Student version Corrected Case Report
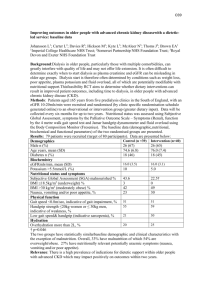
advertisement
Inpatient Multidisciplinary Rehabilitation Program for a Patient with Gait Abnormalities and Endurance Deficits Secondary to a Traumatic Brain Injury. Melissa Thorn Introduction Traumatic Brain Injury (TBI) is the most common cause of death for young adults and adolescences. It is defined as an external force causing brain dysfunction.1 It can be caused by a fall, motorized vehicle accident, or any other jarring or shaking of the head. Any of these accidents can cause bruising, bleeding, or swelling of the brain resulting in motor, cognitive, behavior and emotional deficits.2 Gait is a highly focused goal in rehabilitation due to the adverse effects associated with TBI. Some of gait abnormalities can include falls, decrease in endurance, and limited community access.2 Complications associated with gait abnormalities include various cognition deficits,decrease endurance and language barriers. Numerous studies have been done on gait with traumatic brain injury patients, however limited data and single aspect focus has been researched on the hip, knee, ankle, and center of mass has been researched.2 Working with a multidisciplinary team can help address cognitive deficits and get better results in therapy. Interpreters are present during therapy to provide needs; however the interpreters can affect the level of participation of the patient. The purpose of this case report is to describe a multiple disciplinary rehabilitation program for a patient with gait abnormalities and endurance deficits secondary to a traumatic brain injury. Case Description Patient The patient was a 44 year old Hispanic; right handed male who was involved in a motorized vehicle accident. The patient’s car was reported clipped by another car that resulted in the patient crashing into a wall. Patient was initially admitted to Utah Valley Regional Medical center. Severe traumatic brain injury insured from the injury with, right hemiparesis upper extremity greater the lower extremity and cognitive deficits. Following the motorized vehicle accident on arrival to emergency department, the patient represented with a 6 on the Glasgow Como Scale. Patient required intubation due to respiratory failure and underwent a tracheotomy and PEG placement five days post-surgery. Patient was transferred to university inpatient neurology rehabilitation unit two months later for an extensive rehabilitation program. Prior to his injury, the patient was an independent ambulatory and lived in a one story apartment with his wife and three children ages 23, 11, and 7. Examination The following examination was performed by the physical therapist day after admission to the inpatient rehabilitation unit, 47 days after his incident. Posture No deficits noted Sitting Balance Standing Balance Static sitting balance: Mod A Dynamic Sitting balance: Unable Sitting Balance Reactions: Delayed Patient requires min A to shift trunk anterior in w/c and unable to control posterior shift. Static Stand Time: 60 Sec Static Stand Assist: Total Assistance Range of Motion BLE: WFL, LUE: WFL, RUE: Not WFL Strength Patient unable to follow MMT LLE: Patient able to WB on LLE w/ assist and move LLE in antigravity at all joints. Strength overall >3/5. RLE: Patient demonstrates spontaneous hip flexion with return to bed and partial knee extension. LUE: Within Functional Limits (WFL) RUE: Not WFL Patient unable to tolerate standing and demonstrated poor balance and motor control making gait unsafe without multiple person assist in AM. Decrease endurance with activity Gait Activity Tolerance Sensation LUE: light touch Intact RUE: light touch impaired BLE: unable to fully assess due to cognition, sensation appeared intact to light touch in BLE and LUE. Pain Able to self-report pain symptoms. Tone Trunk Tone: Hypotonic LLE Tone: Normal RLE Tone: Hypotonic Not oriented to place, situation or time. Patient is appropriate, calm and cooperative. Cognition Mobility Skills Transfers Interventions Patient requires Max A. for rolling, supine<>sit, and scooting. Patient requires tactile cues for motor planning and initiation of rolling with transfers supine to sit EOB. Patient requires Mod A to maintain static sitting at EOB. Patient requires Max A for sit <> stand. Patient requires Max A with second person assist with squat pivot transfers in PM due to fatigue After examining the patient, the patient and physical therapist discussed the frequency of therapy and patient goals. The following short term and long term goals were discussed and agreed upon by both therapist and patient. Short Term Goals: To be met in 2 weeks. 1. Patient will transfer from bed to w/c w/ min A in 2 weeks. 2. Patient will static stand with min A >5 min and Mod A for dynamic standing in 2 weeks. 3. Patient will ambulate w/ total assist >50ft in 2 weeks. 4. Patient will maintain static sitting EOB w/ Min A in 2 weeks. Discharge/Long Term Goals: To be met in 4 weeks. 1. Patient will transfer from bed <>w/c w/ SBA in 4 weeks. 