ron Toxicity
advertisement
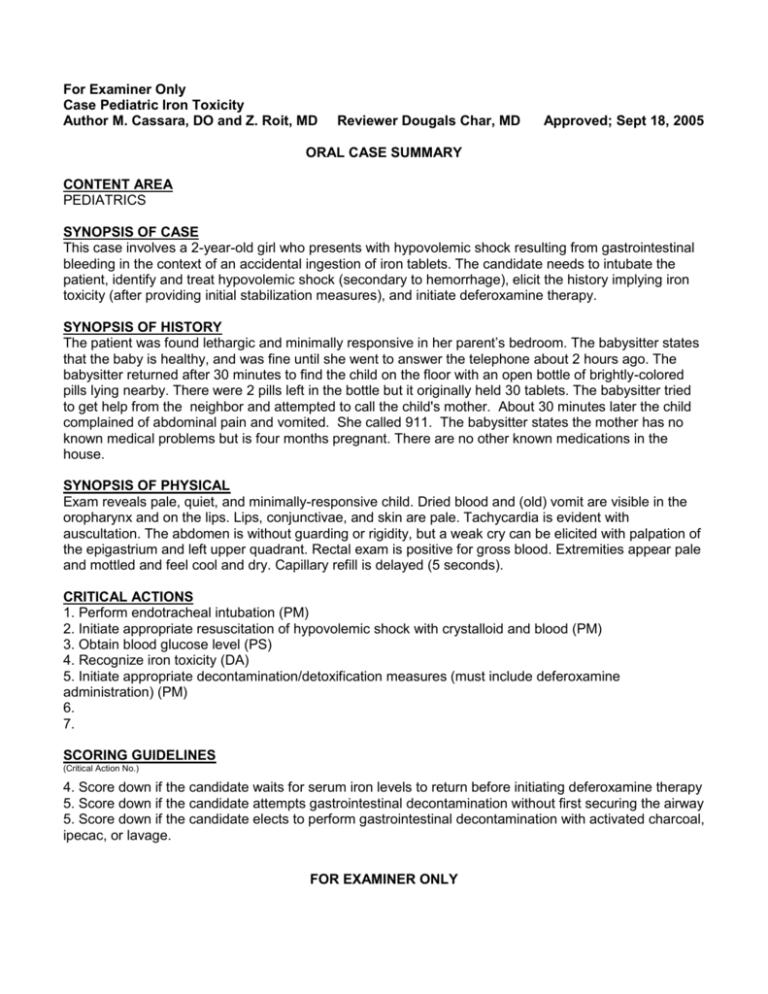
For Examiner Only Case Pediatric Iron Toxicity Author M. Cassara, DO and Z. Roit, MD Reviewer Dougals Char, MD Approved; Sept 18, 2005 ORAL CASE SUMMARY CONTENT AREA PEDIATRICS SYNOPSIS OF CASE This case involves a 2-year-old girl who presents with hypovolemic shock resulting from gastrointestinal bleeding in the context of an accidental ingestion of iron tablets. The candidate needs to intubate the patient, identify and treat hypovolemic shock (secondary to hemorrhage), elicit the history implying iron toxicity (after providing initial stabilization measures), and initiate deferoxamine therapy. SYNOPSIS OF HISTORY The patient was found lethargic and minimally responsive in her parent’s bedroom. The babysitter states that the baby is healthy, and was fine until she went to answer the telephone about 2 hours ago. The babysitter returned after 30 minutes to find the child on the floor with an open bottle of brightly-colored pills lying nearby. There were 2 pills left in the bottle but it originally held 30 tablets. The babysitter tried to get help from the neighbor and attempted to call the child's mother. About 30 minutes later the child complained of abdominal pain and vomited. She called 911. The babysitter states the mother has no known medical problems but is four months pregnant. There are no other known medications in the house. SYNOPSIS OF PHYSICAL Exam reveals pale, quiet, and minimally-responsive child. Dried blood and (old) vomit are visible in the oropharynx and on the lips. Lips, conjunctivae, and skin are pale. Tachycardia is evident with auscultation. The abdomen is without guarding or rigidity, but a weak cry can be elicited with palpation of the epigastrium and left upper quadrant. Rectal exam is positive for gross blood. Extremities appear pale and mottled and feel cool and dry. Capillary refill is delayed (5 seconds). CRITICAL ACTIONS 1. Perform endotracheal intubation (PM) 2. Initiate appropriate resuscitation of hypovolemic shock with crystalloid and blood (PM) 3. Obtain blood glucose level (PS) 4. Recognize iron toxicity (DA) 5. Initiate appropriate decontamination/detoxification measures (must include deferoxamine administration) (PM) 6. 7. SCORING GUIDELINES (Critical Action No.) 4. Score down if the candidate waits for serum iron levels to return before initiating deferoxamine therapy 5. Score down if the candidate attempts gastrointestinal decontamination without first securing the airway 5. Score down if the candidate elects to perform gastrointestinal decontamination with activated charcoal, ipecac, or lavage. FOR EXAMINER ONLY For Examiner Only Case Pediatric Iron Toxicity PLAY OF CASE GUIDELINES (Critical Action No.) 2. Resuscitation may be initiated by providing one or two 20 cc/kg crystalloid boluses intravenously prior to initiating 10 cc/kg boluses of blood. Administration of crystalloid alone does not meet the critical action. 3. The empiric administration of dextrose using the appropriate concentration and dose in an attempt to reverse this patient’s lethargy /mental status change will meet this critical action (4/5 exception) 5. If the candidate empirically initiates gastrointestinal decontamination in this patient without first securing the airway, the patient will vomit blood and aspirate. FOR EXAMINER ONLY For Examiner Only Case Pediatric Iron Toxicity Critical Actions 1. Perform endotracheal intubation (PM) This critical action is met by the candidate endotracheally intubating the patient Cueing Guideline: If candidate does not secure the airway, the patient will vomit blood and aspirate during the primary survey 2. Initiate appropriate resuscitation of hypovolemic shock with crystalloid and blood (PM) This critical