PEM|BRS: GI & Metabolic Disorders Metabolic Disorders: Urea
advertisement

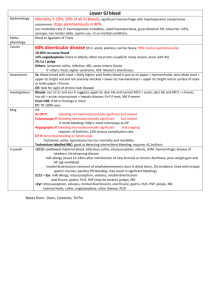
PEM|BRS: GI & Metabolic Disorders Metabolic Disorders: Urea Cycle Defect: OTC Deficiency (Ornithine Transcarbamylase Deficiency) X-linked so it affects males severely and females less severely Hallmark is severely high ammonia level in the absence of metabolic acidosis. Patients present with feeding problems and worsening encephalopathy as their ammonia levels continue to rise. Treatment with IV 10% arginine HCl can lower the ammonia level. The primary respiratory alkalosis with a compensatory metabolic acidosis is the RED FLAG for this; when present, draw an ammonia level, which will be quite high for this disorder (>100); therefore treatment is immediate dialysis if there is severe encephalopathy. Normal glucose, normal AG, and production of ketones Organic Acidemias: Propionic Acidemia (PA) pH: Low pCO2: Low HCO3-: Low Glucose: Low AG: Increased The organic acids inhibit the urea cycle, causing a secondary hyperammonemia Associated with significant ketosis (red flag!) Idiopathic Ketotic Hypoglycemia Most common cause of hypoglycemia in 1-5 year olds (not seen in older children due to their greater muscle mass and glycogen stores). Mild metabolic acidosis Increased AG Low glucose Ketones very high and out of proportion for an overnight fast Scrawny child who is a picky eater is a red flag when she cannot be aroused after an overnight fast during which she vomited a few times the prior evening and is found hypoglycemic and unresponsive. Prompt return to normal following administration of IV dextrose. If this occurs, no further workup is necessary—if repeated or hepatomegaly, needs further w/u. Tx: limiting fasting, and aggressive tx when vomiting; bed time snack 1 Fatty Acid Oxidation Defect: Medium-chain acyl-CoA dehydrogenase deficiency (MCAD) Red Flag: Hypoketotic hypoglycemia is NEVER normal beyond the neonatal period; you get more acidosis than would be expected for a few episodes of vomiting, yet there is no ketones. Metabolic Acidosis High AG Hypoglycemia No ketones in urine May have mild to moderate increase in ammonia but not the severe increase that urea cycle defects have. Associated with sudden infant death and Reye Syndrome like symptoms Abnormalities with the plasma acylcarnitine profile (increased acylcarnitine) are most helpful in establishing the diagnosis of MCAD. Tx: dietary fat restriction to avoid the build up of toxic metabolites. Oral carnitine replacement advocated (binds with FA to make acylcarnitine which can be excreted in urine instead of letting toxic FA’s build up). Diarrhea with bicarbonate wastage: bad diarrhea can cause acidosis with a normal anion gap. Galactosemia: An inborn error of metabolism caused by deficiency of the enzyme responsible for breakdown of galactose, which is a component of lactose (gal + glu = lactose). Patients can present in the early newborn period with GI symptoms, such as vomiting and diarrhea, lethargy, and FTT. On physical exam, hepatomegaly, lethargy, and cataracts are noted. Patients are also noted to have hyperbilirubinemia, initially indirect, then predominantly direct. Patients may be hypoglycemic on presentation but most notably have urine that is positive for reducing substances (galactose), while being negative for glucose. Patients will also have abnormal clotters and abnormal LFT’s. Patients with Galactosemia are at high risk for sepsis, especially due to E. coli, which poses the highest mortality risk in the acute phase of presentation. In the acute phase, with a lethargic infant, cultures should be drawn and antibiotics given. Hypoglycemia should also be treated. If clotters elevated, vitamin K and FFP may be given to the toxic appearing infant; avoid cow’s milk formulas (have gal)—use soy or elemental instead. The two most helpful studies in evaluating children for inborn errors of metabolism are a blood glucose and an ammonia level. A urinary test for reducing substances will detect lactose, fructose, galactose, pentose, and glucose. In the absence of urinary glucose, a positive test is suggestive of an inborn error of metabolism affecting the metabolism of one of those other sugars. 2 One inborn error of metabolism deserves special attention for ED physicians: glutaric aciduria type I. It may mimic nonaccidental trauma manifesting chronic subdural hemorrhages and retinal hemorrhages. A good screen is urine for organic acids. A child has bilateral frontal subdural fluid collections and a signal density and brightness most consistent with an acute hemorrhage in the high left parietal area. She had a minor fall—yet less force may be needed in the setting of chronic dilatation of the subdural space to cause bleeding from the bridging veins that can lead to an “acute on chronic” picture of the subdural collections. Whenever the history does not fit the findings on physical examination or the nature of the injuries discovered during the evaluation, nonaccidental injury must be considered. The CT findings shown for this girl may be consistent with “acute on chronic” abuse, but most children who have hypertonia in the setting of acute nonaccidental injury are not alert on examination. This should prompt the physician to consider a broader differential diagnosis, including inborn errors of metabolism. For this child, the subdural collections and clinical picture of increasing fussiness and increased tone are consistent with an acute decompensation in glutaric aciduria type 1 (GA1). GA1 is one of the organic acidurias that typically manifests later in infancy. Organic acidurias (also known as organic acidemias) are diagnosed by finding increased excretion of organic acids