2. Patient will maintain static sitting and static standing w/ SBA >5 minutes in 4 weeks. 3. Patient will AMB w/ min A >150ft with Least Restrictive Assistive Device in 4 weeks. 4. Patient will ascend/descend a flight of stair w/ Min A and use of railing in 4 weeks. 5. Patient will be SBA for w/c mobility in 4 weeks. The patient was admitted to inpatient rehabilitation unit for intensive multidisciplinary therapy. Patient’s physical therapy sessions were twice daily for 45 minute sessions each, 6 days a week. The initial plan of treatment was set by the physical therapist consisting of balance training, basic activities of daily living, bed mobility, body weight support treadmill training, gait training, neuromuscular reeducation, pain management, patient and family education, posture/body mechanics training, stair training, therapeutic exercises, transfer training, and wheelchair assessment and management. Balance Training Balance training included sitting and standing balance. Patient initially demonstrated with Mod A for sitting balance due to hypotonic trunk tone and delayed sitting balance reactions. Patient initially required total assistance for static standing balance. Standing in parallel bars with a mirror in front for midline of patient was used for static standing balance, however patient demonstrated poor weight acceptance on to R LE. Sitting balance varied between contact guard assist and moderate assistance over the first few weeks. Fifteen days the patient had improved sitting balance to stand by assist for safety and verbal cuing during loss of balance. Training was progressed to dynamic sitting balance with upper and lower extremities performing activities. Over the length of patient’s stay in inpatient rehabilitation patient was able to progress to static standing balance using single point cane and contact guard assist for safety. Patient increased dynamic standing balance to minimal assistance by gradually increasing squats and emphasizing an eccentric control. Basic Activities of Daily Living Basic activities of daily living were addressed through Occupational Therapy.” Bed Mobility/ Transfer Training Bed mobility and transfer training included rolling, scooting, supine <>sit, sit<>stand, stand pivot transfers with w/c <>mat table and w/c<>bed. Patient initially required maximal assistance for bed mobility and maximal assistance by 2 person assist for squat pivot transfers. Patient was able to demonstrate supine to sit with minimal assist on right lower extremity within eight days due to patient responding to verbal and tactile cuing. By discharge, patient required minimum assistance for rolling, supine<>sit, and scooting. Patient still required verbal cues for motor planning and initiation for rolling with transfers supine to sit EOB. Body weight Support Treadmill Training Patient performed un-weighted treadmill training. Patient was unable to sequence movement patterns and maintain upright posture due to patient remaining flexed at hips. Patient was unsuccessful with intervention. The patient will benefit from continued physical therapy on this activity. Gait training Gait initially was unable to assess during evaluation due to patient being unable to tolerate standing and demonstrated poor balance and motor control. Gait training began with 2 hand assist with patient demonstrating a step to gait pattern w/ moderate assist from therapists. Patient was progressed to bilateral platform walker. Unfortunately the patient had difficulty time maintaining an upright posture therefore went back to 2 hand assist for 150ft with seated rests breaks as needed. Patient was able to progress to right forearm crutch for 150ft with moderate assistance and occasional minimal assistance from therapist due to loss of balance. Patient had trials to multiple assistive device techniques and training, however was unsuccessful and not pursued further. Patient required verbal cues for proper assistive device placement, foot placement, weight shifting, and sequencing. Depending on previous activities throughout the day would take effect on patient’s endurance tolerance to gait. Patient was able to progress and discharge home with single point can with minimal to moderate assistance for balance and sequencing. Neuromuscular Reeducation Patient demonstrated difficulty finding midline during static standing balance. Patient progressed to performing Nustep with right lower extremity strap on thigh to keep extremity in alignment. Focus of the activity was to promote reciprocal movement. Patient required verbal cues to keep midline posture and tactile cuing for alignment of right lower extremity without strap on right lower extremity. Patient performed quadruped with maximum assistance by two persons to maintain position and verbal cue for hip and lower extremity placement. Patient was able to accomplish task, however had sporadic involvement on proximal right hip. Patient was able to progress to tall kneel with two person assist to attain position and maximal verbal cueing. Patient required moderate assistance and maximum verbal cues to maintain tall