physician drugs
advertisement

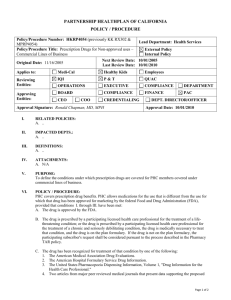
Chapter 25 The High Price of Prescription Drugs 1. Prescription drug expenditures are increasing faster than other medical expenditures (see slide) Expenditures growing faster than prices indicate that use is increasing o An increase in the number of aged leads to more use (see slide) o An increase in insurance coverage leads to more use (see slide) o Baby boom will continue upward trend o Out of pocket share is steadily declining (see slide) The replacement of older drugs by newer drugs is the most important reason for the increase in drug expenditures. o Innovative new drugs that cost more and have preventive and curative effects that result in greater use. o New “lifestyle” drugs have been developed that improve quality of life and can be taken for decades. 2. Are rising drug expenditures necessarily bad? No. Rising drug prices often reflect new and improved drugs. For example, there are new pain relievers to treat severe arthritis, but they cost $150 a month, nearly 20 times more than previous pain relievers. A new biotech drug, Enbrel, to treat rheumatoid arthritis can cost $1,500 a month. A greater number of prescriptions per person, particularly for the aged, may indicate that chronic diseases can be better managed and the aged can live longer with a higher quality of life. New drugs, although expensive, reduce nonpharmaceutical medical costs; for example, new antidepressants have reduced costly psychotherapy, and beta-blockers and blood pressure drugs have reduced the costs of cardiovascular-related hospital admissions and surgeries. 3. Is the high price of drugs determined by the high cost of developing a new drug? No. High research and development (R&D) costs are not the reason for high or rising drug prices. Large fixed or “sunk” costs are costs that have already been incurred; hence they are not relevant for setting a drug’s price. Fixed costs must be recouped, however, or a firm will lose money. High prices of drugs are determined by their greater value relative to other drugs to treat the same disease. Only if a drug provides greater benefits than competitor drugs are insurers willing to pay a higher price for that drug. New drugs that aren’t better than existing ones can’t sell for more. Patent protection for new Rx drugs typically lasts 20, but since they’re usually granted prior to clinical trials, they usually last about 8-10 years after FDA approval. 4. Why do drug manufacturers charge different purchasers different prices for the same prescription drug? It is the ability to shift market share rather than just the volume purchased that drives discounts. Purchasers who are not price sensitive are charged higher prices than those who are. Large MCOs pay less because they’re more elastic demanders willing to switch all of their patients to a competitor drug. High prices to some is not intended to cross-subsidize losses to others. It’s simply a matter of the elasticity of demand. Not all large volume purchasers receive price discounts. o Retail pharmacies in total sell a large number of drugs, but they do not receive the same price discounts as do managed care plans. o MCOs receive larger discounts because of their willingness to switch patients from one drug to another (via their formulary). o Prescription Benefit Managers (PBMS) operating on behalf of health plans can also promote particular brand names which leads to large discounts. o Retail pharmacies pay the highest prices for their prescription drugs because they must carry all branded drugs. They cannot promote substitution between branded drugs because the physician may be prescribing according to a health plan’s formulary. Because the pharmacy cannot shift volume, the drug manufacturer has no need to give it a price discount. 5. What methods have managed care plans used to limit their enrollees’ drug costs? Drug costs have become health plans’ fastest increasing expense. In response to rising costs, MCOs have provided the patient with incentives to use less expensive drugs. o A three-tiered system is used: patients pay a small copayment for generic drugs, a higher copayment for prescription drugs on the HMO’s formulary (where the manufacturer gives a large discount), and a much higher copayment for branded drugs not on the health plan’s formulary. 6. How have drug firms changed their marketing strategy as a result of managed care? Previously, physicians decided the patient’s prescription drug, and drug manufacturers spent a great deal of money marketing directly to physicians. Managed care shifted the purchasing decision from the individual physician to the committee overseeing a managed care organization’s formulary. Physicians continue to be important in prescribing drugs to their patients, but PBMs and health plans determine which brand-name drugs the physician is able to prescribe and the prices paid for those drugs. To counteract the closed formularies, drug firms started direct-to-consumer advertising to generate consumer pressure on physicians to prescribe certain drugs. This advertising has proved very effective in increasing sales of advertised prescription drugs. o Drug companies claim the ads are meant to inform the patient and to stimulate a discussion between the patient and his or her physician. o Critics claim that the ads do not inform patients about who is most likely to benefit from that drug, possible side effects, or other treatment options.