory problems Lewis et al., 2007, Chapter 28 with associated study guide ATI Adult medical-surgical nursing, pp. 92-100 5G Laurie Anne Silva, RN BS Respiratory System Obstructive pulmonary diseases Lewis et al., 2007, Chapters 28-29 with associated study guide Grodner et al., 2007, Chapter 20, pp. 460-465 ATI Adult medical-surgical nursing, pp. 101-160 5G Laurie Anne Silva, RN BS Respiratory System Respiratory pharmacology, pediatric respiratory disorders and related collaborative and nursing management Lilley et al., 2007, Chapters 35-36, and 40 with associated study guides OR Adams & Koch, 2010, Chapters 73-74 Hockenberry Chapter 23 with associated study guide ATI Nursing care of children, pp. 153-199 5 H-K Respiratory agents Laurie Anne Silva, RN BS 12 Revised 2/9/2016 Class 10 Focus: Hematologic/Lymphatic System Pathophysiology and Assessment of Hematologic and Lymphatic Systems of Adult and Children Including Diagnostic Studies Reading: Lewis, Ch. 30 Sole (2005) Ch. 15 or Sole (2009) Ch. 16 Objectives: 6A, B, C, D Instructor: Darcie Koffer, BS, RN Study Guides: O’Brien/Lewis Study Guide; Ch. 30 Class 11 Focus: Hematologic/Lymphatic System Nursing Role in the Care of Adults and Children with Hematologic and Lymphatic Disorders Reading: In class handout on Diagnostic Tests Lewis, Ch 31 Sole (2005) Ch. 15 or Sole (2009) Ch. 16 Hockenberry, Ch. 26 Grodner, Ch. 7, pp. 137-140; Ch. 8 pp. 174-178 Objectives: 6E Instructor: Darcie Koffer, BS, RN Study Guides: O’Brien/Lewis Study Guide; Ch. 31 Murphy Study Guide; Associated Sections Only Class 12 Focus: Hematologic/Lymphatic System Nursing Role in Pharmacologic and Blood Component Therapy in the Care of Adults and Children with Hematologic and Lymphatic Disorders. Reading: Lewis, Ch. 31 Sole (2005) Ch. 15 or Sole (2009) Ch. 16 Hockenberry (2005) Ch. 26, pp. 978-980 or Hockenberry (2009) pp. 943-946 Lilley, Ch. 49, pp. 767-769, Ch. 54, pp. 832-833, pp. 836-838, and Ch. 56 Grodner, Ch. 7, pp. 137-140, Ch. 8 pp. 174-177 Objectives: 6F, G Instructor: Darcie Koffer, BS, RN Study Guides: O’Brien/Lewis Study Guide, Ch. 31 Murphy Study Guide, Associated Sections Only Lilley Study Guide, Associated Sections Only EXAM #2 Class 13 Focus: Reading; Objectives: Instructor: Cardiovascular System Anatomy, pathophysiology, and assessment of the cardiovascular system in adults and children Lewis, 2007 Chapter 32 with associated study guide Sole, 2005, Chapter 11, pp. 291-296 7 A, B, C Tammy Becker, MS RN 13 Revised 2/9/2016 Class 14 Focus: Reading: Objectives: Instructor: Class 15 Focus: Reading: Objectives: Instructor: Class 16 Focus: Reading: Objectives: Instructor: Class 17 Focus: Reading: Objectives: Instructor: Class 18 Focus: Cardiovascular System Clinical manifestations and nursing management of adults and children with hypertension; prevention and pharmacological management Lewis; Chapter 33 with associated study guide Grodner; Chapter 20, pp. 447-460 Lilley; Chapter 24, 25 with associated study guides OR Adams & Koch, 2010, Chapters 31-33 ATI Adult medical-surgical nursing, pp. 263-273 7 D-E Tammy Becker, MS RN Cardiovascular System Pathophysiology, clinical manifestations, diagnostic testing and nursing care of adults with coronary artery disease, angina, and acute myocardial infarction; pharmacological management. Lewis; Chapter 34 with associated study guide Grodner; Chapter 20, pp. 447-460 Lilley; Chapter 21. 23, and 28 with associated study guides OR Adams & Koch, Chapters 36-37 Sole, 2005 Chapter 11, pp. 296-340 ATI Adult medical-surgical nursing, pp. 209-232 and 330-340 7 F-J Tammy Becker, MS RN Cardiovascular System Pathophysiology, clinical manifestations, and nursing care of adults and children with heart failure; pharmacological management. Lewis; Chapter 35 with associated study guide Lilley; Chapter 25 with associated study guide OR Adams & Koch, 2010, Ch. 38 Grodner; Chapter 20, pp. 459-460 ATI Adult medical-surgical nursing, pp. 306-320 7K Tammy Becker, MS RN Cardiovascular system Dysrhythmias, pathophysiology, clinical manifestations, nursing interventions of adults and children experiencing dysrhythmias; antidysrhythmic pharmacology Lewis, 2007, Chapter 36 with associated study guide Lilley, 2007, Chapter 22 OR Adams & Koch, 2010, Chapter 39 ATI Adult medical-surgical nursing, pp. 181-188 and pp. 199-208 7L Tammy Becker, MS RN Cardiovascular System Pathophysiology, clinical manifestations, and nursing care of adults and children with inflammatory and structural heart disorders 14 Revised 2/9/2016 Reading: Objectives: Instructor: Class 19 Focus: Reading: Objectives: Instructor: Lewis, 2007, Chapter 37 with associated study guide Sole, 2005 Chapter 11, pp. 340-348 ATI Adult medical-surgical nursing, pp. 321-329 7M Tammy Becker, MS RN Cardiovascular System Vascular disorders. Anticoagulation therapy. Pathophysiology, clinical manifestations, diagnostic testing and nursing care of children after cardiac catheterization and with congenital heart defects Lewis, 2007, Chapter 38 with associated study guide Hockenberry, 2009, Chapter 7, pp. 143-147 Hockenberry, 2009, Chapter 25, pp. 861-909 with associated study guide Lilley, 2007, Chapter 27 OR Adams & Koch, 2010, Chapter 40 ATI Nursing care of children, pp. 200-214 ATI Adult medical-surgical nursing, pp. 274-305 7 N-O Tammy Becker, MS RN EXAM #3 Class 20 Focus: Readings: Objectives: Instructor: Neurological intro Structure and function of the neurological system. Lewis, 2007 Ch. 56 A-C Gay Bondelid, RN MS Class 21 Focus: Neurological Assessment, pathophysiology, and collaborative and nursing management of patients with intracranial problems and craniocerebral trauma Lewis, 2007 Ch. 57 Sole Ch. 12 Hockenberry, Ch 28 Brooks lesson 10 Associated study guides for assigned readings in Lewis and Hockenberry D Gay Bondelid, RN, MS Readings Objective: Instructor: Class 22 Focus: Readings Objective: Instructor: Neurological Pathophysiology and risk factors for stroke and related collaborative and nursing management of the patient with a stroke Lewis, 2007 Ch. 58 Sole pp. 391-404 Associated study guide for Lewis E Gay Bondelid, RN, MS 15 Revised 2/9/2016 Class 23 Focus: Readings: Video: Objective: Instructor: Class 24 Focus: Readings: Objective: Instructor: Class 25 Focus: Readings: Objective: Instructor: Neurological Etiology and pathophysiology of chronic neurologic problems and related collaborative and nursing management Lewis, 2007 Ch. 59 Lilley, 2007 Ch. 12, 13, & 14 Parkinson’s Disease (optional) Associated study guide for Lewis F Gay Bondelid, RN, MS Neurological Pathophysiology, etiology, collaborative and nursing management of patients with peripheral and spinal nerve problems Lewis, 2007, Ch. 61 (pp. 1580-1589, 1609-1611) Sole p. 401 - 404 Hockenberry Ch. 32 Associated study guides for Lewis and Hockenberry G, 1-8 Gay Bondelid, RN, MS Neurological Collaborative and nursing management of the patient with a spinal cord injury Lewis, 2007, Ch. 61 (pp. 1589-1609) Sole pp. 404 - 416 G-9 Gay Bondelid, RN, MS EXAM #4 Class 26 Focus: Readings: Objectives: Instructor: Class 27 Focus: Readings: Objectives: Gastrointestinal intro Review Pathophysiology and Assessment of GI System Lewis, Ch. 39 Sole (2005) Ch. 16, pp. 541-550, or Sole (2009) Ch. 17, pp. 559-568 Associated Study Guides and ATI sections 9A & B Darcie Koffer BS, RN Gastrointestinal Upper Gastrointestinal Disorders Lewis, Ch. 42 Lilley Ch. 51 and 53 Sole (2005) Ch. 16, pp. 550-563, or Sole (2009) Ch. 17, pp. 568-582 Hockenberry, Ch. 24 Grodner, Ch. 17 Associated Study Guides and ATI sections 9C1 16 Revised 2/9/2016 Instructor: Darcie Koffer, BS, RN Class 28 Focus: Readings: Gastrointestinal Lower Gastrointestinal disorders Lewis, Ch. 43 Hockenberry, Ch. 24 Lilley, Ch. 52 Grodner, Ch. 17 Associated Study Guides and ATI sections 9C2 Darcie Koffer, BS, RN Objectives: Instructor: Class 29 Focus: Readings: Objectives: Instructor: Class 30 Focus: Readings: Objectives: Instructor: Gastrointestinal Liver, Biliary Tract, and Pancreatic Problems Lewis, Ch. 44 Sole (2005) Ch. 16, pp. 563-580, or Sole (2009) Ch. 17, pp. 583-603 Grodner, Ch. 18 Associated Study Guides and ATI sections 9D Darcie Koffer, BS, RN Gastrointestinal Pharmacology Related to GI Disorders Lewis, Ch. 42, 43, 44 Lilley, Ch. 51, 52, 53 Associated Study Guides and ATI sections 9E Darcie Koffer, BS, RN EXAM #5 EXAM #6 COMPREHENSIVE FINAL EXAM- Wed., Dec. 16, 1200-1400 Rooms TBA 17 Revised 2/9/2016 August 2009 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 In-service Week 18 In-service Week 19 In-service Week 20 In-service Week 21 In-service Week 22 27 0900-1000 Dosage calc help 1000-1230 Theory 2 Genitourinary/Renal 28 F-S Clinical #2 29 F-S Clinical #3 Transition Class orientation 13-1500 Aspen 176 23 Forms due on 8/24/08: Handbook validation Health insurance Car insurance Clinical confidentiality Davita confidentiality Drug/Alcohol 30 24 0800-1100 Meditech orientation Aspen 144 1200-1600 Clinical #1 for all Students TAY 276-277 [6 forms due ] Dosage calc test opens Portfolio due 25 1000-1230 Theory 1 Fluid/electrolytes Acid/base imbalance 1400-1600 T & L Lab Home Health 26 M-W Clinical #2 SLMV Orientation 0700-1300 Sunflower 0900-1100 Case study #56 due 31 M-W Clinical #3 Case study #56 due ORIENTATION PORTFOLIO DUE TO CLINIC ORIENTATION PORTFOLIO DUE TO CLINICAL INSTRUCTOR AL INSTRUCTOR 18 Revised 2/9/2016 September 2009 6 7 HOLIDAY No clinical 1 1000-1230 Theory 3 Renal/ESRD Dialysis presentation 1400-1600 NURR 202 class 2 M-W Clinical #4 3 1000-1230 Theory 4 Burns 4 F-S Clinical # 4 8 1000-1230 Unit #1 Exam 9 M-W Clinical #5 10 1000-1100 Theory 6 Respiratory 11 F-S Clinical # 5 12 F-S Clinical # 6 #1 Test Review 16 M-W Clinical #7 18 F-S Clinical # 7 19 F-S Clinical # 8 1000-1230 Theory 7 Case Study #29 due 17 1000-1230 Theory 8 Respiratory 22 1000-1230 Theory #9 Respiratory 1400 Resp. T&L 23 M-W Clinical #9 24 1000-1100 Theory 10 25 F-S Clinical # 9 1000-1230 Theory 11 Hematology 1400-1600 NURR 202 class 30 M-W Clinical #11 Dosage calculation Exam closes 1115-1230 Theory 5 5 HOLIDAY No clinical Resp. Intro 1400 Chest tubesT & L 13 14 M-W Clinical #6 15 0900-1000 Unit Respiratory 1400 Trach T & L 20 27 21 M-W Clinical #8 28 M-W Clinical # 10 29 Hematology Teaching plan #1 due Care plan #1 due 19 Revised 2/9/2016 Case Study #29 due Teaching plan #1 due 26 F-S Clinical # 10 October 2009 4 5 M-W Clinical # 12 6 1000-1100 Resp/Hemo Exam 1115 11 12 HOLIDAY No Clinicals 18 19 2nd Clinical Rotation Begins M-W Clinical #1 SLMV orientation 0700-1300 Sunflower 09001100 26 M-W Clinical #3 25 1 1000-1230 Theory 12 Hematology 2 F-S Clinical # 11 Care plan #1 due 3 F-S Clinical # 12 7 M-W Clinical #13 8 Theory 14 Cardiac 9 F-S Clinical # 13 10 HOLIDAY No Clinicals 14 M-W Clinical # 14 15 1000-1230 Theory 16 Cardiac 1300-1600 Meditech training Sunflower SLMV 16 F-S Clinical # 14 Trach DVD due to second clinical instructor 17 No Clinicals 21 M-W Clinical #2 Case Study #15 due 22 1000-1100 Theory 18 Cardiac 23 F-S Clinical #1 Case Study #15 due 24 F-S Clinical #2 28 M-W Clinical # 4 29 1000-1115 30 F-S Clinical # 3 31 F-S Clinical # 4 Theory 13 Cardiac Intro 1400-1600 NURR 202 class 13 0900-1000 Hemo/Resp Test Review 1000-1230 Theory 15 Cardiac 1400 T & L lab ECG 20 1000-1230 Theory 17 Cardiac 1400-1600 NURR 202 class 27 1000-1230 Theory 19 Cardiac 1400-1600 NURR 202 class 1130-1230 Theory 20 Neuro Intro 20 Revised 2/9/2016 Cardiac Exam November 2009 1 2 M-W Clinical #5 3 1000-1230 Theory 21 Neuro 1400-1600 NURR 202 class 4 M-W Clinical # 6 Teaching plan #2 due Final Trach DVD due 5 1000-1230 Theory 22 Neuro 6 F-S Clinical # 5 Teaching plan #2 due Final Trach DVD due 7 F-S Clinical # 6 8 9 M-W Clinical # 7 Case Study # due 10 1000-1230 Theory 23 Neuro 1400-1600 NURR 202 class 11 HOLIDAY No Clinicals 12 1000-1230 Theory 24 Neuro 13 F-S Clinical # 7 Case Study # due 14 F-S Clinical # 8 Care Plan # 2 due 15 16 M-W Clinical # 8 17 1000-1230 Theory 25 Neuro 18 M-W Clinical # 9 20 F-S Clinical #9 21 F-S Clinical # 10 Care Plan #2 due 1400 NeuroT & L 19 1000-1100 Neuro exam 1115-1230 Theory 26 GI Intro 23 M-W Clinical # 10 24 0900-1000 Exam Review 1000-1230 Theory 27 GI 25 HOLIDAY No Clinicals 26 HOLIDAY 27 HOLIDAY 28 No Clinicals 22 ATI Exams opens 29 30 M-W Clinical #11 21 Revised 2/9/2016 December 2009 1 1000-1230 Theory 28 GI 2 M-W Clinical #12 3 1000-1230 Theory 29 GI 4 F-S Clinical # 11 5 F-S Clinical # 12 1400 T & L Ostomy Case study # 9 due 6 7 M-W Clinical #13 8 1000-1230 Theory 30 GI 9 M-W Clinical #14 Case Study # 9 due 10 1000-1100 GI Exam 11 F-S Clinical # 13 12 F-S Clinical # 14 1300-1400 GI Test Review 13 14 ATI Exam closes at 1700 15 16 Final Exam 1200-1400 Rooms TBA 17 18 19 20 21 22 23 24 25 26 22 Revised 2/9/2016 COURSE: Course Name: Central Course Objective: Theory Objective: Level Objectives III through VIII III through VIII NURR 201 Advanced Nursing Interventions Part 1 Applies the concepts of caring, wellness, and illness in meeting the needs of unique individuals with increasingly complex health issues through the use of the nursing process and critical thinking. Analyzes the needs of the unique individual with the focus on advanced medical/surgical health conditions. Student Objectives 1. Fluid & Electrolytes, acid-base imbalances A. Pathophysiological deviations in patients experiencing fluid and electrolyte imbalances. 1. Causes, clinical manifestations, and therapeutic and nutritional management of imbalances in: Potassium, sodium, calcium, magnesium, and phosphate. 2. Fluid excess/deficit: clinical manifestations, therapeutic and nutritional management B. Acid Base Imbalances 1. Metabolic Acidosis and alkalosis; Respiratory acidosis and alkalosis 2. Compensatory mechanisms 3. Systematic assessment of arterial blood gases. C. Oral and IV fluid and electrolyte replacement 2. Genitourinary system disorders: Describe the pathophysiological impact on patients experiencing impairments in the functioning of the genitourinary system: A. Structures, functions, assessment and diagnostic studies of the urinary system B. Urinary tract infection and pharmacological management of the adult and child 1. Lower UTI – cystitis 2. Upper UTI – acute and chronic pyelonephritis 3. Urethritis 4. Urethral diverticula 5. Interstitial cystitis 6. Renal Tuberculosis C. Disorders of the kidney: etiology, clinical manifestations, therapeutic pharmacologic, and nutritional management of the adult and child 1. Acute and chronic glomerulonephritis and acute poststreptococcal glomerulonephritis 2. Good pasture Syndrome 23 Revised 2/9/2016 Learning Activities Lecture/class discussion Readings: Lewis et al., 2007, Ch. 17 Associated Study Guide for Lewis Adams & Koch, Ch. 42 Prior to class: Complete the Study guide (with answer sheet) provided in the assignment section of Blackboard Lecture/class Discussion Readings: Lewis, 2007 Ch. 45 & 46 Associated study guide for Lewis Hockenberry, Ch. 27 Brooks, Lesson 4 Adams & Koch, Ch. 51 Preusser Case Study, Ch 5, #59 Evaluation Quizzes Exam Practice assignment Quiz Exam Quiz Exam III through VIII III through VIII 3. Nephrotic syndrome D. Obstructive uropathies: Etiology, clinical manifestations, therapeutic pharmacologic, and nutritional management 1. Urinary tract calculi 2. Strictures: Ureteral or urethral E. Renal Vascular Problems 1. Nephrosclerosis 2. Renal artery stenosis 3. Renal vein thrombosis F. Hereditary renal disease 1. Polycystic kidney disease G. Neoplastic disorders of the urinary tract 1. Wilms Tumor 2. Kidney, bladder, or prostate cancer H. Urinary incontinence and retention I. Instrumentation 1. Ureteral catheters 2. Suprapubic catheters 3. Nephrostomy tubes J. Surgery of the urinary tract 1. Urinary diversion 3. Renal Failure A. Acute renal failure 1. Etiology, pathophysiology, clinical manifestations, therapeutic pharmacological management, nutritional therapy, and nursing management 2. Uremia; etiology, pathophysiology, clinical course 3. Initiating, oliguric, diuretic, and recovery phases of renal failure 4. Diagnostic studies B. Chronic kidney disease (CKD); clinical manifestations, metabolic disturbances, therapeutic collaborative management 1. Metabolic disturbances, electrolyte and acid-base balance, hematologic system, and other system affected by CKD 2. Pharmacologic therapy 3. Nutritional therapy 4. End stage renal disease 5. Dialysis- peritoneal and hemodialysis 6. Kidney Transplantation 4. Burns A. Pathophysiological deviations that occur with patients experiencing burns; causes, prevention, clinical manifestation, and complications of burn injuries. 