CALL 999
Health
Needs
Response
Booklet
Your Paediatric First Aiders are:
First Aid at Work :
Your school nurse is
You can contact her on
E-mail Address
Parent Responsibilities :
Inform the school or school nurse of changes in the Child’s Health or Treatment.
Supply the school with medical letters & medication within date and with a prescription label (Child’sname, amount of medication and method of administration).
School Responsibilities :
Annual training for identified staff.
Inform School nursing services of Child’s health needs or changes.
Update Booklet when informed of child’s health needs or changes.
Follow protocol for storage of medications on school site and during events off site.
Ensure staff aware of and have access to
Booklet
School Nursing Service :
Facilitate production of Booklet
Liaise with parents and schools
Review of medical information with parents and child as required.
Provide annual training for schools
Children with Asthma ANAPHYLAXIS
Mild to Moderate Reaction
Hives & Flushes
ACTION
Stay with child & CALL for help
GIVE ANTI HISTAMINE AS
Per PROTOCOL from consultant
Contact parent/carer
Watch for signs of anaphylaxis
SEVERE ALLERGIC
REACTION
Swelling of face or lips
Abdominal pain
Nausea, vomiting
Difficulty / noisy breathing swollen tongue
Swelling tightness of throat
Difficulty talking / hoarse voice
Give ADRENALINE auto injector
IMMEDIATELY
If difficulty breathing SIT
If collapsed raise legs
DO NOT STAND
Call 999 state ANAPHYLAXIS
If no improvement in 5 minutes give
SECOND ADRENALINE
AnaphylaxisCampaign
Children with Allergies/Anaphylaxis
ASTHMA
Symptoms
Coughing
Shortness of breath
Wheezing
Feeling tight in the chest
Being unusually quiet
Difficulty speaking in full sentences
Tummy ache (sometimes in younger children)
Give reliever (BLUE) Inhaler
Repeat up to 4 puffs (use spacer if prescribed)
Reassure child / adult to remain with child
SYMPTOMS RELIEVED
Yes
Return to school activities
Parent/Carer informed
No
Child/young person too breathless to talk
Lips blue
Distressed, gasping, struggling for breath
Unable to use inhaler
Decreased level of consciousness
CALL 999
If possible give reliever inhaler 1 puff/minute for 10 minutes
Encourage to sit upright / lean forward
Loosen clothing
Contact parents/carers
Asthma UK
Children with Sickle Cell
SEIZURE MANAGEMENT
Focal seizures:
Repetitive
Movements
Behaviour changes/ confusion
Unresponsive but may be conscious
Tonic / Clonic
Jerking & Rigidity
Unconscious
Incontinence
Atonic
Sudden drop
Absence::vacant may have facial twitching/rapideye movement
Maintain safe environment
Ensure safe position to prevent injury- move furniture not child.
If vomiting/ excessive saliva place head to side
Cushion head
Stay with child & observe and time seizure
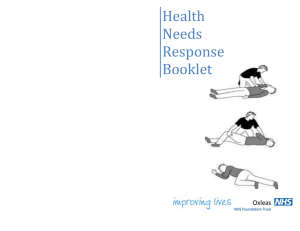
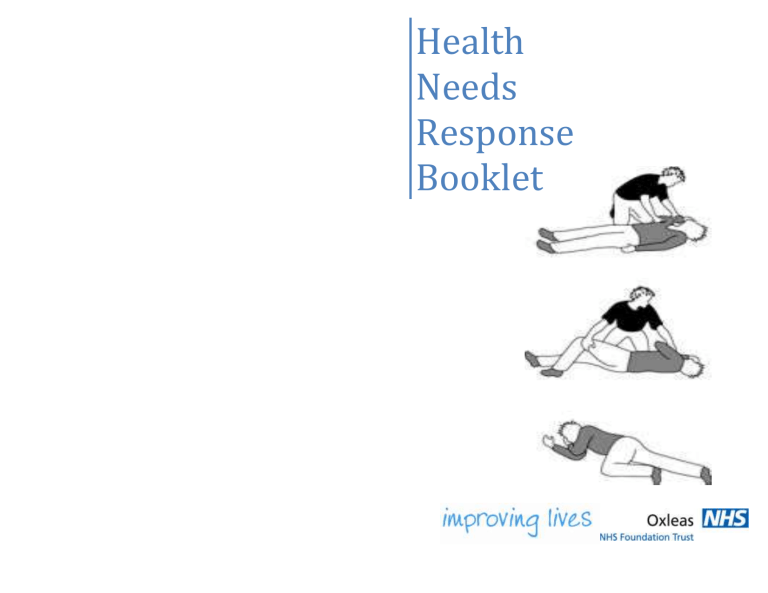
Put in recovery position after they stop shaking
Inform Parent/ Carer
Seizure lasts longer than5 minutes
NO YES
CALL 999
If Seizure does not respond to medication or 1st dose of buccal
If another seizure starts straight after the first
If breathing difficulties
If injured during seizure
If you are at all concerned
Inform Parent/ Carer
Monitor Recovery
If prescribed Administer
BuccalMidazalom as per protocol
As seizure stops put on side or into recovery position
Stay with child until they recover.
Reassure child and record time of seizure and medication administration
Inform Parent/carer.
Children with Seizures
SICKLE CELL
Daily Considerations
Access to water
Child kept warm and dry
Participation in PE determined by temperature extremes, individual tolerance and pain
If tired allow rest
Frequent Access to toilet
Guide for mild to moderate
Pain / Tiredness
Pain relief if prescribed
Rest and fluids
Keep child warm & comfortable
Inform parent / carer
Urgent Medical Response required if:
Breathless
Chest Pain
Abdominal pain
Drowsy
Severe headache
Call 999
Inform parents
Children with Diabetes
Treatment for Hypoglycaemia (Low Blood Sugar)
MAIN CAUSES:
Missed, delayed or inadequate snacks/meals, more exercise/activity than planned, too much insulin
SYMPTOMS:
Hungry, Sweaty, Pale, Grumpy, Irritable,
Wobbly/Shaky, Tearful/Emotional,
Headache/Tummy ache, Mood Changes,
Glazed Eyes BLOOD GLUCOSE (BG)
LEVEL 4MMOL or BELOW
PUPILS MAY NOT SHOW ANY SIGNS
TREATING A HYPO
Blood glucose level
4mmols or below
URGENT ACTION IS
REQUIRED
DO NOT LEAVE
PUPIL ALONE
Can the pupil eat and drink independently ?
YES
TREATMENT:
1.
Pupil to have fast acting carbohydrates
(sugar) e.g.100 - 150mls of sugary drink or 3
- 5 glucose tablets e.g. Dextrose or Lucozade.
Check BG level after 10 minutes, if level has not risen- repeat.
2.
Always follow this with slow acting carbohydrates (starchy food) e.g. 2 x plain biscuits or next meal or snack if due.
3.
Retest blood sugar to ensure it is 4.1mmols or above after 30 minutes.
NO
If the pupil is conscious but needs help to eat or drink?
NO
YES
YES
Is the pupil unconscious? (can lead to seizures)
Further Treatment:
Pupil will need assistance
Give treatment as above. I pupil uncooperative but conscious use GLUCOGEL
Twist off lid Place dispenser tip in mouth and direct gel between the gum and both sides of the cheeks
Massage cheeks (externally) to aid absorption Give whole tube
(can be repeated) or continue with steps 1, 2, 3 above when pupil co-operating
IF CONDITION DETERIORATING
CALL
999
Recovery position Nil by mouth Stay with Pupil
Inform parent/carer