in the urine due to deficiencies in the metabolic pathways that are responsible for the breakdown of amino acids. Assessment of serum ammonia and urine organic acids is most helpful in diagnosing GA1. Most organic acidurias (eg, methylmalonic aciduria, propionic acidemia, and isovaleric acidemia) become evident in the neonatal period. Children who initially appear well at 1 to 2 weeks of age develop poor feeding, vomiting, hypotonia, and lethargy that may progress to coma. They develop a severe anion gap metabolic acidosis and may appear septic. Hyperammonemia, hypoglycemia, and electrolyte abnormalities due to volume depletion occur. Often, affected children have bone marrow suppression and may have pancytopenia. Intravenous fluid rehydration and the provision of adequate glucose to stop catabolism and sodium bicarbonate to correct acidosis should be provided. Treatment of the hyperammonemia with sodium benzoate, sodium phenylacetate, or intravenous arginine may be indicated. Consultation with a metabolic specialist is recommended. GA1 is caused by a deficiency in glutaryl-CoA dehydrogenase, which is required for the breakdown of lysine, hydroxylysine, and tryptophan. GA1 rarely presents in the newborn period. Affected children usually have an episode of decompensation characterized by ketoacidosis, hyperammonemia, hypoglycemia, and encephalopathy. Typically, the crises are triggered by an intercurrent illness, although there have been reports of episodes associated with or the diagnosis being made after a minor traumatic event. Children who have GA1 exhibit macrocephaly, and as many as 30% have subdural hemorrhages or effusions. Acute bleeding into the areas of subdural effusion may be mistaken for nonaccidental injury. In the absence of additional abuse findings (eg, 3 bruises, fractures) in a young infant, metabolic disorders need to be excluded. It is believed that the widening of the subdural spaces by the pre-existing effusion stretches the bridging veins and results in acute hemorrhages with relatively minor trauma. The most devastating manifestation of this disease is acute symmetric necrosis of the striatum and basal ganglia, which is irreversible and results in severe dystonia. Many, but not all, children have cognitive defects, and seizures are common. Over time, disease progression leads to further cerebral atrophy and a characteristic picture on central nervous system imaging of a marked widening of the Sylvian fissure and worsening subdural fluid collections (Fig. 2). Figure 2: Noncontrast CT scan shows progressive loss of cerebral volume, with marked increase in all cerebrospinal fluid-containing spaces. Changes are most notable at temporal lobes bilaterally. Reprinted with permission from Bergman I, Finegold D, Gartner JC Jr, et al. Acute profound dystonia in infants with glutaric acidemia. Pediatrics. 1989;83:228-234. Fluid and calorie restriction in children who have GA1 may worsen the metabolic crisis and hasten the onset of the necrosis within the basal ganglia and the accompanying dystonia. Intravenous fluids, appropriate glucose concentrations to stop catabolism, and treatment of hyperammonemia are indicated. Thorough evaluation for nonaccidental injury should be undertaken, but a broad differential diagnosis and consideration of other entities must not be omitted. Some children with acute exacerbations of inborn errors of metabolism will present to the ED with refractory seizures. These children typically have normal glucose and sodium. In addition to the normal Status Epilepticus protocol, the administration of IV pyridoxine and folinic acid may stop the seizure. 4 Lethargy in the newborn is a nonspecific sign that almost always indicates severe systemic illness and warrants a comprehensive evaluation. An inborn error of metabolism should be suspected when a previously well newborn deteriorates clinically within a few days of birth. The combination of respiratory alkalosis with normal glucose, electrolytes, and anion gap suggests a urea cycle disorder. Nitrogen, a waste product of peripheral (muscle) and enteral (dietary) protein breakdown, is converted into water-soluble urea for renal excretion by a complex metabolic pathway called the urea cycle. Hyperammonemia due to increased concentrations of nitrogen causes cerebral edema, central hyperventilation, and respiratory alkalosis, which are common early signs in newborns. Signs and symptoms of urea cycle defects are often nonspecific and can be confused with other systemic illnesses, such as sepsis, bacteremia, meningitis, metabolic abnormalities (dyselectrolytemia, hypoglycemia), and other inborn errors of metabolism. Most patients who have complete deficiency of enzymes present within 24 to 48 hours of initiation of feedings that provide the enteral protein load. As ammonia concentrations increase, patients develop poor feeding and vomiting, followed by increasing somnolence, lethargy, seizures, coma, and death. Those who have partial deficiency of the enzyme can present in late childhood or adulthood. Their presentation is characterized by episodes of hyperammonemia resulting in vomiting, mental confusion, ataxia, agitation, irritability, and combativeness, rarely progressing to seizures and coma. Hyperammonemia can also be seen in organic acidemias, fatty acid oxidation defects, and disorders of pyruvate metabolism. Patients who have organic acidemias exhibit metabolic acidosis or ketotic hypoglycemia; those who have fatty acid oxidation defects exhibit nonketotic hypoglycemia and present later in infancy. Pyruvate metabolic disorders are characterized by lactic acidemia and an elevated ammonia concentration. Other causes of hyperammonemia, including prematurity, dehydration, and liver failure, rarely result in plasma ammonia concentrations greater than 140 to 280 μg/dL (100 to 200 μmol/L). GI Disorders: Swallowed maternal blood is the most common cause of GI bleeding in neonates. This can occur either via ingestion of blood during delivery or while breast feeding— therefore, always ask about breast pain and nipple cracks/fissures. Many foreign bodies such as coins, thumbtacks, nails, and screws less than 5 cm in length that are found in the stomach or GI tract should be allowed to spontaneously pass through the GI tract and out the rectum. These are unlikely to have any complications. Anal fissures are commonly seen in children with constipation. The only treatment required is a stool softener, sitz baths, and application of protective ointment to the area (petroleum jelly). 