24 Revised 2/9/2016 Lecture/class discussion Readings: Lewis, 2007 Ch. 47 Associated study guide for Lewis Sole, 2009, Ch. 15, or Sole, 2005, Ch. 14 Murphy study guide for Chapter 27 (Hockenberry) Grodner, 2007, Chapter 21 Adams & Koch, Ch. 35 Lecture/class discussion Quiz Exam Case Study Quiz Exam III-VIII B. Types of burns 1. Thermal burns 2. Chemical burns 3. Smoke and inhalation injury 4. Electrical burns C. Classification of burn injury 1. Depth, extent, location 2. Patient risk factors D. Phases of burn management; nursing management in each phase, including airway management, pharmacologic therapy, fluid resuscitation, nutritional therapy, and wound care 1. Pre-hospital care 2. Emergent phase 3. Acute phase 4. Rehabilitation phase F. Nursing and collaborative management for the patient with burns. 1. Airway management 2. Fluid therapy 3. Wound care 4. Drug therapy 5. Nutritional therapy 6. Pain management 5. Respiratory A. Describe the structure and function of the upper and lower respiratory tract and chest wall. B. Differentiate normal and abnormal findings of altered pulmonary function and identify nursing assessment related to the following clinical manifestations. 1. Dyspnea 2. Abnormal breathing pattern 3. Hypo/hyperventilation 4. Cough/hemoptysis/sputum 5. Cyanosis 6. Pain 7. Clubbing 8. Chest deformities 9. Sounds breath/voice/percussion C. Identify common measures of pulmonary function and relationship of lung volumes and capacities. D. Analyze difference between restrictive and obstructive pulmonary disease E. Identify and describe the etiology, pathophysiology, clinical 25 Revised 2/9/2016 Readings: Lewis, 2007 Ch. 25 Hockenberry, 2009, Ch. 30; pp. 1091-1104 or Hockenberry, 2005, pp. 1129-1145. Grodner, 2007, Ch. 15, pp. 351-355 Brooks, Lesson 2 Sole, 2009,Ch. 20, or Sole, 2005, Ch. 19 Lecture/class discussions/case studies Readings: Brooks Lesson 3 Lewis Chapters 26, 27, 28, 29 Lewis Chapter 17, 333-341 Sole, 2009, Ch. 9, pp. 173-193, pp. Sole, 2005, pp. 159 – 179 Grodner, Chapter 20. pp 460-463 Lilley, 2007, Ch. 35, 36, 37, 38, & 40 Hockenberry Chapter 23 Murphy Chapter 23 Preusser, 2009, Ch. 2 Exam Quiz Case Study Written assignment III-VIII manifestations, interdisciplinary care, and appropriate nursing care of adults with upper respiratory problems. 1. Nasal fracture 2. Expistaxis 3. Chronic Sinusitis 4. Influenza 5. Sleep Apnea 6. Tracheostomy 7. Laryngectomy F. Identify basics of respiratory acid-base physiology with respiratory alterations. Priority nursing diagnosis for acid-base disturbance, collaborative and nursing management of a patient experiencing an acid-base disturbance G. Identify and describe etiology, pathophysiology, clinical manifestations, interdisciplinary care, and appropriate nursing care of patients with lower respiratory and obstructive problems. 1. Pneumothorax 2. Acute bronchitis 3. Pneumonia 4. Tuberculosis a. Diagnostic tests: Mantoux test, CXR, sputum for acid fast bacillus b. Drug regimen 5. COPD emphysema and chronic bronchitis a. use of oxygen, methods of administration, b. CO2 narcosis, and oxygen toxicity c. nutritional therapy for the COPD d. patient teaching 6. Asthma a. Compare the inflammatory process early vs. late phase b. Diagnostic measures and classification c. Nurses role in prevention d. Management during an acute attack e. Current recommendations for pharmacologic treatment 7. Lung Cancer a. Risk factor for lung cancer b. Nurses role in primary prevention c. Nursing implications for three standard d. Treatments of lung cancer 26 Revised 2/9/2016 III-VIII e. Surgical Therapy 8. Radical neck dissection and other surgical interventions 9. Bronchiectasis 10. Cystic Fibrosis H. Identify various pharmacologic agents used to treat respiratory disorders and discuss nursing implications for patients receiving these medications. 1. Corticosteroids 2. Beta agonist 3. Mast cell stabilizers 3. Leukotriene modifiers i.e. Singular 4. Methylxanthines 5. Anticholinergics 6. Expectorants and mucolytics 7. Antitussives I. Identify how respiratory function is affected in infants and children by structural differences and immunologic immaturity. J. Identify and describe the etiology, pathophysiology, clinical manifestations, and interdisciplinary care and appropriate nursing care of the following pediatric respiratory disorders. 1. Croup Syndromes 2. Acute epiglottitis 3. Acute Laryngitis 4. LTB 5. Acute spasmodic laryngitis 6. Bacterial tracheitis 7. Pharyngitis 8. Tonsillitis 9. Pneumonia 10. Otitis Media 11. RSV 12. Pertussis 13. Tuberculosis 14. Asthma 15. Cystic Fibrosis K. Describe the diet therapy, rationale and related nursing interventions used to meet the nutritional needs of patients with respiratory disorders. 6. Hematologic/Lymphatic System A. Review the pathophysiology of the hematologic and lymphatic systems of adult and children B. Differentiate the types of blood cells and their function. 27 Revised 2/9/2016 Lecture/class discussions Practice NCLEX questions Video: Blood Written exam Quizzes C. Identify assessment findings common to deviations in the hematologic/lymphatic systems. 1. Assessment findings 2. Lab data D. Interpret the nurses’ role in diagnostic studies of the hematologic and lymphatic systems. E. Identify and describe the etiology, pathophysiology, interdisciplinary care, risk factors, diet therapy and appropriate nursing care of adults and children with the following hematologic/lymphatic system disorders: Red blood disorders 1. Anemia a. Generalized anemia b. Iron-deficiency anemia c. Thalassemia d. Vitamin B12 deficiency e. Folate deficiency f. Acute hemorrhagic anemia g. Aplastic anemia h. Anemia of chronic illness 2. Sickle cell disease 3. Hemochromatosis 4. Polycythemia Platelet disorders 5. Thrombocytopenia 6. Hemophilia A & B 7. DIC White blood cell disorders 8. Neutropenia 9. Myelodysplastic Syndrome 10. Leukemia Lymph system disorders 11. Hodgkin’s Lymphoma 12. Non-hodgkin’s Lymphoma 13. Multiple Myeloma F. Explain the pharmacologic interventions as they relate to hematologic disorders for the following: 1. Vitamins and Minerals a. Vitamin K b. Cyanocobalamin c. Iron d. Folic Acid 28 Revised 2/9/2016 Required Reading: Lewis; Ch. 30 Lewis Ch. 31 Sole (2005) Ch. 15 or Sole (2009) Ch. 16 Hockenberry (2005) Ch. 26, pp. 939-972 and pp. 978-980, or Hockenberry (2009) Ch. 26, pp. 912939 and pp. 943-946 Lilley; Ch. 49, pp. 767-769 Ch. 54, pp. 832-833, pp. 836-838 Chapter 56 Grodner; Ch. 7, pp. 137-140 Ch. 8 pp. 174-177 Review Lilley and Grodner 2. III-VIII Hematopoietic agents a. Erythropoietin b. Neupogen G. Identify the different types of, care involved, and adverse reactions in blood component therapy. 7. Cardiovascular A. Review the anatomy, physiology and assessment of the cardiovascular system in adults and children. 1. Heart and vascular system 2. Conduction system 3. Mechanical system B. Identify pertinent assessment findings that are related to the cardiovascular system 1. Subjective data 2. Objective data 3. Assessment abnormalities, etiology and significance 4. Geriatric differences C. Emphasize the role of the autonomic nervous system in regulation of the cardiovascular system. D. Describe the pathophysiology, clinical manifestations, complications, nursing and collaborative care of patients with hypertension. 1. Mechanisms involved in regulation of BP 2. Classification of hypertension 3. Primary versus secondary hypertension 4. Hypertensive crisis 5. Pediatric hypertension E. Identify strategies the nurse implements in the prevention of hypertension; risk factors, nutrition, patient and family teaching. F. Describe the pathophysiology, clinical manifestations, and complications of coronary artery disease. 1. Modifiable risk factors 2. Unmodifiable risk factors 3. Cultural and ethnic considerations 4. Types of serum lipids 5. Health promoting behaviors for decreasing risk factors 6. CAD in women G. Describe the pathophysiology, clinical manifestations, complications, diagnostic studies, nursing and collaborative care for patients with angina. H. Describe the clinical pathophysiology, clinical manifestations, complications, diagnostic studies, nursing and collaborative care 29 Revised 2/9/2016 Review Lewis, Sole, and Hockenberry Lecture, Class Discussion, Case studies, discussion Reading: Lewis; Chapter 32 Sole, 2005, Ch. 11, or Sole 2009, Ch. 12 Hockenberry, 2005, Ch 7, pp. 139146 and 160-162 or Hockenberry, 2009 Ch. 6, pp. 145-148. Brooks; Lesson 6 Lewis; Chapter 33 Grodner; Chapter 20 Lilley; Chapter 24, 25 Hockenberry, Ch. 25 Lewis; Chapter 34 Lilley; Chapter 21. 22, 23, 27 and 28 Exam Quizzes Case study I. J. K. L. for patients following a myocardial infarction. 1. Emotional and behavioral responses to MI 2. Patient and family teaching Identify pharmacologic therapy and the corresponding nursing management for patients with coronary artery diseases. 1. Positive Inotropic Drugs 2. Antidysrhythmic Drugs 3. Antianginal Drugs 4. Antilipemic Drugs 5. Coagulation Modifier Drugs 6. Morphine Describe the clinical pathophysiology, clinical manifestations, complications, diagnostic studies, nursing and collaborative care for patients with or at risk for sudden cardiac death. Describe the clinical pathophysiology, clinical manifestations, complications, diagnostic studies, nursing and collaborative care for adults and children with heart failure and cardiomyopathy. 1. Types of heart failure (HF) 2. Acute decompensated HF and pulmonary edema a. Core measures for HF 3. Chronic HF 4. Drug therapy 5. Nutritional therapy 6. Cardiac transplantation Dysrhythmias M. Describe the clinical pathophysiology, clinical manifestations, complications, diagnostic studies, nursing and collaborative care for patients with inflammatory and structural heart disorders. 1. Infective endocarditis 2. Pericarditis 3. Myocarditis 4. Rheumatic fever and heart disease 5. Cardiomyopathy N. Describe the clinical pathophysiology, clinical manifestations, complications, diagnostic studies, nursing and collaborative care for patients with vascular disorders. 1. Peripheral arterial disease 2. Aortic aneurysms 3. Disorders of the vein O. Explain the purpose and actions of anticoagulant therapy and the nursing management of patients receiving them. 30 Revised 2/9/2016 Lewis; Chapter 35 Lewis Chapter 37 Lewis; Chapter 38 All All 8. Neurological Disorders A. Describe the structure and function of the nervous system 1. Central nervous system 2. Peripheral nervous system 3. Autonomic nervous system 3. Cerebral circulation B. Assessment of the nervous system 1. Mental status 2. Cranial nerves 3. Motor system 4. Sensory system 4. Reflexes C. Diagnostic studies used to assess the nervous system and related nursing actions. 1. Lumbar puncture 2. Radiologic studies 3. Electrographic studies D. Pathophysiology, clinical manifestations, pharmacologic management, and collaborative care of patients with acute intracranial problems 1. Intracranial pressure a. Identify normal physiologic mechanism that maintains constant intracranial pressure (ICP) b. Classify common etiologies of conditions associated with increased intracranial pressure c. Differentiate decorticate and decerebrate posturing and etiology 2. Unconsciousness a. Classify various causes of unconsciousness b. Explain the mechanism of unconsciousness c. Generate an outline of nursing management for the unconsciousness patient 3. Generate outline for nursing management of the patient with increased ICP 4. Head Injury a. Differentiate type of head injury by mechanism of injury, clinical manifestation and treatment 4. Brain tumor a. Compare the types, clinical manifestations, and collaborative care of patients with brain tumors. b. Describe nursing management of the patient with a brain tumor. 5. Meningitis 31 Revised 2/9/2016 Lecture/Class discussion Reading: Lewis, 2007 Ch. 56 Class case studies Exam Quiz In-class assignment Case Study Lecture/class discussion Reading: Lewis, 2007 Ch. 57 Sole Ch. 12 Hockenberry, Ch 28 Brooks lesson 10 Associated study guides for assigned readings in Lewis and Hockenberry Quiz Exam Case Study Reading: Lewis, 2007 Ch. 58 Sole pp. 391 - 404 Associated study guide for Lewis Quiz Exam Lecture/class discussion Reading: Quiz Exam All a. Describe the primary causes of meningitis. b. Describe collaborative care and nursing management of meningitis. 6. Encephalitis, rabies, and brain abscess a. Compare the primary causes, collaborative care, and nursing management of encephalitis and brain abscess. b. Describe the etiology, clinical manifestations, and nursing and collaborative management of the patient with rabies. E. Connect pathophysiology, clinical manifestations, pharmacologic management, and collaborative care of patients with a stroke 1. Identify incidence and risk factors 2. Three types of stroke: Thrombotic, embolic, and hemorrhagic 3. Clinical manifestations of each type of stroke 4. Collaborative care; preventative, acute, and rehabilitative care of stroke patient 5. Describe surgical interventions 6. Pharmacologic and diet therapy recommended for stroke patients 7. Generate an outline for nursing management of the stroke patient F. Connect pathophysiology, clinical manifestations, pharmacological, collaborative care and gerontologic considerations of patients with chronic neurological problems 1. Headache a. Compare and contrast different types of headaches. b. Describe the etiology, clinical manifestations, collaborative care, and nursing management of tension-type, migraine, and cluster headaches. 2. Seizure disorder including complications, patient and family teaching a. Describe the etiology of seizure disorders. b. Compare and contrast nursing management, collaborative care, and complications of generalized and partial seizures. c. Outline the major goals of treatment for patients with seizures. 3. Multiple Sclerosis a. Describe the etiology of multiple sclerosis. b. Describe diagnostic studies utilized for multiple sclerosis. c. Describe clinical manifestations and nursing and collaborative care of the patient with multiple sclerosis. d. Outline the major goals of treatment for patients with multiple sclerosis. 4. Parkinson’s Disease a. Describe the etiology of Parkinson’s disease. b. Describe diagnostic studies utilized for Parkinson’s disease. c. Describe clinical manifestations and nursing and collaborative 32 Revised 2/9/2016 Lewis, 2007 Ch. 59 Lilley, 2007 Ch. 12, 13, & 14 Lecture/class discussion Video: Parkinson’s Disease Associated study guide for Lewis Quiz Exam Reading: Lewis, 2007 Ch. 61 Sole p. 401 - 404 Hockenberry Ch. 32 Associated study guides for Lewis and Hockenberry Lecture/class discussion Reading: Sole pp. 404 – 416 ATI Adult Med-Surg Nursing pp. 762-879 Quiz Exam All care of the patient with Parkinson’s disease. d. Outline the major goals of treatment for patients with Parkinson’s disease. 