kneeling. Patient continues to demonstrate proximal weakness and will benefit from continued therapy to increase functional mobility and gait pattern. Pain Management Nursing and medical staff managed patient’s pain; which enabled the patient to participate in therapy. Patient and Family Education Patient and family were educated on patient’s conditions throughout his stay in rehabilitation. Family participated in gait training and transfer training during therapy sessions. Family was not present during floor transfer and safety education one day prior to discharge. Patient has been referred to outpatient therapy to further improve patient’s independence and safety. Posture and Body Mechanics Training Training correlated with static sitting balance and posture. Stair Training Patient unable to perform stairs during initial evaluation due to original decrease in standing balance not being safe, however patient was able to perform prior to discharge. Patient demonstrated 12 stairs using left hand rail with contact guard to minimal assistance by 2 persons and moderate verbal cues to maintain safety. Patient demonstrated a step to gait pattern during stair training. Therapeutic Exercises Patient performed Nustep to increase lower extremity strength and encourage bilateral movement. Patient performed various lower extremity exercises to increase strength and improve patient’s functional mobility. Patient was able to demonstrate bridging on the nineteenth day, however patient required multiple verbal and tactile cues and had difficulty bringing right hip off the mat table. Patient required multiple rests between activities due to poor endurance and muscle fatigue. Wheelchair Assessment and Management Patient’s equipment; wheelchair and single point cane, issued and properly adjusted to patient prior to discharge. Outcomes The following table describes the patient’s status at time of discharge. The patient was discharged home with family and use of wheelchair for transportation and mobility. Patient was been referred to outpatient physical therapy for further progress. Posture Was addressed during static sitting and standing balance. No deficits were noted. Sitting Balance Static sitting balance: SBA Dynamic Sitting balance: SBA Sitting Balance Reactions: Minimal verbal cues Static Stand Time: 30 Sec , due to poor weight shift Standing Balance Range of Motion Strength Gait Stairs Static Stand Assist: using single point cane with contact guard assist. Dynamic Standing: Min Assist due to posterior loss of balance. BLE: WFL, LUE: WFL, RUE: Not WFL LLE. Patient demonstrated functional strength however was not retested at discharge. RLE: Patient demonstrated functional strength however was not retested at discharge. LUE: Within Functional Limits RUE: Not WFL Patient able to ambulate using single point cane or bilateral hand hold assist for 150 ft with contact guard assist to min assist by 2 persons, however patient requires moderate assist to recover from occasional loss of balance. Patient demonstrated 12 stairs using left hand rail with contact guard to min assist by 2 persons and moderate verbal cues to maintain safety. Patient demonstrated a step to gait pattern during stair training. Activity Tolerance Patient able to participate in therapy, however tolerance is limited due to physical and cognitive fatigue. Sensation LUE: light touch Intact RUE: light touch impaired BLE: unable to fully assess due to cognition, sensation appeared intact to light touch in BLE and LUE *Was not retested at discharge Pain Able to self-report pain symptoms. Tone Trunk Tone: Hypotonic L LE Tone: Normal R LE Tone: Hypotonic *Was not retested at discharge Patient was alert and orientated and able to answer questions appropriately. Cognition Mobility Skills Transfers Patient requires Min A. for rolling, supine<>sit, and scooting. Patient requires verbal cues for motor planning and initiation of rolling with transfers supine to sit EOB. Patient requires Min- mod A for sit <> stand with verbal and tactile cuing for weight shift to Right. Patient requires step up and verbal cues for sequencing with squat pivot transfers. Discussion The goals and outcomes after a traumatic brain injury (TBI) are highly variable depending on the patient and what part of the brain was affected. As physical therapists we are looking to improve a patients’ level of function and give them back their independence. The foundation for successful rehabilitation is an interdisciplinary team. No one person could possibly have the knowledge and skills necessary to treat all damaged aspects of the brain.3 Although we are concerned about cognition and behavioral issues associated with traumatic brain injury the physical therapists focus is on neuromuscular function by balance training, proprioception, gait training, strength training, transfer training, and education. Gait is a highly focused goal in rehabilitation due to the adverse effects associated with TBI. Some of gait abnormalities can include falls, decrease in endurance, and limited community access.2 In a recent study comparing time spent on gait during rehab with different impairment groups, it was found that TBI patients spent on average 17 minutes a day in gait training.4 With this amount of time being spent on gait are we addressing the gait abnormalities in TBI patients? There are a variety of gait abnormalities associated with TBI patients. Pelvic and trunk abnormalities have received little attention and are more prevalent than other gait patterns. 