5 A G-Tube originally placed 1-3 months ago that has become displaced has the complication risk of false passage of the GT when you try to replace it. If it has been over 3 months since placement, this is unlikely to be a problem. A patient with a caustic ingestion needs to be placed NPO, start an IV with normal saline, and admit for endoscopy to examine for possible mucosal burns to the esophagus. Any agents that can potentially cause emesis such as syrup of ipecac and activated charcoal are contraindicated because emesis of the caustic substance would cause further esophageal injury. An OG tube is contraindicated because of risk of perforation of an injured esophagus and subsequent mediastinitis. Administration of neutralizing agents would result in a damaging exothermic reaction and are therefore also contraindicated. Reye’s Syndrome: characterized by a recent viral illness followed by intractable vomiting, encephalopathy, and liver disease; strong association with aspirin. An elevated PT is common although DIC is not and patients rarely have clinical bleeding problems. Definitive diagnosis is made by liver biopsy. Serum glucose is low but bilirubin, ammonia, transaminases, and BUN are all high. Treat with dextrose infusion. Rectal prolapse is usually seen in children between 1-2 years of age. The most common predisposing condition seen with rectal prolapse is severe constipation. Of all the opiates, meperidine causes the least amount of spasms of the Sphincter of Oddi, and therefore is preferred for the treatment of pancreatitis. The metabolite of meperidine, normeperidine, is known to cause seizures in high concentrations. The most common cause of epistaxis is nose trauma from nose picking in toddlers. They may swallow the blood, have abdominal pain, and then vomit clots. With home births, vitamin K is often not given, putting the child at risk for hemorrhagic disease of the newborn, or Vitamin K deficiency bleeding (VKDB). This is also seen in exclusively breast fed infants since breast milk has low levels of vitamin K. The most common areas of bleeding are from the GI tract, umbilicus, mucous membranes, and circumcision and venipuncture sites. A prolonged PT is present but does not confirm VKDB. VKDB is confirmed if the bleeding ceases after Vitamin K administration. Related symptoms of pyloric stenosis besides projectile vomiting: associated gastritis will cause a brown or coffee brown appearance in the emesis. Patients may have decreased stools due to little food going into the intestines—parents may perceive this as constipation. Signs of dehydration may be present (lethargy, dry mucous membranes, decreased skin turgor, decreased urine output). Jaundice may be also seen which resolves after pyloromyotomy. The diagnosis of pyloric stenosis is confirmed with a pyloric ultrasound. Muscle thickness greater than 4 mm and a pyloric channel greater than 18 mm is diagnostic. 6 In patients exhibiting signs of midgut volvulus secondary to malrotation who are unstable with evidence of acute bowel obstruction, no contrast material should be given by mouth until the obstruction has resolved. In that clinical situation, an abdominal ultrasound will help confirm a midgut volvulus. In a stable patient without evidence of acute bowel obstruction, an upper GI series with small bowel follow through is the preferred study of choice to confirm the diagnosis. Lipase is more specific than amylase in diagnosing pancreatitis. Treatment is NG, NPO, and morphine. For pediatric liver transplant recipient patients, phone consultation with the transplant physician, a peds GI doc, or a peds ID doc is usually indicated; These patients have misleading presentations—i.e. fever does NOT accompany 40% of infections in liver transplant recipients; patients with even mild or subtle symptoms require full evaluation—i.e. mild abd pain may be an appy; mild headache may be meningitis! IBD: stress dose steroids should be considered in toxic appearing patients who are already taking prednisone. Fulminant Colitis and toxic megacolon can also be seen in patients with Crohn’s disease but are much less common than in UC. Pancreatitis and Biliary tract disease is more common in IBD patients. They are also at increased risk for thromboemboli and urolithiasis as well as ocular emergencies and urosepsis. Initial priorities in the management of hematochezia are to assess and preserve hemodynamic stability while attempting to localize the site of bleeding. Patients who present with mild signs and symptoms may be managed expectantly and in a stepwise fashion. However, patients who have significant hematochezia, such as the boy described in the vignette, require intravenous access, appropriate laboratory studies, and preparation for possible transfusion. At the same time, the clinician must localize the source of the bleeding to either the upper or lower gastrointestinal tract. A nasogastric