5. Myasthenia Gravis a. Describe the etiology of Myasthenia Gravis. b. Describe diagnostic studies utilized for Myasthenia Gravis. c. Describe clinical manifestations and nursing and collaborative care of the patient with Myasthenia Gravis. d. Outline the major goals of treatment for patients with Myasthenia Gravis. 6. Restless legs syndrome a. Describe the etiology of Restless legs syndrome. b. Describe clinical manifestations and nursing and collaborative care of the patient with restless legs syndrome. c. Outline the major goals of treatment for patients with restless legs syndrome. 7. Amyotrophic Lateral Sclerosis a. Describe the etiology of Amyotrophic Lateral Sclerosis. b. Describe diagnostic studies utilized for Amyotrophic Lateral Sclerosis. c. Describe clinical manifestations and nursing and collaborative care of the patient with Amyotrophic Lateral Sclerosis. d. Outline the major goals of treatment for patients with Amyotrophic Lateral Sclerosis. 8. Huntington’s Disease a. Describe the etiology of Huntington’s Disease. b. Describe diagnostic studies utilized for Huntington’s Disease. c. Describe clinical manifestations and nursing and collaborative care of the patient with Huntington’s Disease. d. Outline the major goals of treatment for patients with Huntington’s Disease. G. Connect etiology, pathophysiology, clinical manifestations and collaborative care of patients with peripheral nerve and spinal cord problems. 1. Trigeminal neuralgia a. Describe the etiology of Trigeminal Neuralgia. b. Describe diagnostic studies utilized for Trigeminal Neuralgia. c. Describe clinical manifestations and nursing and collaborative care of the patient with Trigeminal Neuralgia. d. Outline the major goals of treatment for patients with Trigeminal Neuralgia. 2. Bell’s Palsy 33 Revised 2/9/2016 All a. Describe the etiology of Bell’s Palsy. b. Describe diagnostic studies utilized for Bell’s Palsy. c. Describe clinical manifestations and nursing and collaborative care of the patient with Bell’s Palsy. d. Outline the major goals of treatment for patients with Bell’s Palsy. 3. Guillain Barre’ a. Describe the etiology of Guillain Barre’. b. Describe diagnostic studies utilized for Guillain Barre’. c. Describe clinical manifestations and nursing and collaborative care of the patient with Guillain Barre’. d. Outline the major goals of treatment for patients with Guillain Barre’. 4. Botulism a. Describe the etiology of Botulism. b. Describe diagnostic studies utilized for Botulism. c. Describe clinical manifestations and nursing and collaborative care of the patient with Botulism. d. Outline the major goals of treatment for patients with Botulism. 5. Tetanus a. Describe the etiology of Tetanus. b. Describe diagnostic studies utilized for Tetanus. c. Describe clinical manifestations and nursing and collaborative care of the patient with Tetanus. d. Outline the major goals of treatment for patients with Tetanus. 6. Neurosyphilis a. Describe the etiology of Neurosyphilis. b. Describe diagnostic studies utilized for Neurosyphilis. c. Describe clinical manifestations and nursing and collaborative care of the patient with Neurosyphilis. d. Outline the major goals of treatment for patients with Neurosyphilis. 7. Spinal cord tumors a. Explain the types, clinical manifestations, collaborative care, and nursing management of spinal cord tumors. 8. Post polio syndrome a. Describe the etiology of Post polio syndrome. b. Describe diagnostic studies utilized for Post polio syndrome. c. Describe clinical manifestations and nursing and collaborative care of the patient with Post polio syndrome. 34 Revised 2/9/2016 III through VIII 9. A. B. C. III through VIII d. Outline the major goals of treatment for patients with Post polio syndrome. 9. Spinal Cord Injury a. Identify risk factors for spinal cord injury b. Describe classification of spinal cord injury. 1. Mechanism of injury 2. Level of injury 3. Degree of injury. c. Explain the physical and psychological problem associated with spinal cord injury. d. Generate outline for nursing management of the patient with a spinal cord injury. Gastrointestinal Disorders Functions and structures of the gastrointestinal system. 1. Ingestion and propulsion of food, digestion, absorption, and elimination through the GI tract. 2. Liver, Biliary Tract, and Pancreas Assessment of the gastrointestinal system 1. Functional health patterns 2. Common assessment abnormalities 3. Diagnostics studies 4. Liver function tests Etiology and pathophysiological impact on all age patients experiencing impairments in the functioning of the gastrointestinal system. Describe diagnosis, treatments, including pharmacologic treatments, and nursing implications for: 1. Upper gastrointestinal problems a. Oral infections and oral cancer b. Structural defects: Cleft lip and palate c. Gastroesophageal reflux disease d. Hiatal hernia e. Esphophageal cancer and other esophageal disorders f. Nausea and vomiting g. Upper gastrointestinal bleeding h. Gastritis i. Pyloric stenosis j. Peptic ulcer disease k. Stomach cancer l. Food poisoning 2. Lower gastrointestinal problems a. Diarrhea, constipation, and fecal incontinence b. Acute abdominal pain and abdominal trauma 35 Revised 2/9/2016 Lecture/class discussion Small group activity Associated Study Guides ATI Associated sections Readings: Lewis, Ch. 39, 42, 43, and 44 Sole (2005) Ch. 16, or Sole (2009) Ch. 17 Hockenberry, Ch. 24 Lilley, Ch. 51, 52, and 53 Grodner, Ch. 17 and 18 Ostomy Lab Ostomy practical experience Quiz Exam Case Study c. d. e. f. g. Irritable Bowel Syndrome Appendicitis Peritonitis Gastroenteritis Inflammatory bowel disease 1. Ulcerative colitis 2. Crohn’s disease h. Intestinal obstruction 1. Hirshsprung’s 2. Intussuception i. Polyps j. Colorectal cancer k. Malabsorption syndromes l. Diverticulosis and diverticulitis m. Hernias n. Anorectal problems o. Ostomy surgery 1. Ileostomy 2. Colostomy D. Liver, Biliary tract, and Pancreatic problems 1. Pathophysiology, clinical manifestations, management, and care of patients with disorders of the liver, biliary tract and pancreas: b. Jaundice c. Hepatitis d. Cirrhosis and cancer of the liver e. Liver transplantation f. Acute and chronic pancreatitis g. Cancer of pancreas and gallbladder h. Disorders of gallbladder and biliary tract E. Explore the drug therapy utilized for treating patients with gastrointestinal disorders. 1. Acid-controlling drugs 2. Antidiarrheals and laxatives 3. Antiemetic agents 36 Revised 2/9/2016 Course: Central Course Objective: NURR 201 Teaching and Learning Lab Applies the concepts of caring, wellness, and illness in meeting the needs of unique individuals with increasingly complex health issues through the use of the nursing process and critical thinking. Teaching & Learning Lab Objective: Demonstrates use of the nursing process and critical thinking for complex skills related to the care of the unique individual in medical surgical settings. Level Student Objectives Learning Activities Evaluation Objectives I-VIII III-VIII III, IV, V, VI, VIII III-VII II-VI 1. Home Health a. Demonstrate by use of the nursing process, the principles of safe, costeffective, evidence based nursing care to patients in the home health setting. b. Discuss the adaptations necessary to meet the needs of the patient in the Home Health setting. 2. Chest Tubes a. Describe the principles of chest drainage for a variety of pts. b. Explain the purpose of the Atrium Pleur-vac and Oasis (dry suction) closed drainage system & identify the purpose for the three compartments. c. Describe nursing responsibilities related to chest tubes pre & post insertion as well as during insertion & removal. d. Describe potential complications such as infection, & tube malposition. e. Demonstrate care of pts with chest tubes in a variety of clinical settings. 3. Tracheostomy a. Demonstrate suction and care of tracheostomy in a variety of clinical settings. b. Describe common complications encountered when caring for a pt. with trach. Airway management Swallowing dysfunction Infection c. Speech with a tracheostomy tube 4. Pulmonary Function/Respiratory therapy/Respiratory agents a. Describe the purpose of pulmonary function tests (PFT’s) and its use in diagnosing disease and disease progression. b. Describe the role of the respiratory therapist and collaboration with nursing c. State major respiratory drug types and specific considerations for their use 5. Basic Cardiac Rhythm Interpretation a. Discuss basic knowledge of electrical activity of the heart and sinus 37 Revised 2/9/2016 Practice Lab Activities: Attend teaching and learning lab Direct observation and clinical experience with a home health and/or hospice nurse in the community. Journal completion according to syllabus requirements Required Reading: Lewis et al., 2007, pp. 588-592 Teaching and Learning Lab Exam Exam/Quiz Required Reading: Lewis et al., 2007, pp. 543-551 Video Demonstration/return demonstration of tracheostomy care and suctioning Exam/Quiz DVD skill check-off must be satisfactorily completed with one or two attempts. Remediation required if not satisfactory the first time. Required Reading: Lewis, 2007 pp. 530-531, and Lilley Chapters 35 & 36, OR Adams & Koch, 2010, Chapters 73-74 Respiratory teaching and learning lab Exam/Quiz Participation in clinical experiences Required Reading: Lewis, 2007, Chapter 36 Exams II-VIII III-VIII rhythm, atrial dysrhythmias, junctional and ventricular dysrhythmias, and heart blocks. b. Identify a systematic approach to rhythm interpretation for normal sinus rhythm and common dysrhythmias. 6. Neurological Assessment a. Perform a neurological assessment: b. Identify the six categories of function assessed to identify the presence, location, and nature of disease of the nervous system. c. Identify the significant subjective and objective data related to the nervous system that should be obtained from a patient. d. Describe the techniques used in the physical assessment of the nervous system. e. Differentiate normal from common abnormal findings of a physical assessment of the nervous system. 7. Ostomy care a. Explain the anatomic and physiologic changes and nursing management of the patient with an ileostomy and colostomy. b. Discuss the adaptations necessary to meet the needs of the patient in the Home Health setting. 38 Revised 2/9/2016 Required Reading: Lewis 1455-1461 Practice Lab Activities: Teaching and learning lab Neurological handout Exam/Quiz Participation in clinical experiences Required Reading: Ostomy handout in Blackboard Lewis, Hockenberry, & Potter (see next page) Practice Lab Activities: Teaching and learning lab 72 hour ostomy appliance experience Quiz Exam Appliance must be worn at least 72 hours for full credit NURR 201 – TUESDAYS: 1400-1600 REQUIRED TEACHING AND LEARNING LABS 08/25/09 Home Health 09/08/09 Chest Tubes; Potter, pp. 950-955; Lewis, 2007, pp. 588-593 09/15/09 Tracheostomy Care Cleaning and Suctioning; Potter, 2009, pp. 931-950, Lewis, 2007, pp. 543-551, and pp.17511757 09/22/09 Pulmonary studies and respiratory medications; Lewis, 2007 pp. 530-531, and Lilley Chapters 35 & 36, OR Adams & Koch, 2010, Chapters 73-74 10/13/09 ECG; Lewis, 2007, Chapter 36 11/17/09 Neuro Assessment, Potter, 2005, Ch. 32, pp. 758-769 or Potter, 2009, pp. 631-639; Lewis, 2007, pp. 1456-1459. 12/01/09 Ostomy Care Lab, Lewis, 2007, pp. 1069-1077 & Potter, 2005, pp. 1380-1385; 1409-1415 or Potter, 2009, pp. 1181-1185, and pp. 1203-1218. 39 Revised 2/9/2016 COURSE: NURR 201 Clinical Course Name: ADVANCED NURSING INTERVENTIONS Central Course Objective: Applies the concepts of caring, wellness, and illness in meeting the needs of unique individuals with increasingly complex health issues through the use of the nursing process and critical thinking. Clinical Course Objective: Demonstrates the nursing process and critical thinking in meeting the needs of the unique individual with increasingly complex medical/surgical conditions. Level Objectives I-VIII Student Objectives Learning Activities Evaluation Given the opportunity, the student will demonstrate by use of the nursing process, the principles of safe, costeffective, evidence based nursing care to patients with increasingly complex needs. Clinical experiences in medical/surgical nursing including assessment, documentation, and interventions utilizing all steps of the nursing process. Implement teaching plans to meet the needs of a patient with common deviations from health. Use of a comprehensive assessment tool to evaluate functional health patterns on assigned patients. Satisfactory in all areas on clinical evaluation by end of semester Satisfactory journal completion, More than 3 late journals will result in clinical failure Satisfactory completion of teaching plans Satisfactory completion of care plans which includes concept mapping Direct observation by instructor during clinical experience Participate in structured clinical post conference Completion of daily tally sheet Test/Quiz Implement discharge plans addressing the needs of a patient utilizing the interdisciplinary team. Demonstrate care of patients with chest tubes in a variety of clinical settings Teaching and Learning Lab Demonstration and return demonstration of tracheostomy care and suctioning in teaching and learning lab Demonstrate care of patients with tracheostomies. Describe the purpose of pulmonary function test (PFT) and its use in diagnosing disease and disease progression. Pulmonary function teaching and learning lab Describe the basic electrophysiology of the heart and correlate to clinical findings. Essentials of Cardiac Rhythm interpretation Teaching and learning lab practice sessions 40 Revised 2/9/2016 DVD skill check-off must be satisfactorily completed with one or two attempts. Remediation required if not satisfactory first time. Test/Quiz and participation in clinical experiences Lewis chapter 36 Perform a complete neurological assessment. Teaching and learning lab Explain the anatomic and physiologic changes and nursing management of the patient with an ileostomy and colostomy. Teaching and learning lab Discuss the adaptations necessary to meet the needs of the patient in the Home Health setting. Summarize the nursing care performed for patients receiving hemodialysis Journal entry Direct observation and clinical experience with a nurse in a community dialysis unit. Instructor evaluation and journaling. Clinical experience with documentation, teaching, accessing internet to obtain teaching materials, searching for evidenced based data to validate nursing interventions. Demonstrate utilization of technology. 