action is met by the candidate administering at least one 20 cc/kg bolus of crystalloid fluid and at least one 10 cc/kg bolus of blood during this patient’s resuscitation Cueing Guideline: If candidate does not administer blood, and continues to administer only crystalloid fluids, the blood pressure will not improve 3. Obtain blood glucose level (PS) This critical action is met by the candidate obtaining a blood glucose level Cueing Guideline: 4. Recognize iron toxicity (DA) This critical action is met by the candidate when he or she identifies iron toxicity as a cause of the patient’s presentation, either, by recognizing the clinical toxidrome (gastrointestinal bleeding, nausea, vomiting, hematemesis, hematochezia, and hypovolemic shock), by acquiring the relevant history (pill fragments) from the babysitter, or by analyzing the results of laboratory test ordered. Cueing Guideline: 5. Initiate appropriate decontamination/detoxification measures (must include deferoxamine administration) (PM) This critical action is met by the candidate administering deferoxamine to the patient. The candidate may consider other methods of decontaminating the patient (i.e. whole bowel irrigation), but these other methods do not meet the critical action, and could complicate patient care and worsen the patient’s outcome. Cueing Guideline: 6. This critical action is met by Cueing Guideline: For Examiner Only Case Pediatric Iron Toxicity History Data Panel Age: 2 Sex: Female Name: Sidney Smith Method of Transportation: Ambulance Person giving information: Babysitter Presenting complaint: Found on the floor unconscious / minimally responsive by EMS Onset and Description of Complaint: The babysitter states that the baby is healthy, and was fine at at her normal baseline mental status and level of function. The babysitter then went to answer the telephone about 2 hours ago. When she returned after 30 minutes, the babysitter found the child on the floor with an open bottle of brightly-colored pills lying nearby. There were 2 pills left in the bottle but it originally held 30 tablets. She tried to call the child's mother and went over to the neighbors to get help. The child began to complian of abdominal pain about 30 minutes later and vomited once. The babysitter got scared and called 911. The babysitter states the mother has no known medical problems but is four months pregnant. There are no other known medications in the house. Past Medical History Allergies: none Medical: none Surgical: none Last Meal: unknown Habits Smoking: n/a Drugs: n/a Alcohol: n/a Family Medical History Father: none Mother: 4-months pregnant Siblings: none Social History Married: n/a Children: n/a Employed: n/a Education: n/a PMD: Dr. Kidd For Examiner Only Case Pediatric Iron Toxicity Physical Data Panel General Appearance: minimally-responsive, pale, lethargic girl Vital Signs: BP : P : R : T : O2Sat : Glucose : 40 / palp 180 / minute 32 / minute 37.5 C (rectal) 97% 100 per EMS Neurological: No focal or lateralizing signs, localizes painful stimuli Mental Status: Lethargic, minimally-responsive Head: Normal Eyes: PERRL, but slightly sluggish; EOM normal Ears: Normal Mouth: Dried blood and vomit in oropharynx; gag reflex intact; slight drooling Neck: Normal Skin: Cool and dry; mottled and pale; capillary refill = 5 seconds Chest: Tachypneic, but clear, breath sounds bilaterally (IF PATIENT HAS VOMITED WITH AN UNPROTECTED AIRWAY, crackles are present on the right) Heart: Tachycardic, without murmurs, rubs, or gallop Abdomen: Soft, non-distended, mild tenderness elicited with palpation of the epigastrium and left upper quadrant, no masses, no hepatosplenomegaly, no rigidity or guarding Extremities: Pale palms and soles; capillary refill = 5 seconds Rectal: Gross