tube should be passed and an aspirate obtained to determine if there is blood in the stomach. You may say a patient has no evidence of upper gastrointestinal bleeding, based on the nonbloody, heme-negative gastric aspirate. In this situation, the presence or absence of signs of intestinal obstruction (acute abdominal pain, vomiting, abdominal distention) helps to guide the ensuing diagnostic evaluation. The investigation of lower gastrointestinal bleeding is guided by patient age and clinical presentation. Intussusception and midgut volvulus are the most common causes of intestinal obstruction associated with lower gastrointestinal hemorrhage. If the bleeding is painless, and there are no signs of obstruction, the most common causes for lower gastrointestinal bleeding in a young child are Meckel diverticulum, juvenile polyps, vascular malformation of the gut, and infectious colitis. Inflammatory bowel disease (especially ulcerative colitis) also could have this type of presentation, but it would be unusual in young children, and brisk, painless lower gastrointestinal bleeding is an uncommon presentation of inflammatory bowel disease—more likely to be Meckel’s. Meckel diverticulum is present in 2% of the population at birth, but only 2% of affected 7 people ever have related symptoms. Usually the diverticulum is located about 50 to 75 cm (approximately 2 ft) proximal to the terminal ileum. The diagnostic radiology study of choice is a radionuclide scan, but the sensitivity of the test is decreased in the presence of brisk bleeding. The location of a Meckel diverticulum reduces the likelihood that endoscopic evaluation can determine the cause of bleeding or treat it. Accordingly, consultation with a gastroenterologist is unlikely be of immediate benefit. Of the foreign bodies that become lodged in the “normal” esophagus, approximately 70% become stuck at the level of the thoracic inlet, 15% become stuck in the midesophagus as the aortic arch crosses, and 15% are stopped at the lower esophageal sphincter. Round objects larger than 25 mm in diameter, linear objects longer than 5 to 6 cm, or objects that are sharp are less likely to pass spontaneously and often require removal. The choice of removal technique depends on how long the object has been lodged, the nature of the object, and the local expertise and preference. As mentioned, Foley catheter removal is preferred in some centers for smooth objects lodged high in the esophagus for a short duration of time. Esophageal bougienage, in which the foreign body is pushed into the stomach, is less popular, but has been advocated for coins lodged in the midesophagus or at the lower esophageal sphincter. The “penny pincher” technique, in which a specialized device for coin removal is introduced through a nasogastric tube and directly grasps the foreign body, is another alternative. However, none of the alternatives to endoscopy allow direct viewing of the esophagus. Approximately 40% of children who ingest foreign bodies are asymptomatic at presentation. The decision to proceed with imaging (posteroanterior and lateral view of the chest that includes the larynx, down to the stomach) frequently is based on the history of a choking or coughing episode or an eyewitness account of ingestion. If imaging reveals a smooth object at the level of the stomach or lower, expectant waiting is appropriate. Endoscopic removal is recommended for many sharp objects, especially straight pins, which have difficulty navigating the c loop of the duodenum and carry a risk of bowel perforation. Many authors recommend expectant waiting for round, smooth objects lodged for less than 24 hours in the esophagus because up to one third of these pass spontaneously, especially if they are in the lower esophagus. If left within the esophageal lumen, disc batteries can cause necrosis and ulceration. Therefore, immediate operative removal with flexible or rigid endoscopy is required. If the battery already has entered the stomach, it has a 90% chance of passing without intervention. Most authors recommend close follow-up with repeat radiographs in such patients to ensure passage of the battery. A girl has painless, bright red rectal bleeding in conjunction with or following bowel movements as well as a history of what may be prolapse of a perivaginal or perianal structure. The blood on rectal examination and the mother’s description of “something coming out of her bottom” suggest that tissue prolapsed through the rectum. This combination of findings strongly suggests acute prolapse of a juvenile colonic polyp 8 through the rectum followed by spontaneous reduction. The girl has no other risk factors for rectal prolapse, such as repeated episodes of increased intra-abdominal pressure (chronic constipation), acute or chronic diarrhea, parasitic infection, cystic fibrosis, or conditions predisposing to pelvic floor weakness, such as myelomeningocele. In addition, most rectal prolapse occurs in children younger than 4 years of age; an initial presentation at age 9 is highly unusual. Rarely, an ileocecal intussusception prolapses through the rectum, but it is less likely to reduce spontaneously. Polyps can act as lead points for intussusception, although the absence of pain and cramping makes intussusception extremely unlikely. A patient who has a prolapsed urethra should not have blood in the rectal vault, and spontaneous resolution of urethral prolapse is uncommon. Internal hemorrhoids are very rare in a child of this age and do not cause prolapse. Juvenile colonic polyps (also termed retention or inflammatory polyps) are erythematous, friable, pedunculated masses ranging in size from a few millimeters to 3 cm. Histologically, they are characterized