41 Revised 2/9/2016 Direct observation and clinical experience with a home health and/or hospice nurse in the community. Clinical experiences, community spin-outs, and teaching and learning labs Demonstrate creativity, innovation & self-awareness through use of reflective thinking in post-conference. Unit exam Tests/Quiz and participation in clinical experiences Test/Quiz and participation in clinical experiences Instructor observation Teaching plans Care plans SECTION C ASSIGNMENTS 42 Revised 2/9/2016 REQUIRED NURR 201 ASSIGNMENTS: CLINICAL ASSIGNMENTS Daily online journaling (May be late no more than three times per rotation) One Student Care Plan (110 points) per clinical rotation One patient/client teaching plan (50 points each) per clinical rotation 2 or 3 case studies per rotation – 25 points each Hospital nursing care plan and education plan: update daily Satisfactory completion of trach care and suctioning DVD; No more than two attempts will be allowed REQUIRED THEORY ASSIGNMENTS Quizzes-Class activities-120 points Unit Tests (5) -- 260 total points Comprehensive Final Exam-75 points (Divided proportionally between all theory content and includes teaching/learning lab content) ALL ASSIGNMENTS WILL BE TURNED IN PERSONALLY, ON THE DUE DATE, TO THE CLINICAL INSTRUCTOR AT THE BEGINNING OF CLINICAL OR (ONLY IF DUE DATE IS A CLINICAL SPIN OUT DAY) ASSIGNMENT MUST BE TIME AND DATE STAMPED ON CAMPUS BY 4 P.M. 43 Revised 2/9/2016 Case Studies Case Studies are due at the beginning of a clinical day and turned in directly to clinical instructor. When the student attends clinical, either on M-W or F-S, determines which due date applies for each case study. Each case study is worth 25 points. Case studies referenced below are from the Preusser (4th Edition) text. Case Study #56 (Preusser, 2009) pp. 289-295 Case Study #29 (Preusser, 2009) pp. 151-155 Case Study #15 (Preusser, 2009) pp. 73-78 Case Study #72 (Preusser, 2009) pp. 371-374 Case Study for GI (TBA) ESRD COPD Endocarditis Subdural hematoma 44 Revised 2/9/2016 Aug. 29 & 31 Sept. 16 & 18 Oct. 21 & 23 Nov. 9 & 13 Dec. 2 & 4 STUDENT CARE PLAN NURR 201 Student___________________________________________Date______________________ DEMOGRAPHIC INFORMATION Patient Date of Admission _______ __ _____ Patient M/F__________________ Marital Status ________Date(s) student cared for patient___________________________ Medical Diagnosis(es)________________________________________________________________ ___________________________________________________________________________ Surgery (If any) and date of surgery_______________________________________________ ___________________________________________________________________________ 45 Revised 2/9/2016 GORDON’S FUNCTIONAL HEALTH PATTERNS STUDENT ASSESSMENT GUIDE (11 points) #1 #2 #3 #4 HEALTH MAINTENANCE MANAGEMENT Admit date Medical Diagnosis Pertinent medical history Pertinent psychosocial history Insurance/Financial concerns Age Allergies/Food and Medicine Erikson’s Developmental Level* Tendency toward which pole* Perception of health status* Immunization status Risk behaviors Discharge needs Medications prior to admission NUTRITION/METABOLIC Diet Recent intake (% of meals) Food Preferences* Abdomen Bowel sounds Nausea NG tube* IV Fluids* Intake/Output (at least 24 hours) Temperature Edema Height and Weight Body mass index* Health risk related to score* ELIMINATION Bladder Bowel patterns Last bowel movement Skin Braden scale score* Risk related to score* Wound/incision Wound drainage system ACTIVITY/EXERCISE Respiratory-Rate SUBJECTIVE 46 Revised 2/9/2016 OBJECTIVE #5 #6 #7 #8 #9 Character of respirations/Cough Color (related to oxygenation) Breath sounds SpO2* Cardiac-Apical pulse rate, rhythm, and sounds Peripheral pulses* Capillary refill time* Blood pressure Range of motion Mobility (describe extent) Assistive equipment ADL performance Leisure and recreation COGNITIVE/PERCEPTUAL Pain (scale, characteristics) Glascow score* Sensory aids Level of consciousness Circulation, Motion, Sensation (CMS) SLEEP/REST Pattern of Sleep Quality/Quantity SELF-PERCEPTION/SELF ESTEEM Describes attitudes about self and perception of abilities* Impact of illness of self* Desire to change self* Nervous or relaxed: supportive data Perceived powerlessness Body posture* Eye contact* Assertive or passive: supportive data Nonverbal cues to self-esteem* Facial expressions* ROLE/RELATIONSHIPS Occupation Recent change in role Comfort with change Marital status Family structure SEXUALITY Menstrual history: children 47 Revised 2/9/2016 #10 #11 Self-breast/testicular exams Impact of illness on sexuality Birth control Prostate specific antigen COPING/STRESS Expression of stress Stressors Usual coping mechanisms Support systems Family support Community resources VALUE/BELIEF Religious preference Spirituality Cultural beliefs and practices Practice of values/beliefs Advance directives DNR *All starred items require either subjective or objective information; all other areas require both subjective and objective data to be included. 48 Revised 2/9/2016 Discharge Plan/Resource Guide Date information obtained_____________________ Anticipated date of discharge___________________ Resources available (explain in detail) Persons/Family: Financial: Community: Support Groups: Socialization: Areas that may require alteration/assistance Food preparation and areas of need: Shopping, housekeeping and maintenance of home: Transportation: Ambulation: Medication/IV therapy: Treatments: Wound Care: Supplies: Self-Care (specify): Homemaker/maintenance (specify): Physical layout of home (specify)(include home safety): 49 Revised 2/9/2016 Anticipated changes in living situation after discharge: Living facility other than home (specify): Referrals (date, source, services): Social services Rehabilitationl services Dietary Home care Respiratory/O2: Psychiatric: Equipment: Supplies: Education (diabetes, OB etc.) 50 Revised 2/9/2016 RESOURCE PLANNING MODEL Community Family Unique Individual Health Care System This model identifies three arenas of the patient’s environment which impact his/her health status: (1) family, (2) health care system, and (3) community. All arenas interact to affect the equilibrium of the individual. An arena is an identified area in the patient’s environment with which he interacts and by which he is influenced. Each arena must be addressed in the plan of care and areas identified that are specific to the patient. PURPOSE OF ARENAS: Each arena should function to fulfill the following purposes for the individual: 1. Promote life, dignity, and integrity 2. Promote positive change and adaptive health behaviors 3. Promote optimal growth/development and maturation Health Care System is that system which provides health care for the individual for a given health problem and includes but is not limited to the acute care agency, nursing care, nutrition, medical care, therapists, pharmacies, rehabilitative facilities, adult and child protective services, and durable medical equipment providers. 51 Revised 2/9/2016 Health care System – Physical Health Care System – Psychosocial/cultural/ spiritual: Family is the primary group within which the patient lives and interacts; the group may be (1) nuclear, (2) extended, (3) single parent (4) significant others, or (5) a combination of these. Information to be included but is not limited to: housing, physical support, home safety, financial support, meal preparation, transportation, roles within the family, ethnicity, social class and family dynamics, including unique communication patterns. Family – Physical: Family – Psychosocial/cultural/spiritual: Community is the geographical area in which the individual lives and or works and which has meaningful impact on the individual’s health status; this may be an extended area as well as the immediate area where the patient lives. This community includes but is not limited to churches, support groups, grocery stores, senior citizen center, public transportation, office on aging, meals prepared and delivered to the home, communication alert systems, legal assistance, community action, law enforcement agencies, leisure, recreation, educational opportunities, and county indigent funding. Community – Physical: Community – Psychosocial/cultural/spiritual: 52 Revised 2/9/2016 Medication Worksheet Classification Medication (Include generic & trade names) Usual dose and route Pt. dose and route Mechanism of action Cite reference(s) per APA format for medication chart here 53 Revised 2/9/2016 Why is pt. taking med Drug interactions with drugs pt. is taking Common and toxic side effects Relevant nursing interventions DIAGNOSIS & PLANNING WORKSHEET (22 points total) Strengths Weaknesses Nursing Diagnosis Scientific Evidence List all defining characteristics considered a strength from your GFHP patient assessment. List and prioritize all defining characteristics considered a weakness from your GFHP patient assessment. Cite Maslow’s Hierarchy of Needs or other appropriate resource to support prioritization. (4 pts) Choose three areas of need from your problem list and in order of priority, state each problem as a NANDA two or three part nursing diagnosis. Cite references for nursing diagnosis. Provide evidence based rationale validating and ensuring accuracy of each nursing diagnosis. Include references. (6 pts) (6 pts) (2 pts) HIGH: List two (2) discharge goals and two (2) teaching needs. Each goal and need has to be individualized, measurable and within a specific timeframe. (4 pts) Discharge Goals MED.: Teaching needs LOW: 54 Revised 2/9/2016 Discharge Goals and Teaching Needs CONCEPT MAP Include: Pathophysiology at the cellular level, relevant GFHP and physical assessment data, medications, lab studies, diagnostic imaging, collaborative care (treatments, meds, OT, PT, ST, RT, diet, activity, medical orders, etc) and nursing care including nursing diagnoses, interventions, rationale, outcomes, and evaluation. You must include at least three nursing diagnoses. You may use more than one sheet of paper. A bi-fold or tri-fold is preferred. Use the grading rubric to ascertain that all necessary material is covered as expected. Linking lines are to be meaningful, accurate and provide a visual relationship between patient symptoms, pathophysiology, and nursing interventions. Emphasis is placed on appropriate linking lines to the pathophysiology. Dotted lines - suggest a correlation. Solid lines - suggest a strong relationship between data. 55 Revised 2/9/2016 NURR 201 Care Plan and Concept Map Name______________________________________Date_____________________________ Objectives: 1. Applies steps of the Nursing Process for an individual assigned in the NURR 201 clinical setting. 2. Incorporates the role of caring and critical thinking when planning, providing, and evaluating care of the assigned individual in the NURR 201 clinical setting. 3. Utilize nursing textbooks and current journal articles as references. 4. Demonstrate comprehension of linking concepts necessary to complete the nursing process for an assigned NURR 201 individual through development of a concept map. Special Instructions: Students must verify patient with clinical instructor for this assignment. Please submit this grading sheet with your completed care plan. Points Possible (1) __________ (11) _________ Demographic information Gordon’s Functional Health Patterns Discharge Resource Plan 1. Agency a. Physical b. Psychosocial and Spiritual 2. Family a. Physical b. Psychosocial and Spiritual 3. Community a. Physical b. Psychosocial and Spiritual (2) __________ (2) __________ (2) __________ (2) __________ (2) __________ (2) __________ Medication worksheet 1. Classification/medication/dosage/route 2. Mechanism of action 3. Identifying why this pt is on the med 4. Identify possible drug interactions, side effects, and symptoms of toxicity. 5. Relevant nursing interventions and assessments Diagnosis & Planning Worksheet 1. Identify strengths and prioritize weaknesses using Maslow’s Hierarchy of Needs. 2. Nursing Diagnosis must be NANDA. 3. Include rationale for prioritization. 4. Identify discharge goals and teaching needs 56 Revised 2/9/2016 (5) __________ (6) __________ (6) __________ (6) __________ (4) __________ Concept Map 1. Pathophysiology at the cellular level or functional (4) __________ level (cite reference). 2. List a minimum of (6) significant patient signs and (3) __________ symptoms obtained through physical assessment. 3. Collaborative Care including: lab, diagnostic imaging, (5) __________ dietary, physical therapy, occupational and respiratory therapy, medical orders, medications (include multidisciplinary needs that may or may not have been previously ordered). 4. Appropriate, specific, and meaningful links throughout. (5) __________ 5. Three (3) NANDA diagnosis derived from GFHP data (3) __________ (correct two or three part statements) 6. Identify individualized, realistic, and measurable desired (6) __________ outcome, including timeframe (one for each nursing diagnosis). 7. List three nursing interventions per NANDA diagnosis (6) __________ that are focused on nursing action. Include specific actions for meds and treatments when appropriate. 8. Identify evidence based rationale for each intervention. (9) __________ (cite reference) 9. Evaluate patient response to interventions. (3) __________ 10. Evaluation of desired outcome. (3) __________ Web assignment (attach copy of online teaching resource) (1) __________ APA Format References, citations, and reference page should follow format according to APA guideline as outlined in the ADN Program Student Handbook. (11) _________ Total (110) _________ 57 Revised 2/9/2016 NURR 201 Nursing Care Plan Grading Rubric Assessment Points Awarded: Provides demographic information of patient while ensuring confidentiality. (1 point) Points Awarded: Utilizes Gordon’s Functional Health Patterns (GFHP) to collect complete data on patient. (11 points possible) Points Awarded: Identifies discharge planning/resource needs of patient using the discharge planning/resource guide assessment form. (2 points possible per discharge resource) Points Awarded: Medications: Identifies all medications patient is taking , unless specific arrangements (otherwise) have been made with the instructor due to the complexity of the pt. (5 points possible) Diagnosis & Planning Points Awarded: Worksheet Strengths: Utilizes Gordon’s Functional Health Pattern (GFHP) assessment to determine patient’s strengths (2 points possible) Points Awarded: Worksheet Weaknesses: Utilizes GFHP assessment to identify and prioritize patient weaknesses utilizing Maslow’s hierarchy of needs or another published tool for Excellent Satisfactory Unsatisfactory 1 Demographic information page is filled out completely and patient confidentiality is completely maintained. 11 GFHP is complete in breadth and depth. All pertinent information is addressed and a clear ‘picture’ of the patient is formed through the collected data. 0.5 Demographic information page may not be complete; or patient confidentiality is not maintained. 0 Demographic information page is vague or not completed or patient confidentiality is not maintained. 0-5 GFHP is vague or incomplete. Little pertinent information is addressed and a clear ‘picture’ of the patient is not provided. 10-12 Discharge planning is complete. All potential resources and support are identified in detail. It is apparent that information provided is patient specific. 4-5 Medication information is accurate, detailed, and patient specific. All patient medications are identified. 6-10 GFHP may be complete, but lacking in depth of information. Pertinent information is addressed, however a clear ‘picture’ of the patient is not necessarily provided through the information presented. Subjective data may be provided in the objective data column. 6-9 Discharge planning is mostly complete. The majority of potential resources and support are identified, however information provided is not necessarily patient specific. 2-3 Medication information is accurate, but lacking in detail and/or patient specificity. Most of the patient’s medications are identified. Interactions pertinent to this pt. with other meds. pt. was taking may not have been identified. 0-1 Medication information is vague, incomplete, and inaccurate. Many of the patient’s medications are not identified. 2 GFHP assessment is utilized to list all relevant patient strengths 1 The majority of strengths are identified but some assessment findings may not be listed. 