2 In providing treatments and interventions for patients, is important to address pelvic and trunk rotation during gait training. The patient in this case study worked on quadruped, tall kneel, ½ kneel, and bridging to increase core and pelvic strength. The most common gait abnormalities are related to trunk and pelvic movement and excessive knee flexion. There is limited research on what interventions strengthen proximal musculature and improve patient’s gait abnormalities. A patient with hemiparesis may require more intensive therapy focusing on the pelvic and trunk strengthening to improve the patients’ symmetry. The patient in this case report had hemiparesis on the left upper and lower extremity, however had decrease proximal stability and strength on left lower extremity during activities including gait. By incorporating proximal strengthening exercises to the treatment session, patient was able to decrease hip instability and improve gait pattern, however the patient still demonstrated poor endurance with gait training. Studies have shown that traumatic brain injuries result in reduced walking speeds, resulting in reduced cadence and shorter step length as well as wide base of support.2 A study by Mossberg found that endurance capacity and cardiorespiratory fitness in early TBI rehabilitation can help prevent co-morbidities. Colleagues studied individuals with TBI surviving more than one year and found they were more likely to die from cardiovascular conditions compared to general population. The cardiovascular system is a major long-term consequence of a TBI.5 The patient of this case study demonstrated decreased endurance and fatigued quickly. It was addressed by the patient performing the Nustep and by gait training. By providing him with physical activity at his maximal or submaximal capacities could have decreased his risk for co-morbidities and provided more endurance for activities of daily living. Cardiovascular activities should have been addressed and documented more efficiently for this patient. Further research is needed to properly asses the effectiveness of cardiorespiratory training with TBI. Studies have shown that by working with an interdisciplinary team will increase the outcomes in multiple areas. By increasing cognitive levels the patient will be able to respond better to physical therapy; nonetheless the patient for this case study had a language barrier creating more of a challenge for the therapists and the patient. An interpreter was present during sessions; however the patient demonstrated an increase response to therapy when a certain interpreter was present. The patient of this case study was willing to work and responded well to demonstration. This patient supported these findings by participating in proximal strengthening and cardiorespiratory conditioning addressing his gait abnormalities acquired after his traumatic brain injury. The patient was discharge to outpatient to continue improving his gait pattern and increasing functional mobility. Further research needs to be address to properly assess the interventions need to improve gait abnormalities in TBI patients. Conclusion Gait abnormalities acquired through traumatic brain injuries have wide variations. Pelvic, trunk, and endurance are just a few areas that require further research on what interventions will decrease gait abnormalities in traumatic brain injury patients. Many variables are to be considering during research with traumatic brain injury patients therefore making it difficult to know what interventions in pelvic, trunk and endurance are valuable. References 1. WebMD. Brain and nervous system health care. WebMD. http://www.webmd.com/brain/tc/traumatic-brain-injury-topic-overview. Published August 16, 2011. Accessed October 30, 2013. 2. Gavin Williams, Meg E. Morris, Anthony Schache, Paul R McCrory. Incidence of Gait Abnormalities after Traumatic Brain Injury. Archives of Physical Medicine and Rehabilitation. 2009; Vol. 90( Issue 4): Pages 587-593. 3. Susan B. O’Sullivan, Thomas J. Schmitz. Physical Rehabilitation 5th edition. Philiadelphia, PA: FA Davis Company; 2007 4. Gerben Dejong, Ching-Hui Hsieh, Koen Putman, Randall J. Smout, Horn and Wenqiang Tian. Physical Therapy Activites in Stroke, Knee Arthroplasty, and Traumatic Brain Injury Rehabilitation: Their Variations, Similarities, and Association with Functional Outcomes. Journal of the American Physical Therapy Association. 2011; 91:1826-1837. 5. Kurt A. Mossberg, William E. Amonette, Brent E. Masel. Endurance Training and Cardiorespiratory Conditioning after Traumatic Brain Injury. Journal Head Trauma Rehabilitation. 2010; 25(3); 173-183.