blood present (guaiac positive) Pelvic: Normal Back: No focal or lateralizing signs, localizes painful stimuli Other exam findings: WEIGHT = 12 kilograms For Examiner Only Case Pediatric Iron Toxicity Lab Data Panel Stimulus #2 – CBC WBC Hgb Hct Platelets Differential Segs Lymphs Monos Eos 15 /mm3 9 g/dL 21.3% 171/mm3 75% 20% 5% 1% Stimulus #3 – Chemistry Na+ 140 mEq/L K+ 4.2 mEq/L HCO3100 mEq/L Cl11 mEq/L Glucose 105 mg/dL BUN 40 mg/dL Creatinine 0.7 mg/dL Stimulus #5 – Arterial blood gas pH 7.27; pCO2 28 mm Hg; pO2 90 mm Hg; O2 Sat 96% Stimulus #6 – Serum iron and TIBC levels Iron level = 352 micrograms/dL; TIBC = 300 micrograms/dL Stimulus #7 – ASA and APAP levels: negative Stimulus #8 – Stimulus #9 – Stimulus #10 – Stimulus #11 – VERBAL REPORTS CXR = NORMAL Stimulus #4 – Urinalysis Color Yellow Sp Gravity 1.025 Glucose Negative Protein Negative Ketone Positive Leuk. Est. Negative Nitrite Negative WBC 0/HPF RBC 0/HPF AXR = RADIOPAQUE PILL FRAGMENTS SEEN IN STOMACH AND IN SMALL INTESTINE HEAD CT = NORMAL URINE TOXICOLOGY = UNAVAILABLE For Examiner Only Case Pediatric Iron Toxicity Stimulus Inventory Stimulus #1 – Emergency Admitting Form Stimulus #2 – CBC Stimulus #3 – Chemistry Stimulus #4 – Urinalysis Stimulus #5 – Stimulus #6 – Stimulus #7 – Stimulus #8 – Stimulus #9 – Stimulus #10 – Stimulus #11 – FOR EXAMINER ONLY Mock Oral Feedback Form – ABEM model Case Pediatric Iron Toxicity Date: Examiner: Examinee: Data acquisition Worst 1 NOTES 2 3 4 5 6 7 8 Best Problem solving Worst 1 NOTES 2 3 4 5 6 7 8 Best Patient management Worst 1 2 NOTES 3 4 5 6 7 8 Best Resource utilization Worst 1 2 NOTES 3 4 5 6 7 8 Best Health care provided Worst 1 2 NOTES 3 4 5 6 7 8 Best 4 5 6 7 8 Best Comprehension of path physiology Worst 1 2 3 4 NOTES 5 6 7 8 Best Clinical competence (overall) Worst 1 2 3 NOTES 5 6 7 8 Best Patient Interpersonal relations Worst 1 2 3 NOTES 4 Critical Actions Dangerous actions 1. Perform endotracheal intubation (PM) and omissions 2. Initiate appropriate resuscitation of hypovolemic shock with crystalloid and blood (PM) 3. Obtain blood glucose level (PS) 4. Recognize iron toxicity (DA) 5. Initiate appropriate decontamination/detoxification measures (must include deferoxamine administration) (PM) 6. 7. FOR EXAMINER ONLY Mock Oral Feedback Form – Core Competencies Case Pediatric Iron Toxicity Date: Does not meet expectations Examiner: Examinee: Meets Expectations Exceeds Expectations 1. Patient care 2. Medical knowledge 3. Interpersonal skills and communication 4. Professionalism 5. Practice-based learning and improvement 6. Systems-based practice Critical Actions Dangerous actions 1. Perform endotracheal intubation (PM) and omissions 2. Initiate appropriate resuscitation of hypovolemic shock with crystalloid and blood (PM) 3. Obtain blood glucose level (PS) 4. Recognize iron toxicity (DA) 5. Initiate appropriate decontamination/detoxification measures (must include deferoxamine administration) (PM) 6. 7. FOR EXAMINER ONLY Stimulus #1 ABEM General Hospital Emergency Admitting Form Name : Sidney Smith Age :2 Sex : Female Method of Transportation : Ambulance Person giving information : Babysitter Presenting complaint : Found on the floor unconscious / minimally responsive Background: Found on the floor unconscious / minimally responsive Vital Signs BP: 40 / palp P: 180 / minute R: 32 / minute T: 37.5 C (rectal) Stimulus #2 – CBC WBC Hgb Hct Platelets Differential Segs Lymphs Monos Eos 15 /mm3 9 g/dL 21.3% 171/mm3 75% 20% 5% 1% Stimulus #3 – Chemistry Na+ 140 mEq/L K+ 4.2 mEq/L HCO3100 mEq/L Cl11 mEq/L Glucose 100 mg/dL BUN 40 mg/dL Creatinine 0.7 mg/dL Stimulus #4 – Urinalysis Color Yellow Sp Gravity 1.025 Glucose Negative Protein Negative Ketone Positive Leuk. Est. Negative Nitrite Negative WBC 0/HPF RBC 0/HPF