0 There is little or no identification of strengths from the GHFP assessment. 4 GFHP assessment is utilized to list patient’s weaknesses in priority order and Maslow’s hierarchy of needs (or other valuable resource) 2-3 The majority of weaknesses identified are supported by the GFHP assessment, but the prioritization may not correlate with the NANDA 0-1 The majority of relevant patient weaknesses may be missing, there may be no rationale provided for prioritization, or reference citations are completely 58 Revised 2/9/2016 ≤5 Discharge planning is vague. Potential resources and support are not clearly identified and information provided is not patient specific. prioritizing patient needs. (4 points possible) is utilized to prioritize weaknesses that might interfere with the patient’s health. All references are cited. Points Awarded: Nursing Diagnosis: Must use 2-3 part NANDA approved problem statements, (depending on whether problem is actual or risk for.) NANDA diagnoses must be associated with patient’s main pathology covered in the NCP. (6 points possible) Points Awarded: Scientific Evidence: Scientific, evidence-based rationale is provided for NANDA diagnoses, clearly supporting the relevance of each nursing diagnosis. Reference(s) must be cited appropriately. (6 points possible) Points Awarded: Discharge Goals/Teaching needs: Two appropriate discharge goals and two teaching needs are noted that the student taught the patient prior to discharge. (4 points possible) 5-6 Nursing diagnoses selected are NANDA approved, follow the appropriate format, are correlated with the identified strengths/weaknesses, and are prioritized appropriately. Care Plan/ Concept Map Points Awarded: Criteria #1: Describes pathophysiology of the priority medical problem at the cellular or functional level with reference cited appropriately (4 points possible) Points Awarded: Criteria #2: Identifies a minimum of six Revised 2/9/2016 diagnoses, or logically follow Maslow’s hierarchy or other (evidence-based) priority order. Some assessment findings may not be listed 2-4 The nursing diagnoses selected are NANDA approved, but may not follow the appropriate format. The diagnoses chosen may be loosely correlated with the identified strengths/weaknesses. lacking. 5-6 Strong evidence-based rationale is provided to support the relevance of each nursing diagnoses at the functional level. Reference(s) are cited appropriately in APA format. 2-4 Evidence-based rationale may vaguely support the relevance of the nursing diagnoses, or evidencebased resource may not be appropriate. 0-1 Evidence-based rationale does not support the prioritization of the nursing diagnoses, or rationale is not given. 4 Discharge goals are individualized, measurable, include a timeframe, and are appropriate for the nursing diagnoses. Teaching needs involve information the patient needs to know prior to discharge and should be taught by the student. 2-3 Discharge goals may not be individualized, measurable, include a timeframe, or are not appropriate for the nursing diagnoses. Teaching needs may not be information the patient needs to know prior to discharge or were not actually taught by student. 0-1 Discharge goals and/or teaching needs are missing major components or not applicable for the patient’s diagnoses. 4 Pathophysiology is accurate, detailed, complete, and patient specific. There is clear, detailed identification of the cellular or functional processes of the disease. Pathophysiology correlates with patient’s identified medical problems and reference is cited appropriately from a textbook or peer reviewed medical journal. 3 Six significant signs/symptoms are 2-3 Pathophysiology is accurate and complete. However it is lacking in detail and patient specificity. Cellular or functional processes of the disease are identified, but may not have sufficient detail. Pathophysiology correlates with patient’s identified medical problems. 0- 2 Pathophysiology is brief or even inaccurate. Little attention may be paid to patient specificity and to the cellular or functional processes of the disease. Pathophysiology may not correlate with identified medical problems. 2 Six or less significant signs and symptoms are 59 0–1 Few significant signs and symptoms are identified. They 0-1 The nursing diagnoses are either not NANDA approved, or do not follow the appropriate format. There may be little to no correlation between the identified strengths/weaknesses and the nursing diagnoses. (6) significant signs and symptoms (defining characteristics) from patient assessment and identifies the GFHP# for each. (3 points possible) identified that are patient specific, supported by the GFHP, and support the pathophysiology of the medical diagnosis. Points Awarded: Criteria #3 Collaborative Care: Identifies and includes complete descriptions of all care that may or may not have been ordered. Must include patient specific results as well as normal findings when appropriate. (5 points possible) Points Awarded: Criteria #4: Appropriately correlates (links) the following: pathophysiology, signs and symptoms, lab values, diagnostics, nursing diagnosis and interventions, and medications. (5 points possible) Points Awarded: Criteria #5: NANDA diagnoses derived from GFHP information (3 points possible) 5 The concept map includes a full description of all collaborative care that may or may not have been ordered to enhance the patient’s care including, but not limited to; lab, DI, PT, OT, ST, RT, clinical nutritionist, pharmacist, MD 5 There is a clear correlation identified between all of the areas listed. Utilizes solid lines, dotted lines, arrows, or other technique to indicate specific correlations. Points Awarded: Criteria #6: Identifies individualized, realistic, and measurable desired outcomes, one for each nursing diagnosis, including a time frame. (6 points possible) Points Awarded: Criteria #7: Selects three priority nursing interventions that are focused on the nurse’s behavior and are patient specific (consider GHFP assessment when formulating interventions) (Remember: interventions correlate and assist in achieving the desired outcome and are based on Revised 2/9/2016 3 Correct two or three part statements are made, using NANDA format for three nursing diagnoses from student worksheet. 6 A patient specific, realistic outcome is identified that directly correlates with each nursing diagnosis. The outcome is realistic, measurable, and includes a time frame. 5-6 3 nursing interventions are identified that are directly correlated to achieving the desired outcome and addressing the nursing diagnosis. The interventions are nursing specific, clearly delineate what the nurse is to achieve (who will do what, under what circumstances, by when). identified, however they may not be patient specific, or are not supported by GFHP assessment. There is weak correlation to the pathophysiology of the medical diagnosis. 3-4 Some collaborative care options may have been listed but other areas, not addressed on the concept map, could have improved the patient’s plan of care. The information provided may have been incomplete. likely are not patient specific and are not supported by GFHP assessment. There may be no correlation to the pathophysiology of the medical diagnosis. 3-4 There is a vague correlation identified between one or more of the areas listed but correlations may be too general or do not show relevance of the information. 0-2 No correlation is identified between specific components of the areas listed or all areas are linked inappropriately. 2 Two nursing diagnoses are listed, or NANDA format is not correctly used to state the nursing diagnoses. 0-1 One or no nursing diagnosis is appropriately stated in NANDA format. 4-5 A realistic outcome is identified, however it is either not patient specific or it does not directly correlate with the nursing diagnosis. The outcome is realistic, vaguely measurable and includes a time frame. 3-4 3 nursing interventions are identified however they may or may not directly correlate to achieving the desired outcome and/or addressing the nursing diagnosis. Interventions may be vaguely nursing specific, or do not clearly delineate what the nurse is to achieve Little consideration may have 60 0–3 An outcome is identified, however it is not realistic, is not patient centered, or does not correlate with the nursing diagnosis. It is vaguely (if at all) measurable and may or may not be realistic, or include a time frame. 0-2 There was little or no notation on the concept map of actual or possibly beneficial collaborative care available for the patient. 0-2 Less than three nursing interventions are identified and they are not directly correlated to the desired outcome and/or the nursing diagnosis. The interventions are vaguely nursing specific, or perhaps patient specific. There is little delineation of what the nurse is to achieve or no consideration is made to the patient’s and nurse’s the priority nursing diagnosis). (6 points possible) Points Awarded: Criteria #8: Identifies the evidence-based rationale for each selected nursing intervention (with references for each). (9 points possible) Points Awarded: Criteria #9: Evaluate the patient’s response for each intervention. (3 points possible) Points Awarded: Criteria #10: Desired outcome met? (Include answers to the following: Was the outcome met, and was it appropriate? Were the interventions appropriate for the nursing diagnosis?) (3 points possible) Points Awarded: Web assignment (1 points possible) Points Awarded: APA: Title page, running head, and references according to APA 5th ed. format and criteria as outlined in the student handbook. (11 points possible) Consideration is made to the patient and nurse’s strengths and limitations. 8-9 Scientific, evidence-based rationale is provided for each nursing intervention, that clearly supports how the intervention will aide in achieving the desired outcome and addressing the nursing diagnosis. Reference(s) are cited appropriately. 3 Reflective evaluation of the patient’s observable response to each of the nursing interventions is identified. 3 Reflective evaluation is provided as to whether or not the desired outcome was met and/or to what degree. Thoughtful consideration shown as to whether the outcome and interventions were appropriate for the nursing diagnosis and pt. If not met, possible changes for the future are provided. 1 Hard copy of online patient teaching resource is attached to NCP. Information uses terminology that is appropriate for patient’s learning level. 9-11 APA format is nearly perfect. No spelling or grammatical errors, etc. Consideration is given to number of references. Pt confidentiality is maintained. All references listed on reference page were cited in the body of the paper. been made to the patient’s and nurses’ strengths and limitations. 5-7 Vague evidence-based rationale may have been provided for each nursing intervention, but clear support of how the intervention will aide in achieving the desired outcome and address the nursing diagnosis may not have been provided. 2 Vague evaluation of the patient’s response to each of the nursing interventions is identified or the response listed does not directly correlate to the achievement of the desired outcome. 1-2 Evaluation of the desired outcome was met and/or to what degree is provided, however it may not have displayed reflective thought and analysis. Vague consideration may have been given related to the appropriateness of the outcomes and interventions. Changes for outcomes not met were not appropriate. 0.5 Online teaching resource is attached but the information is either inadequate or it is worded in language that is not appropriate for the level of learning of the patient. 5-8 Few APA format errors. Occasional spelling and/or grammatical errors, which did not obscure the meaning. Consideration is given to number of references. Pt confidentiality is maintained. 61 Revised 2/9/2016 strengths and limitations. 0-4 Little or no evidence-based rationale is provided. There is very little, if any, support in how the intervention will aide in achieving the desired outcome and address the nursing diagnosis. 0-1 Little if any evaluation of the patient’s response to each of the nursing interventions is identified. 0 The evaluation is not reflective and does not display thoughtful analysis. Little, if any, consideration is shown related to the appropriateness of the outcomes and interventions. No possible changes were given for outcomes not met. 0 Online teaching resource is missing. 0–4 Major APA formatting errors. Frequent spelling and/or grammatical errors that obscure the meaning of the paper. No consideration is given to number or references, and/or pt. confidentiality is broken. Reference page may have been missing. TEACHING PLAN LEARNER READINESS: This is an assessment of the patients learning needs. Include a description of the patient, his or her clinical situation, personal history or any significant data related to lifestyle that may impact learning, such as cultural and social issues. Include the patient’s knowledge, skills and attitudes about his or her situation, any previous experience related to health problems, areas of strength that are related to his or her learning, the impact of family or other supportive persons, and the patient’s motivation for learning about his or her situation. GOAL: Goals are statements that describe, in broad terms, what is to be accomplished by the learner. Educational goal statements are written to communicate the expected or intended achievements of the teaching plan. OBJECTIVES: Objectives are not written as a restatement of the goal. Instead, objectives are precise statements that specify the behavior changes needed to achieve the goal. Each learning objective must state the skill or activity the patient must do in order to objectively measure what he or she has learned. (Review Potter and Perry p. 323, Guidelines for writing goals and expected outcomes). Use action verbs to write educational objectives. Examples are: choose, define, describe, differentiate, identify, list, demonstrate, explain, discuss (See Bloom’s taxonomy handout for a complete list). Remember to include a time frame for each objective. 1. Note: Use the number of objectives necessary to meet your stated goal. 2. Must use a minimum of 3 objectives. 3. CONTENT/INFORMATION 1. For each of the objectives listed above, the teaching information or content is included in this section as presented to the patient. This section should be concise and worded at the learner’s level. If you are using demonstration or handouts, include a copy of the handout(s) also. TEACHING STRATEGIES/MATERIALS USED Evidence-Based Rationale: This is the statements of supportive scientific evidence at the foundational level to support the basis for the content information taught to the learner. (cite reference in APA format) Evidence-Based Rationale: This should be statements of supporting data for why you the above listed strategies and materials were the most effective way to present the teaching plan. (cite reference) State the teaching strategies and materials used. (Writing the content and teaching actions in side-by-side columns enables the teacher to compare content with teaching methods and reflect on whether the objectives can be met by the methods indicated). Examples of teaching methods may be demonstration, discussion, as well as teaching tools used to supplement instruction. See Lewis, Heitkemper, Dirksen, O’Brien, & Bucher, 2007, pp. 60-63. 