by benign hamartomatous proliferation of mucusfilled glandular and stromal infiltrates. They are the most common type of childhood bowel tumor, with a peak incidence at 2 to 10 years of age and rare occurrences before the ages of 1 year or after 15 years. They usually present as solitary lesions, although two or more may occur in some children. In the absence of adenomatous changes on biopsy, such lesions are considered to have no malignant potential. The usual presentation is intermittent bright red, painless rectal bleeding accompanying or immediately following defecation. Bleeding usually stops spontaneously, and exsanguinating hemorrhage is rare. Iron deficiency anemia, although relatively common (30%), rarely is the chief complaint. Spontaneous infarction with self-amputation is common. Most polyps are located within 25 cm of the anus and, therefore, may be detected on digital rectal examination or barium enema. If prolapsed through the rectum at the time of examination, the examiner should manually reduce it with gentle pressure via a well-lubricated, gloved hand. Follow-up with a gastroenterologist for diagnosis by colonoscopy, with removal for pathologic confirmation, is required. Juvenile polyps occasionally recur. Juvenile Polyposis: Other conditions associated with painless rectal bleeding include juvenile polyposis (JP), an autosomal dominant disorder of multiple gastrointestinal tract polyps that sometimes is associated with other congenital anomalies. Twenty percent of cases result from sporadic mutation. In general, children who have JP have an increased risk of gastrointestinal malignancy, although the risk is low if two or fewer polyps are present and there is no family history of JP. Three or more polyps or a family history significantly increases the lifetime risk of malignancy. Every-other-year whole gastrointestinal tract screening with upper endoscopy, colonoscopy, and upper gastrointestinal tract contrast radiography and small bowel follow-through is recommended in such patients. Inactivating mutations causing interruption of cellular signaling of transforming growth factor-beta have been found in some afflicted families. Rarely, the entire gastrointestinal tract is involved; affected patients may present with 9 failure to thrive, malabsorption, anemia, and hypoalbuminemia. Peutz-Jeghers syndrome: Another rare autosomal dominant condition characterized by mucosal pigmentation of the lips and gums (deeply pigmented freckled lips) and hamartomas of the gastrointestinal tract. It has an incidence of 1 in 120,000; 50% of individuals have no affected family member. Extensive intestinal involvement is the rule, and disease is so widespread that removal of all hamartomas is not practical. Most gastrointestinal polyps occur in the jejunum and ileum, with fewer in the rectum, colon, stomach, and duodenum. Recurrent episodes of intussusception are common, especially involving the small bowel. Episodes of painful cramping suggest obstruction from small bowel intussusception. Patients who have Peutz-Jeghers syndrome have a 50% lifetime risk of gastrointestinal malignancy. Pancreatitis: The classic signs and symptoms include abdominal pain, nausea, vomiting, and midepigastric or upper quadrant pain that sometimes radiates to the back, shoulder, or flank. Although he does not have fever, 50% of patients who have pancreatitis may have lowgrade fever of less than 38.5°C. In addition, this boy is taking a medication known to trigger pancreatitis (Valproic acid). Individual measurement of serum amylase and lipase concentrations can yield false-negative and false-positive results in this clinical condition, but the combination has a reported sensitivity of 94% for detecting pancreatitis. Elevations in amylase can be seen in myriad disorders, including salivary gland pathology, other intra-abdominal pathology, or systemic illness. Lipase elevations are seen with perforated peptic ulcer and bone fracture with pulmonary fat embolism. A threshold of three times the normal values for amylase and lipase provides increased specificity, without a substantial impact on sensitivity. Aspartate aminotransferase and alanine aminotransferase are more nonspecific assessments than amylase and lipase; they can be elevated in a greater variety of conditions. Valproic acid causes pancreatitis idiosyncratically. CT scan does not need to be performed routinely in children who have typical mild pancreatitis. In complicated cases, magnetic resonance MRCP is being used increasingly for better imaging of the biliary and pancreatic ducts as well as looking for evidence of pseudocyst formation and anatomic abnormalities. Because of its higher rate of complications and greater invasiveness, endoscopic retrograde cholangiopancreatography (ERCP) now is reserved for cases that are believed to require therapeutic intervention, such as stone removal and sphincterotomy. In contrast to adults, in whom alcoholic pancreatitis is the leading cause, trauma (motor vehicle collision, bicycle handle, abuse) is the most common underlying cause of pancreatitis (14%) in children, closely followed by drug-induced (11%) and gallstoneassociated (11%). Familial pancreatitis, an autosomal dominant genetic disorder whose onset occurs from infancy to adolescence, accounts for approximately 5% of cases. Structural and mechanical disorders of the pancreas can cause acute pancreatitis but more 10 commonly cause chronic pancreatitis. They include ductal stenosis, pancreas divisum, choledochal cysts, and tumors. Pancreatic-sufficient cystic fibrosis is another cause of acute pancreatitis that has been described in children who have unrecognized cystic fibrosis and become dehydrated. Hyperparathyroidism