AOCPMR-Journal-Club-October
advertisement
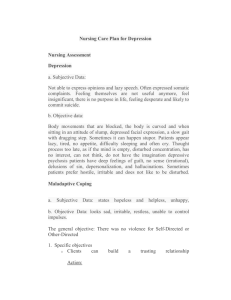
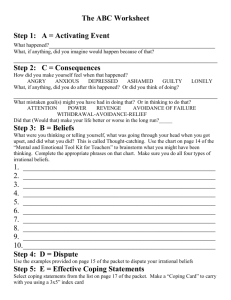
Journal Club October 2012 Brought to you by the AOCPMR Student Council Article title: CHANGES AFTER MULTIDISCIPLINARY PAIN TREATMENT IN PATIENT PAIN BELIEFS AND COPING ARE ASSOCIATED WITH CONCURRENT CHANGES IN PATIENT FUNCTIONING. Authors: Mark P. Jensen, Ph.D., Judith A. Turner, Ph.D., and Joan M. Romano, Ph.D. Journal/Source: Pain. 2007 September ; 131(1-2): 38-47 Discussion: Long-term disabling pain is an all-encompassing scenario. In addition to the physical issues, this study examined the potential impact/importance of pain-related beliefs and coping mechanisms in the overall treatment and care of the patient. This study examined 141 patients enrolled in a multidisciplinary pain program. A majority of the patients enrolled had been sufficiently injured that they had received pain-related disability compensation. Posttreatment outcomes, and 12-month follow-up outcomes were measured. Specific measures documented included beliefs, catastrophizing, and coping. Outcomes measured included depressive symptoms, physical disability, and pain intensity. Among the findings of the study, the most impactful was that patients better adapt at psychological coping had better overall outcomes. When combined with other recent research, the overall consistent theme that emerged was that the beliefs and coping strategies most associated with patient functional and psychological outcomes include: control over pain, guarding, resting, and catastrophizing. Importantly then, opportunity exists for clinicians to further investigate intervention into these areas post-pain-program-treatment. The study concluded that research into more effective means of improving patients coping mechanisms would likely improve the overall effectiveness of pain treatment, functional outcomes, and independence. 1 www.aocpmr.org Questions: 1. Although this study cannot be used to prove causality, what process variables were significantly associated with functioning and should be studied further as a point of intervention posttreatment? 2. What were the focuses of the treatments offered to the patients in the multidisciplinary program? What role does a physiatrist play in such a scenario? 3. What are the strengths and weaknesses of the outcome measure scales used in this study, such as the Roland-Morris Disability Questionnaire? Reviewer: Matthew J. Smith, OMS-II, Nova Southeastern University COM 2 www.aocpmr.org