62 Revised 2/9/2016 Pt. Specific Rationale: These are statements why chosen strategy is appropriate for this specific patient in this particular setting. Include teaching strategies and materials used for content #2. 2. Again, this content should be specifically related to objective #2 as stated above and worded at the learner’s level. Evidence-Based Rationale: This is the rationale for content #2. (cite reference) Evidence-Based Rationale: Include the rationale for your selection of teaching methods and materials used above. (cite reference) Pt. Specific Rationale: Include why appropriate for this specific patient. CONTENT/INFORMATION 3. Again, this content should be specifically related to objective #3 as stated above and worded at the learner’s level. TEACHING STRATEGIES/MATERIALS USED Include teaching strategies and materials used for content #3. Evidence-Based Rationale: This is the rationale for content #3. (cite reference) Evidence-Based Rationale: Include the rationale for your selection of teaching methods and materials used above. (cite reference) Pt. Specific Rationale: Include why appropriate for this specific patient. EVALUATION: Evaluation assesses what the patient learned and indicated areas that need additional or repeat teaching. If your objectives were measurable to begin with, evaluation is possible. Learning is evaluated in terms of changed behaviors. Use the same terminology that was used in goal/objectives when stating whether or not goal was met. There are a number of reasons why learning may not have occurred. Some common reasons are that the patient was not ready to learn or had other problems like pain, stress, coping issues or fatigue. The patient may have had inaccurate background knowledge or experience. Your assessment of their learning needs may have been inaccurate. Your objectives may have been ambiguous or incomplete, or your teaching methods may not have been inappropriate for the content or objectives stated. 63 Revised 2/9/2016 OBJECTIVE 1. State your evaluation of objective #1 using the same terminology used when stating the objective. Be specific and include data assessment to validate that objectives were met. OBJECTIVE 2. State your evaluation of objective #2. Again, include specific data to validate objectives were met. OBJECTIVE 3. State your evaluation of objective #3. Include specific data as noted above. REVISION: In the future, how would you have changed this teaching plan for this patient to improve his or her learning? Note: Remember to include an additional reference page that follows APA format for this teaching plan. 64 Revised 2/9/2016 NURR 201 Patient/Client Teaching Plan Special Instructions: Student must verify patient with clinical instructor for this assignment. . Name: _________________________________________ Date: _________________ Objectives: Upon completion of this assignment the student will be able to: 1. Assess the individual learner’s educational needs. 2. Apply the nursing process in the formulation of goals, objectives, evaluations and revisions to patient and family teaching. 3. Utilize various teaching strategies in the clinical setting with an assigned patient. 4. Support information with references Criteria: Possible Points 1. Learner Readiness 7 2. Goal 2 3. Objectives (Minimum of 3 required) 6 4. Content/Implementation 7 5. Evidence-Based Rationale for content (Cite reference) 9 6. Teaching action 2 7. Evidence-Based Rationale & Rationales for teaching action (Cite reference) 3 8. Patient specific rationale __4___ 9. Evaluation 3 10. How would you revise for the next time? 2 11. References in APA 5th edition format, and considering criteria as outlined in the student handbook. 5 Total 65 Revised 2/9/2016 50 Earned Points ______ NURR 201 Teaching Plan Grading Rubric Excellent Points Awarded: Criteria #1: Learner Readiness (7 points) Points Awarded: Criteria #2: Goal (2 points possible) Points Awarded: Criteria #3: Objectives (Minimum of 3 required) (6 points possible) 6-7 A complete description of the patient’s and/or family/significant other’s learner readiness is provided. Attention is paid to the physical, psychological, sociocultural, and educational aspects of the individual. At least six to eight different, specific aspects are considered and discussed. The patient’s preferred learning style is addressed, as well as his/her motivation to learn, and whether or not he/she has ever had experience with the information presented. Satisfactory 3-5 A vague description of the patient’s and/or family/significant other’s learner readiness is provided. Limited attention is paid to the physical, psychological, sociocultural, and educational aspects of the individual. Only three to five different, specific aspects may have been considered and discussed. The patient’s preferred learning style may have been omitted. There was little attention given to the patient’s motivation to learn this material, or his/her previous exposure to the information. 2 A goal is clearly stated. It is not a restatement of the objectives, but describes, in broad terms, what is the main identifiable focus of the teaching session. The goal is focused on the learner. 5-6 Three objectives are presented and each objective is learner-centered and describes in specific detail what is to be achieved by the learner. The objectives are realistically measurable; answering the questions: ‘who will do what, how well, under what circumstances, by when’. A timeframe states when the objective will be achieved. 2-4 Three objectives are presented, however they are not learner-centered, or they fail to describe in specific detail what is to be achieved by the learner. Or the objectives are not entirely realistic and/or measurable. A timeframe may not be given. 66 Revised 2/9/2016 Unsatisfactory 0–2 An incomplete description of the patient’s and/or family’s/significant other’s learner readiness is provided. Little attention is given to the physical, psychological, sociocultural, and educational aspects of the individual. Two or less different, specific aspects are considered. 0 The goal is incomprehensible or does not correlate with the objectives in any manner. It is either way too broad or too specific and is not focused on the learner. The goal is vague and shares remarkable similarities to the objectives. It is not quite broad enough or may not be learner specific. 0-1 Less than three objectives are presented, or they fail to describe realistic, measurable, learner centered activities, with a timeframe. NURR 201 Teaching Plan Points Awarded: Criteria #4: Content/Implementation (7 points possible) Points Awarded: Criteria #5: Evidence-based rationale for content (cite reference appropriately) ( 9 points possible) Points Awarded: Criteria #6: Teaching Strategy or Action (2 points possible) 5-7 Content is clearly described and worded at the learner’s level. The content is clearly thought out and thorough in depth and breadth. 7-9 Supportive scientific references are directly quoted to fully support the basis for the information provided to the patient. The information validates the content presented at the foundational level defining the purpose behind the content. Information is appropriately referenced. 2 A text book teaching strategy is listed that correlates closely with the content provided. The teaching action is appropriately chosen and defined. (Potential teaching actions: lecture, lecturediscussion, discussion, group teaching, demonstration/return demonstration, role play, audiovisual materials, printed materials, internet) Each content area must have a different rationale and/or a different reference supporting it. 67 Revised 2/9/2016 3-4 Content is described, but is not worded at the learner’s level. The content is vague or the information is not thoroughly presented. 0–2 Content is vague or even incorrect. Little effort seemed to have been made to word it at the learner’s level. 3-6 Supportive scientific references are quoted, but are generalized and do not fully support the basis for the information provided to the patient. The rationale may not be provided at the foundational level to support the purpose behind the content. Information may not be appropriately referenced. 1 Teaching rationale may have been appropriately chosen and defined but each content area may have used the same rationale or the same reference. 0–2 Supportive scientific references are vaguely provided. Little support is provided for the information offered to the patient. Information is not appropriately referenced or student does not give credit to the author(s) by using quotation marks when exact words are used from reference(s). 0 The teaching strategy chosen may not have been standard or did not fit with patient scenario and content in any way. No teaching action may have been provided. A teaching strategy may have been chosen however it vaguely correlated with the content provided. Another teaching action would have been more appropriate for the specific situation. Points Awarded: Criteria #7: Evidence-based rationales and rationales for teaching strategy or action (cite reference) (3 points possible) Points Awarded: Criteria #8 Patient specific rationale (4 points possible) Points Awarded: Criteria #9: Evaluation (3 points possible) Points Awarded: Criteria #10: How would you revise for the next time? (2 points possible) 3 Supportive scientific references are directly quoted to fully support the information provided to the patient. Information is appropriately referenced. A reasonable rationale for why the designated teaching action was chosen for the SPECIFIC patient is provided. 4 Rationale is provided clearly stating why the chosen teaching strategy or action was appropriate for presenting this material to this particular patient in this setting. 3 An evaluation of the teaching experience in totality is provided. Reflective analysis is displayed, spelling out how the patient responded to the teaching. Evaluation of each objective is provided, with description of whether or not the objective was met and to what degree. 2 Reflective thought is provided to the revision of the teaching session. Influence of the learner’s readiness, realistic nature of the goals and objectives, and thoroughness and presentation of content is considered. 68 Revised 2/9/2016 2 Supportive scientific references are quoted, but are generalized and do not fully support the information provided to the patient. A rationale for why the designated teaching action was chosen is provided, however it does not correlate with the SPECIFIC patient. 2-3 Rationale provided may not have clearly stated the reason for choosing the teaching strategy. It may have lacked patient specificity. 0–1 Supportive scientific references are vaguely provided. Little support provided for the info offered to the patient. Information may not be appropriately referenced. No rationale why the designated teaching action was chosen for this specific patient… or perhaps it does not reasonably correlate with the patient. 0–1 Patient specific rationale was missing or vague. 2 An evaluation of the teaching experience is provided but it does not display reflective thought and analysis. An evaluation of each objective is provided but it may be vague or may not accurately describe what was achieved by the learner. 0–1 The evaluation is not reflective and does not display thoughtful analysis. An evaluation of each objective is either not completed, or inaccurate. Reflective thought may not have been displayed. 1 Revision does not display appropriate reflective consideration for the teaching session. Reflective thought may not be fully displayed or little attention may be paid to learner readiness. 0 No revision is provided, or no attention may be paid to the learner’s readiness, realistic nature of the goals and objectives, and thoroughness and presentation of content. Points Awarded: Criteria #11: References in APA 5th ed. format, and considering criteria as outlined in the student handbook. (5 points possible) 5 APA format is nearly perfect. No spelling or grammatical errors, etc. Paper is appropriate length with consideration given to number of references. All references listed on reference page were cited in the body of the paper. Pt confidentiality is maintained. 2-4 Few APA format errors. Occasional spelling and/or grammatical errors, however they do not obscure the meaning. Paper is appropriate length and consideration is given to number of references. Pt confidentiality is maintained. 0–1 Major APA formatting errors. Frequent spelling and/or grammatical errors that obscure the meaning of the paper. Paper is inappropriate length or no consideration given to number of references. Pt confidentiality may be broken. Reference Information All written work (excluding case studies) must utilize APA format. Please refer to instructional presentation under “Assignment” button in Blackboard for a summary explaining how to formulate title page, reference citations, reference page, and other expectations. 69 Revised 2/9/2016 PORTFOLIO PURPOSE: The portfolio: 1. 2. Is used to detail information about the students personal and professional progress related to academic and professional career development throughout the ADN program. Will also serve as a critical thinking outcome. DEFINITION OF CRITICAL THINKING A cognitive approach to inquiry that uses intellectual curiosity in a holistic manner for the purpose of making goal-directed decisions and solving problems with respect to the process of nursing. This holistic approach draws upon clarity, relevance, and logic as well as emotion, belief structure, and culture. The process can be carried out autonomously or cooperatively with a goal of reaching a conclusion which can be evaluated through validation. In compiling the portfolio, student will include: a. All graded original work. b. Completed journal submissions, including instructor comments c. Updated professional development plan. Document on professional development plan all ISNA activities, which must include (minimally) membership, attendance at one meeting, participation in one activity and one fundraiser. d. Updated philosophy of nursing e. Updated record of assignments PORTFOLIO WILL BE COLLECTED MINIMALLYAT THE BEGINNING OF EACH CLINICAL ROTATION BY THE CLINICAL INSTRUCTOR AND AT THE TIME OF EVALUATIONS 70 Revised 2/9/2016 Professional Development Form College of Southern Idaho Associate Degree Nursing Program Name: ___________________________________ This form is to be maintained throughout the course of your nursing education. Please update accordingly and bring to ALL clinical evaluations. It should be kept in your portfolio. Identify activities contributing to professional development and the date they occurred: Example of activities: healthcare related in-services, research of a special topic, services projects related to healthcare, ISNA meetings or activities, special presentations as part of post-conference or class, journal articles, recertification (CPR, etc.), college classes outside of program requirements, work in healthcare field, etc. Activities Contributing to Professional Development Date Completed 71 Revised 2/9/2016 Record of Assignments: Present this to your clinical instructor during clinical evaluation. This section is to be updated at the end of each rotation/semester by your clinical instructor. Course Semester Teaching Plan Topic Care Plan Topic 72 Revised 2/9/2016 Instructor Initials/Date Personal Philosophy of Nursing: This is a statement of the principles that guide your practice as a nurse. This philosophy should evolve over time as you gain more experience and insight