leading to hypercalcemia as well as hypertriglyceridemia are other known triggers of pancreatic obstruction and acute pancreatitis. A wide variety of medications (corticosteroids, l-asparaginase, carbamazepine, valproic acid, isoniazid) and infectious illnesses (mumps, group B coxsackieviruses, Salmonella, hepatitis A and B, human immunodeficiency virus, influenza, and hemolytic-uremic syndrome-producing Escherichia coli strains) can precipitate pancreatitis. Parasitic and fungal infections are more common infectious causes worldwide. Many other systemic and autoimmune illnesses (lupus and periarteritis nodosa) also are associated with pancreatitis. Finally, idiopathic, which represents a group of as yet to be determined causes, comprises at least 25% of diagnoses in pediatric series. Among local complications are pseudocyst formation, with or without associated infection, and pancreatic abscess. Surgical intervention is a last resort and is indicated to drain abscesses and debride necrotic tissue. Adult scoring systems to predict severity in pancreatitis (Ranson, APACHE II) have limitations when applied to the pediatric population. Young age, high white blood cell count, high lactate dehydrogenase value at presentation, hypocalcemia, hyperglycemia, clinical shock, and low Pao2 all have been described as poor prognostic factors. Most children who have pancreatitis have a mild course that responds to gastrointestinal rest, pain control, and aggressive intravenous hydration. Gastric decompression with a nasogastric tube may be useful in cases where vomiting persists despite cessation of oral intake, although it is no longer standard in all cases. Although meperidine historically has been recommended over morphine for pain control in pancreatitis, all narcotics increase pancreatic sphincter wave frequency and biliary pressure to some extent. In the absence of comparative studies of pain control showing that morphine worsens the outcome in pancreatitis, and given the adverse effect profile of meperidine, many practitioners use morphine. Antibiotic therapy is not indicated in uncomplicated pancreatitis. Evidence is mixed for its benefit in cases of known necrotic pancreatitis without obvious infection. In the presence of abscess, infected pseudocyst, or shock and hyperpyrexia, a multidrug regimen such as ampicillin, gentamicin, and clindamycin is indicated. Acute Liver Failure: Acetaminophen is the most common drug-related cause of acute liver failure in the United States. Fulminant hepatic failure involves acute onset of severe liver injury associated with coagulopathy and encephalopathy in patients who do not have preexisting liver disease. The time from jaundice to encephalopathy after acute liver injury can be classified as hyperacute liver failure (0 to 1 week), acute liver failure (1 to 4 weeks), and subacute liver failure (4 to 12 weeks). Among young children, in whom encephalopathy may be absent or occur late in the process, the definition is based more on the development of coagulopathy from the liver injury. The liver failure can also be classified as fulminant or subfulminant, depending on the timing of jaundice to 11 development of encephalopathy, if present. In general, the time to onset of encephalopathy frequently is negatively correlated with outcome. The leading causes of death are cerebral edema, sepsis, and multiorgan failure. Acute liver failure is rare but very challenging; the course is variable and mortality is high. Overall, spontaneous recovery occurs in approximately 56% of children (10% to 60%, depending the cause), with 31% requiring transplant and 13% having a fatal course. Better outcomes are seen with acetaminophen poisoning, hepatitis A, and ischemia. Drug-induced acute liver failure, hepatitis B, and indeterminate causes have higher associated mortality rates. The causes for hepatic injury that leads to failure include viral infection (most common in developing countries) and drug exposures (most common in developed countries). Hepatitis A (fecal-oral route of transmission), hepatitis B (exposure to blood or body fluids), and hepatitis E (fecal-oral route of transmission) account for most viral cases. Hepatitis A frequently is more severe in adults than children, who may be asymptomatic. Hepatitis E is the most common cause of acute liver failure in parts of Asia, including China, India, and Pakistan. Other viruses can also be involved and include herpesvirus, Epstein-Barr, cytomegalovirus, and parvovirus B19. Up to 50% of cases in children do not have a specific cause identified. Drug-related liver injury is the second leading cause of acute hepatic failure, and acetaminophen is the most commonly implicated exposure in the United States, either by intentional or nonintentional overdose. The typical time sequence can be classified as hyperacute, with rapidly progressive multiorgan failure. Drug categories related to acute liver failure include nonsteroidal anti-inflammatory medications, statins, antibiotics, antiepileptics, and antituberculosis agents as well as a variety of other medications. Among the other causes of acute liver failure are heat stroke, protracted seizures, mushroom poisoning (Amanita phalloides), metabolic disease, ischemia associated with cardiac or septic events, autoimmune disorders, pregnancy, and malignancy. Inborn errors of metabolism and other inherited disorders should be considered in newborns and young children. Recurrence has been reported after acute liver failure in children who experience repeated acetaminophen overdoses. Care revolves around management of airway, breathing, and circulation; recognition and treatment of potential multiorgan failure with organ-specific therapy; cause-specific