into your PERSONAL nursing practice. My personal philosophy of nursing at the beginning of my education: ____________________________________________________________________________________________________________ ____________________________________________________________________________________________________________ ____________________________________________________________________________________________________________ ____________________________________________________________________________________________________________ ____________________________________________________________________________________________________________ ____________________________________________________________________________________________________________ ____________________________________________________________________________________________________________ ____________________________________________________________________________________________________________ My personal philosophy of nursing at this point of nursing school: ____________________________________________________________________________________________________________ ____________________________________________________________________________________________________________ ____________________________________________________________________________________________________________ ____________________________________________________________________________________________________________ ____________________________________________________________________________________________________________ ____________________________________________________________________________________________________________ ____________________________________________________________________________________________________________ ____________________________________________________________________________________________________________ ____________________________________________________________________________________________________________ ____________________________________________________________________________________________________________ ____________________________________________________________________________________________________________ ____________________________________________________________________________________________________________ 73 Revised 2/9/2016 SECTION D CLINICAL 74 Revised 2/9/2016 GUIDELINES FOR CLINICAL ACTIVITIES Invasive nursing procedures initially performed by students must be approved by the clinical instructors prior to performing them. The instructor will observe the student or delegate it to the primary RN. After a procedure has been observed to be successful, the student may be given permission to perform subsequent similar procedures with the primary RN*. * A primary RN is an RN who has been previously approached and has agreed to assume responsibility for accurate performance by the student whom she/he is assisting or observing during a procedure. List of Applicable Procedures 1. Preparation of calculated dosages. 2. All medication administration including: Narcotic procurement, IV medications, adding meds into any IV solution, and blood products. Preparation of insulin injections, heparin, lovenox, IV or po digitalis, blood products, TPN, chemotherapy, adenosine, IV dihydroergotamine, IV hydralizine, IV labetolol, IVvasopressin, IV vitamin K, verapamil, interelin, IV methergine, phentolamine, IV narcotic infusions and PCA/Epidural pump medications. Students will follow the hospital policy regarding the administration of IV medications. 3. Central line care and blood draws/ venipuncture. 4. All dressing changes. 5. Airway care (tracheostomy tubes, endotracheal tubes, changing of tracheotomy tubes, suctioning, etc.). 6. Initial postoperative position changes of patients with total joint replacements. 7. Management of patients with major vertebral trauma or surgery. 8. Nasogastric intubations. 9. Urethral catheter insertions. 10. Initial post - TUR prostatectomy catheter irrigations. 11. Initial postoperative and/or postnatal assessment in the recovery room and/or delivery room. Students will not administer medications in recovery rooms. Student's entries on patient's medical records that document care, other than activities for which an instructor or primary RN must be present, need not be cosigned. 75 Revised 2/9/2016 OBJECTIVES FOR CLINICAL SPINOUTS: Objectives for NURR 201 Home Health Spinout A. At the end of this experience, the student will be able to: 1. 2. 3. 4. 5. Describe the role of the home health/hospice nurse as related to: a. Building trust and rapport with patient/client and recognizing their value system. b. Elements of the initial visit. c. Nursing process - assessment, diagnosis, planning, implementation, evaluation. d. Prioritizing nursing care. e. Setting limits with patients/clients. Identify parameters of home visits with regard to Medicare, Medicaid and third-party documentation guidelines for reimbursement. Include quality control and specific documentation forms. Describe patient/client care delivery system with emphasis on: a. Caseload management b. Patient/client education c. Cultural diversity d. Multi-disciplinary services e. Family assessment Determine modifications in infection control in a home environment. Identify adaptations in procedures, equipment, or treatment regimes for delivery of nursing care in the home environment. The student will: 1. Participate with Nurse Designate for two full clinical days in: a. Delivery of home care b. Team meetings c. Documentation 2. Maintain online journaling. ADDITIONAL EXPECTATIONS: 1. 2. 3. 4. 5. 6. 7. Each student must be able to arrange transportation to and from home health experience. CSI students are covered by the college insurance policy as long as the driver and automobile have private insurance coverage. Attendance is necessary for both clinical spin-out days. Students are expected to contact their clinical instructor and agency if unable to attend. Make-up experience will be planned with CSI home health coordinator. Plan for your day to be 0800-1700. The exact seven hours of clinical time will be scheduled by the nurse. Call your assigned Home Health Agency on the afternoon prior to your first scheduled spinout day to establish time and place for meeting with your assigned RN. This may also be an opportunity to learn about the patients you will be visiting. Call again during your spinout week if instructed to do so by your RN designate. Wear professional street clothes (jewelry according to dress code). No Levis. A stethoscope will be necessary for home health visits. Procedures and assessments are to be performed under the direction of RN designate. The student is expected to attend case conferences scheduled during the experience day. 76 Revised 2/9/2016 8. Include home health experience in your journaling. This self-reflection may include your feelings, questions and observations about the home health nursing role. Reflect on relationships between client and caregiver. Objectives for NURR 201 Pediatric Spinout At the end of this experience, the student will be able to: 1. Understand disease process affecting the pediatric patient. 2. Identify adaptations in procedures, equipment, or treatment regimes for delivery of nursing care in the pediatric setting 3. 4. 5. 6. Complete an age appropriate assessment on a pediatric patient. Recognize variations from norms regarding assessment findings. Accurately document assessment findings. Interpret vital sign changes in pediatric patients and correlate to nursing priorities for care. 7. Observe and/or demonstrate administration of medications and immunizations within the pediatric population. Objectives for NURR 201 Hemodialysis Spinout At the end of this experience, the student will be able to: 1. Observe the pre-dialysis care performed. Assist with obtaining baseline vital signs and review pre-dialysis labs (BUN, serum creatinine, sodium, potassium, Hct.). 2. Describe the fistula/graft (site and type) and how it was accessed for dialysis. 3. Summarize the dialysis procedure; i.e., what is monitored, medications given, and 4. possible complications. 5. Identify patient teaching, (before, during, and after dialysis). Review patient teaching 6. literature. 7. Identify dietary modifications required for patients with recurring hemodialysis. 8. Answer all the above objectives in your journaling. Objectives for NURR 201 Respiratory Therapy Spinout: 1. Describe the relationship between ventilation and perfusion. 2. Identify the processes involved in gas exchange. 3. Identify the different types of respiratory equipment used in oxygen administration 4. Identify assessment findings commonly seen with individuals experiencing: a. Hyperventilation b. Hypoventilation c. Hypoxemia Objectives for NURR 201 Cardiac Cath Lab Spinout: 1. Identify the American Heart Association current treatment recommendations for patients experiencing Acute Coronary Syndrome. 2. Describe the purpose for, the procedure and possible complications related to the following coronary interventions: a. percutaneous coronary intervention (PCI) b. stent placement 77 Revised 2/9/2016 c. atherectomy d. laser angioplasty 3. Observe pre, intra, and post procedure nursing interventions. 4. Assist with pre and post procedure assessment, VS, and pt. education (if appropriate and with supervision). Objectives for NURR 201 GI lab Spinout: 1. Observe preparation of patient for endoscopic procedures 2. Participate in preparation of patients under the direction of a licensed professional nurse 3. Observe endoscopic procedures 4. Observe and/or participate in the post-procedure care of patients 5. Describe some common complications encountered during endoscopic procedures and nursing interventions associated with each Objectives for NURR 201 Wound/Ostomy Spinout: 1. Review skin protocol at St. Luke’s Magic Valley Regional Medical Center 2. Demonstrate a proper skin assessment 3. Determine patient risk for skin breakdown using the Braden Score 4. Choose appropriate interventions for the nursing care plan (for specific skin issues) 5. Describe situations that would warrant a referral to the wound specialist 6. Perform dressing changes under the direct supervision of the wound ostomy certified RN (WOCN) Objectives for NURR 201 Diagnostic Imaging Spinout: 1. The student will identify the role of the Diagnostic Imaging (DI) nurse and participate and function as part of the DI team. 2. The student will perform and increase psychomotor nursing skills in the DI setting. 3. Student will observe the initiation of conscious sedation, and may participate in patient assessment and related documentation. This includes preparation for potential complications. 4. Student will identify connection between disease process and its presentation through radiologic imaging. Objectives for NURR 201 Preoperative and Postanesthesia Care Unit (PACU) Spinout: 1. The Registered Nurse will help students to learn through the following behaviors: A. Role modeling and demonstration. B. Direct teaching. C. Discuss organization, prioritization, delegation, self assessment and communication. 2. Expected student clinical behavior: A. Describe purpose and components of pre-op assessment. B. Discuss informed consent, pre-op teaching, and pre-op medications. C. Assess patients systematically under the direction of the RN (PACU) a. Define components of the initial post-anesthesia assessment. b. Verbal report by the anesthesia care provider 78 Revised 2/9/2016 D. E. F. G. H. I. J. K. c. ABC evaluation d. Oxygen therapy e. ECG monitoring f. Neurological and urinary system assessment Identify standards of care in the PACU. Discuss the PACU experience from the patient’s and family perspective. Discuss nurses’ ethical obligations to patients in the PACU. Identify non-pharmacological and pharmacological strategies to promote comfort and decrease anxiety. Identify normal heart rhythm, basic dysrhythmias and paced rhythms. Discuss invasive and noninvasive hemodynamic assessment. Explain etiology and nursing assessment and management of nausea and vomiting, pain, hypothermia, hypoxemia, and altered LOC. Discuss malignant hyperthermia protocol. http://www.medstudents.com.br/anest/anest1.htm Objectives for NURR 201 Cancer Center Spinout: 1. Review history for two cancer center patients and identify goals for cancer therapy. 2. Outline modalities for the cancer treatment of one cancer patient. A. Surgery a. diagnostic b. staging c. curative, palliative, reconstructive, preventative B. Chemotherapy a. vascular access b. side effects of chemotherapeutic agents c. procedure for extravasation C. Radiation a. external beam b. implant therapy (brachytherapy, closed therapy, sealed) 3. Identify essential elements of radiation and chemotherapy safety precautions. 79 Revised 2/9/2016 CRITERIA FOR CLINICAL JOURNAL TEMPLATE Name Date Clinical day Please submit a journal entry after each clinical day. Entries for students in Mon./Wed clinicals are due at 1800 on the day following each clinical day. Students who are in Fri./Sat. clinicals have journal entries due for both clinical days by 1800 on Monday. Attached to each assignment is a journal template which you will complete after each clinical day, save, and then send electronically through Blackboard to your instructor. You will notice an exclamation point in the grade book after submitting your assignment. Once your clinical instructor responds to your entry you will see a “0” in the grade book. Click on the “0” to view your instructor comments. Please print a copy of your entry and your instructor’s comments and include in a notebook for review at your final evaluation. _______________________________________________________________________ 1. Describe your feelings about: a. Strengths and areas for growth in your clinical performance. b. Clinical decisions made, nursing judgments, and possible alternate responses and interventions. What would you do differently? c. Critical thinking: Identify what could go wrong; what complications may occur? What assessments are made to determine if those complications are occurring? What nursing interventions will prevent the complication(s)? d. Submit at least one unanswered question related to your clinical experience this day, i.e., “I would like to know -------“ 2. Reflect on your utilization of learning experiences that day, including patient 80 Revised 2/9/2016 teaching completed. 