interventions where indicated (eg, N-acetylcysteine for acetaminophen toxicity, acyclovir for herpes-related diseases, penicillin and silibinin for Amanita poisoning); and treatment of cerebral edema/increased intracranial pressure. N-acetylcysteine has also been shown to be beneficial in patients with fulminant hepatic failure even in the absence of acetaminophen toxicitiy. Other nonspecific therapies include hypothermia, plasmapheresis, hepatic-assist devices, and liver transplant. Neurologic consequences can include encephalopathy, manifested by signs ranging from confusion to cerebral edema, intracranial hypertension, and coma. The pathogenesis is unclear but likely includes increased concentrations of circulating neurotoxins, such as ammonia. Ammonia is manufactured primarily in the small bowel and is converted to urea by a healthy liver. Reducing circulating ammonia concentrations may be helpful. Also, total body hypothermia may aid in slowing metabolism, decreasing ammonia 12 production, and reducing cerebral uptake. Other useful general therapies aim to reduce intracranial hypertension and sepsis, avoid hypo-osmolality and seizures, and maintain cerebral perfusion. Liver transplantation is a final treatment option, with country-specific selection criteria for qualification, including age, cause of injury, presence of cerebral edema, and extent of liver dysfunction (jaundice and coagulopathy). In addition to encephalopathy and liver-related findings, the clinical impact of acute liver failure can extend to injury to the lungs, heart, kidney, pancreas, and adrenal gland. The coagulopathy abnormalities seen with fulminant liver failure (decreased procoagulant and clotting factors, impaired fibrinolytic system, and decreased number and function of platelets) have multifactorial sources. Spontaneous bleeding is unusual (<5%), even with markedly abnormal clotting studies. Laboratory evaluation can include: complete blood count with platelet count and function as well as assessment of prothrombin time (International Normalized Ratio), antithrombin III, D-dimer, plasminogen, factors (VIII, V, VII), fibrinogen, von Willebrand factor, macroglobulin, and protein C and S. Specific laboratory analysis should be guided by gastrointestinal and hematologic consultation. If bleeding prophylaxis is desired due to coagulation profile abnormality or required due to active bleeding or preparation for invasive procedure, fresh frozen plasma, platelets, and cryoprecipitate can be considered, although potential fluid overload is a concern, as are cerebral edema, increased intracranial pressure, and potential hypersensitivity reactions. GI Bleeding: In general, the differential diagnosis of hematochezia in a toddler can be divided into conditions causing painful or painless rectal bleeding. Large-volume, painless rectal bleeding suggests a specific, localizable lesion. The most common causes of such painless rectal bleeding in children are Meckel diverticulum and colonic juvenile polyps. Among the less common causes are hemangiomas and venous malformations. A child who has Meckel diverticulum typically presents acutely, with large-volume (>30 mL) rectal bleeding that may require transfusion, as noted in this child, who demonstrates tachycardia, pallor, and anemia. If a Meckel diverticulum is suspected, a technetium 99m pertechnetate scan identifies the lesion in approximately 80% to 90% of cases. Once confirmed, the definitive treatment is exploratory laparotomy for surgical excision of the lesion. Colonic polyps present commonly with a history of intermittent small-volume (<5 mL) rectal bleeding. A patient who has rectal bleeding and negative results on 99mTcpertechnetate scan should undergo colonoscopy to evaluate for colitis or polyps. Ultrasonography is most useful if intussuception is suspected. Intussuception typically presents with crampy abdominal pain, emesis, currant jelly stools (representing smallvolume rectal bleeding from intestinal ischemia), and an abdominal mass. Nasogastric tube placement can aid in the diagnosis and treatment of upper gastrointestinal bleeding but usually is not indicated in the management of hematochezia. Meckel diverticulum is a persistent remnant of the omphalomesenteric duct that is identified in 2% of the population. A typical Meckel diverticulum is approximately 5 cm (2 in) long and located on the antimesenteric border of the ileum, approximately 60 cm (2 13 ft) from the ileocecal valve in the distal ileum and, thus, usually is seen in the right lower quadrant. These findings of Meckel diverticulum are commonly referred to as the "rule of twos." Approximately 5% of affected individuals experience complications. The most common presentation in children younger than age 4 years is painless rectal bleeding due to ectopic gastric mucosa. The ectopic mucosa may secrete acid, which causes ulceration of the adjacent tissue and bleeding and may present as melena. Less common presentations include Meckel diverticulitis (which can mimic appendicitis), intestinal obstruction from intussusception or herniation, and rarely perforation from an ingested foreign body trapped in the diverticulum. Management of the Meckel diverticulum involves hemodynamic stabilization of the patient, followed by surgical resection. Nuclear medicine techniques are useful in investigating gastrointestinal bleeding, but they have limitations. Technetium 99m pertechnetate (Meckel scan) localizes within functional gastric mucus cells that usually are found within a Meckel diverticulum or intestinal duplication cyst. Such uptake can be enhanced with agents such as cimetidine, glucagon, and gastrin, which are administered before the study. False-positive results occur