3. Evaluation of your clinical goals each clinical day. 4. Identify three (3) goals for your next clinical day. a. Skill: b. Professional Development: c. Theoretical Application: 81 Revised 2/9/2016 Clinical Tally Sheet Patient Codes M – Medical S – Surgical P – Pediatric G - Geriatric Name _____________________________________ Course____________________________________ Rotation___________________________________ Agency____________________________________ Instructor Signature ________________________ PT. DATE CODE M/F AGE MEDICAL DIAGNOSES STUDENT ACTIVITIES 82 Revised 2/9/2016 MEDICATIONS GIVEN, ROUTES PATIENT TEACHING Name _________________________________ PT. DATE CODE M/F AGE MEDICAL DIAGNOSES STUDENT ACTIVITIES 83 Revised 2/9/2016 MEDICATIONS GIVEN, ROUTES PATIENT TEACHING Name _________________________________ PT. DATE CODE M/F AGE MEDICAL DIAGNOSES STUDENT ACTIVITIES 84 Revised 2/9/2016 MEDICATIONS GIVEN, ROUTES PATIENT TEACHING Checklist for signature forms to be turned in at the beginning of the semester Bring this checklist with the signed forms to your first day ________ Student handbook validation ________ Health insurance ________ Vehicle insurance ________ Clinical confidentiality form ________ Davita Dialysis confidentiality form ________ Drug/alcohol form 85 Revised 2/9/2016 COLLEGE OF SOUTHERN IDAHO ASSOCIATE DEGREE NURSING PROGRAM NURR 201 HANDBOOK VALIDATION THIS FORM MUST BE RETURNED TO THE CLINICAL INSTRUCTOR BY MONDAY, AUGUST 25, 2008 I have read the course requirements for NURR 201 and I understand the expectations. I understand that failure to meet course requirements will result in failure in the course and dismissal from the nursing program. ____________________________________________ Signature ___________________________________________ Date -------------------------------------------------------------------------I have reviewed the Student’s ADN Handbook, 2007-2008, and have also read the updated Policies in the current Student ADN Handbook, 2007 -2008. _____________________________________________ Signature __________________________________________ Date 86 Revised 2/9/2016 ___________________________________________________________________ Health Sciences and Human Services COLLEGE OF SOUTHERN IDAHO HEALTH SCIENCES AND HUMAN SERVICES HEALTH INSURANCE FORM I hereby show, by my signature, that I have health insurance in place at this time and that I will continue to keep this coverage in effect throughout this semester and until the completion of the Health Sciences and Human Services program in which I am currently enrolled ____________________________________________ Program of Study ___________________________ Signature of the Insured Student ___________________ Date 87 Revised 2/9/2016 VEHICLE LIABILITY INSURANCE FORM I hereby show, by my signature, that passengers, automobile and I (driver) are covered by liability insurance in an amount at least equal to that required by the laws of the State of Idaho. My signature also indicates that I have a valid driver’s license from the state of which I am a legal resident or of the State of Idaho. Student Signature______________________________________ Date ________________________________________________ 88 Revised 2/9/2016 ___________________________________________________________________ Health Sciences and Human Services CLINICAL CONFIDENTIALITY CONTRACT In order to uphold nursing’s legal and ethical responsibility to the confidential nature of the data contained in all patient records, electronic, paper, or otherwise and to prevent unauthorized access to hospital supplies, medications or information: I, _______________________________________(print name), will not divulge information about clients and/or their families that I am exposed to as a result of my position as a student. This would include, but is not limited to, information presented in classroom discussions, post-conferences, clinical practice, and agency visits. I may only divulge such information to fellow health care professionals as is necessary and useful to enhance delivery of care and education. I will omit client/agency identification data in all written work. In addition, as a condition to receiving a computer sign-on code and allowed access to a system in any agency, I agree to comply with the following terms and conditions. 1. 2. 3. 4. 5. My sign-on code is equivalent to my LEGAL SIGNATURE and I will not disclose this code to anyone or allow anyone to access the system using my sign-on code. I am responsible and accountable for all entries made and all retrievals accessed under my sign-on code, even if such action was made by me or by another due to my intentional or negligent act or omission. Any data available to me will be treated as confidential information. I will not attempt to learn or use another’s sign-on code. I will not use my sign-on code from CSI’s clinical education experience in my personal employment and vice versa. If I have reason to believe that the confidentiality of my sign-on code from my CSI clinical education experience has been compromised, I will immediately inform my clinical instructor. I will not leave a secured computer access application unattended while signed on. Any breach of confidentiality or unauthorized access is considered unsatisfactory clinical behavior and will result in a meeting with the clinical instructor, Course Coordinator and the ADN Chairperson and may result in dismissal from the program. Signature_______________________________________ Date_____________________ 89 Revised 2/9/2016 DIALYSIS CONFIDENTIAL INFORMATION AGREEMENT I understand the importance of preserving the confidential nature of the information of Total Renal Care, Inc. (“TRC”). This includes, but is not limited to, TRC’s data and records relative to business interests, computer systems and programs, projections, business plans, inventions, trade secrets, know-how, as well as information wherein TRC has an obligation of confidentiality to a third party and information concerning any patient, employee, physician, independent contractor, student, fellow or volunteer. I understand the necessity that such information not be compromised for any reason other than necessary business or medical communications and treatment needs. I further understand that patient information is confidential and not to be discussed with or disseminated to anyone, either inside or outside the company, except on an as-needed basis for the treatment of the individual, payment related thereto, or for TRC’s healthcare operations in compliance with federal and state regulations. Unauthorized dissemination may be a violation of federal and state laws. I am also aware and fully understand, that any violation of this Confidentiality Agreement is grounds for corrective action, up to and including immediate termination of employment or termination of any employment related contract or agreement between TRC and any of its subsidiaries and/or related organizations by which I am bound. Print Name__________________________________ Signature _________________ ___________ _________________ Company Name Date ___________ ________________________________________ Affiliation TRC Employee____ Employee____ Student____ Agency Volunteer____ Physician____ Medical Director____ Independent Contractor____ Attending Nephrology Fellow____ 90 Revised 2/9/2016 ACKNOWLEDGEMENT OF RECEIPT OF ALCOHOL/ DRUG POLICY AND AGREEMENT TO ABIDE BY THE POLICY I, ___________________________(print name) hereby acknowledge that I have received a copy of CSI’s HSHS Department Alcohol/Drug Policy for the Clinical/Practicum Site (referred to hereafter as the Policy) and acknowledge the following: I have read the Policy and have had the opportunity to ask questions about the Policy and the consequences for violating any terms of the Policy. I understand that my compliance with all terms of the Policy is a condition of my remaining in the HSHS Department Program, and I agree to abide by all terms of the Policy. I authorize the lab and/or Medical Review Officer or designee retained by CSI to release test result information to the HSHS Dean or his/her designee. ________________________________ Student’s Signature _________________________ Date ________________________________ Parent’s Signature if student is under 18 _________________________ Date WITNESSED BY: COLLEGE OF SOUTHERN IDAHO HSHS DEPARTMENT REPRESENTATIVE By________________________________ Date_________________________ 91 Revised 2/9/2016 CLINICAL EVALUATION The documentation of a student's clinical behaviors will be a summative evaluation completed at the end of each clinical rotation. This evaluation process will be completed by both the instructor and the student. If there are significant differences between the student and faculty evaluations, an attempt to compromise will be made, but the faculty's evaluation will stand. The clinical component of ADN education is designed to allow you, the student, to measure and achieve the level of competence necessary to meet the level and terminal objectives of the program and to be successful in your endeavors. This will require that you make yourself aware of the clinical requirements for each semester and implement behaviors which allow you to achieve these requirements. The evaluation tool uses a "satisfactory/unsatisfactory" rating scale. To provide consistency among faculty and students, the identification of each factor in the rating scale is as follows: U Unsafe performance Inaccurately performs S Able to perform: a. Identification of the patient/client. b. Communicates with patient/client about and/or during the care being demonstrated. c. Demonstrates procedure/knowledge accurately. d. Completes within a reasonable time frame. e. Cleans up appropriately. f. Documents and reports appropriately. g. Maintains role of AD student nurse. Successful completion of a semester requires the student achieve a satisfactory for each clinical behavior. Once an identified clinical behavior has been demonstrated and evaluated at a satisfactory level, it is expected that this behavior will continue in succeeding semesters at a satisfactory level. Should the student regress below satisfactory, a deficiency notice will be issued and a mutual plan made between the student and instructor to remedy the regression before the end of the semester. Deficiencies noted during the semester require a written plan of action be developed by the student and approved by the faculty member evaluating the student at that time. It is the responsibility of the student to share this written plan with the next clinical instructor. (See policy in ADN Student Handbook). 92 Revised 2/9/2016 College of Southern Idaho Associate Degree Nursing Program Clinical Evaluation Tool – NURR 201 Student Name_______________________ Clinical Instructor____________________________ Semester: _______________________________________ Clinical Site: ____________________________________ Wellness-Illness: Applies knowledge of position on wellness-illness continuum and utilizes the nursing process to problem solve, think critically, and make clinical judgments. Level/Program Objectives III. Assessment Unsatisfactory Performs a comprehensive nursing assessment through analysis of GFHP assessment data, physical assessment data, lab and other diagnostic data Evaluates for changes in health status and begins to identify complex needs Integrates the impact of developmental, emotional, cultural, religious, and spiritual influences on health status Assesses for changes in health status and identifies appropriate actions Analyzes patient’s response to interventions Assess discharge needs and ability to access community resources Evaluates patient’s response to medications VI. TeachingLearning IV. Clinical Decision-Making Recognizes trends in lab data and takes appropriate nursing action Assesses patient/support person(s) learning ability, barriers, motivation to learn, and learning needs prior to teachinglearning Implements steps in the teaching process in increasingly complex patients. Participates in meeting goals toward discharge planning Implements and evaluates teaching to patient’s identified at risk for complications Integrates the steps of the nursing process, evidence-based practice, and critical thinking in patient care 93 Revised 2/9/2016 Satisfactory Comments: Identifies pathophysiology of the medical surgical patient and relates to patient situation Integrates evidence-based practice, collected through technological resources and other modalities, in decisionmaking. With assistance, utilizes nursing process and critical thinking to prioritize and organize care for one or more patients Follows existing care plan to provide for continuity of care Seeks guidance in evaluation of care regimen outcomes With supervision, provides safe, evidence-based care. Caring: Integrates caring in the development of dynamic interpersonal relationships and implementation of nursing actions. Level/Program Objectives II. Communication Unsatisfactory Integrates cultural sensitivity throughout the nursing process Utilizes appropriate communication channels to report relevant assessment data Communicates relevant and complex information in a concise and clear manner to clients and healthcare team members Reports medication side effects or medication inaccuracies to appropriate member of the health care team and instructor in a timely manner Establishes therapeutic communication with patients V. Caring Interventions Utilizes verbal and nonverbal communication skills while establishing caring relationships Demonstrates intermediate computer literacy related to patient care. Demonstrates with minimal supervision the ability to perform procedures/skills based on facility guidelines Establishes and maintains caring relationships with patients/support person(s). Safely administers medication with minimal supervision 94 Revised 2/9/2016 Satisfactory Comments: Evaluates patient response to medications Maintains human dignity Provides developmentally appropriate nursing care Evaluates for physiological & psychological safety of patients Functions as a patient advocate Implements complex nursing interventions based upon patient assessment Unique Individual: Values unique aspects of all individuals, including self, and utilizes this awareness in all interactions within the healthcare environment. Level/Program Objectives I. Professional Behavior Unsatisfactory Accepts ethical/legal responsibility for own actions as expressed in ANA Code of Nursing Demonstrates self reflection by: Examining own ideas, feelings, and behaviors Recognizing and accepting learning potentials and limitations Evaluating own performance in a structured journal Accepts responsibility for nursing care given by self Maintains confidentiality of all healthcare information Functions, with minimal supervision, in the role of a professional nurse as a member of the healthcare team. Accurately documents nursing cares and procedures Utilizes self-reflection for continued growth in nursing practice. Demonstrates personal responsibility by: Arriving on time Informing both school and agency of absence/tardiness Adhering to school and agency dress code Following Student Handbook guidelines 95 Revised 2/9/2016 Satisfactory Comments: VII. Collaboration VIII. Managing Care Demonstrates honesty in: Documentation Performance of skills (meds, treatments, etc.) Interaction with others Clinical paperwork Identifies and recognizes roles and responsibilities of members of the health care team and collaborates with the team effectively Collaborates with patient/family in setting goals and evaluation Provides evidence-based, cost effective patient care Utilizes appropriate technology in provision of care Recognizes aspects of safe/unsafe environment Provides patient-centered nursing care Demonstrates beginning level of patient management, leadership, and organizational skills by: appropriate delegation, accepting responsibility and accountability for own actions, accepting accountability and responsibility for delegated nursing actions. With supervision, accepts legal/ethical responsibility for nursing care. Follows agency policy and procedures, functions within legal scope of a nursing student, shares pertinent information with agency staff and instructor Promotes the rehabilitation potential of the patient Maintains environment that supports patient independence Additional Comments: I have reviewed the contents of this evaluation and fully understand its implications. Student Signature: _______________________________________________________________ Date____________________ Clinical Instructor Signature: _______________________________________________________ Date____________________ 96 Revised 2/9/2016