with ureteral obstruction, an inflammatory mass such as seen in Crohn disease, abscess, arteriovenous malformation, or intussusception. A negative scan result should not delay surgical intervention if bleeding from a Meckel diverticulum is strongly suspected clinically. Technetium 99m-labeled red cells, also called a “bleeding scan,” help to localize a lesion that bleeds intermittently or at a low rate (0.1 to 0.3 mL/min or 500 mL/day) and eludes endoscopic detection. Labeled red cells remain in circulation for up to 5 days, which allows detection of intermittent bleeding. This important feature precludes the use of other radionucleotide or angiographic tests during this period. In rare cases in which Meckel diverticulum is strongly suspected and the Meckel scan yields negative results, abdominal computed tomography scan, angiography, and exploratory laparoscopy are alternative diagnostic modalities. Treatment is surgical resection. Painful rectal bleeding suggests bowel inflammation (especially colitis) or bowel ischemia. The pain associated with colitis usually accompanies the bowel movement and is relieved by passage of stool. The most common causes of colitis are infection (eg, Salmonella, Shigella, Yersinia, Campylobacter, Escherichia coli, Clostridium difficile, and amoebae), and inflammatory bowel disease. In contrast, bowel pain associated with ischemia is crampy, severe, and independent of the bowel movement. Common causes of ischemic pain include vasculitides (eg, Henoch-Schönlein purpura) and intussuception. Although hemorrhoids and anal fissures can also cause painful rectal bleeding, such bleeding usually is trivial. Oral Rehydration Therapy: Several studies have noted that ORT is an effective therapy for rehydration of mild-tomoderate dehydration. Determination of the degree of dehydration has been reviewed by many authors and is summarized well in the 2010 clinical review by Colletti and associates. Prolonged capillary refill, abnormal skin turgor, and abnormal respiratory pattern were noted as the three best indicators of dehydration in the March 2009 Cochrane review of dehydration in infants and young children. The same review article 14 notes many barriers to effective use of ORT, including unfamiliarity with published guidelines, misperception of increased time needed, misperception that ORT is contraindicated with vomiting, and patient or physician preferences. ORT should continue for 4 to 6 hours, as tolerated by the patient or until adequate rehydration is achieved. Oral rehydration fluids typically contain sodium, potassium, chloride, carbohydrates, and a base, and they are commercially available. Commonly used beverages (eg, sports drinks, fruit juices) are not recommended for acute rehydration because they are hyponatremic and have high carbohydrate contents. Oral rehydration has many benefits for the patient experiencing mild or moderate dehydration due to diarrhea, including lower cost than intravenous (IV) rehydration and ease of use both inside and outside the hospital environment. The quantity and timing of fluid administration can be modified, based on patient need and demand. IV rehydration and shock resuscitation is indicated for patients who have severe signs or symptoms. An antiemetic may be considered for patients such as this boy. Much has been written about ondansetron and rehydration. Although the American Academy of Pediatrics (AAP) 1996 guidelines discouraged the use of antiemetics in children younger than 5 years of age due to adverse effects of medications used at that time, many clinicians now include ondansetron as a standard part of their rehydration process. Ondansetron has a lower adverse effect profile than traditional antiemetic medications and may be an advantageous adjunct to oral rehydration. As of 2011, the AAP has neither endorsed nor encouraged the use of ondansetron in children who have vomiting due to acute gastroenteritis. The latest statement from the AAP on this subject was to endorse the 2003 recommendations published by the Centers for Disease Control and Prevention in Morbidity and Mortality Weekly Report. The authors state that “antiemetics are usually unnecessary” and that “cost-effective analysis should be undertaken before routine pharmacologic therapy is recommended” for vomiting due to gastroenteritis. Approximately 1.5 to 3.7 million pediatric outpatient visits in the United States are due to diarrhea-related issues, with 150,000 to 200,000 children requiring hospitalization and 200 deaths per year. The cost of care for affected patients exceeds $2 billion annually. Despite the potential severity, most children present with mild or moderate dehydration, and oral rehydration is sufficient. The process, however, is time-consuming and requires a competent caregiver who can spend a significant amount of time providing incremental amounts of fluid. Oral rehydration has been shown to be efficacious in both high- and low-income populations. The 2009 Cochrane review of 17 trials compared oral and IV rehydration and involved 1,811 participants, 56% of whom were randomized to oral rehydration. Although IV rehydration was slightly favored for rehydration or maintenance of hydration, the risk difference was only 4%. The failure rate for oral rehydration therapy was 4.9% compared with 1.9% for IV therapy. Where analyzed, there were no statistical differences for weight gain at discharge, hyponatremia, hypernatremia, duration of dehydration, total fluid intake at 6 and 24 hours, or amount of sodium intake and sodium concentrations. Children who received ORT actually spent less time in the 15 hospital than those receiving IV therapy. One complication noted in the ORT groups was paralytic ileus. 16