COC SO 2013
advertisement
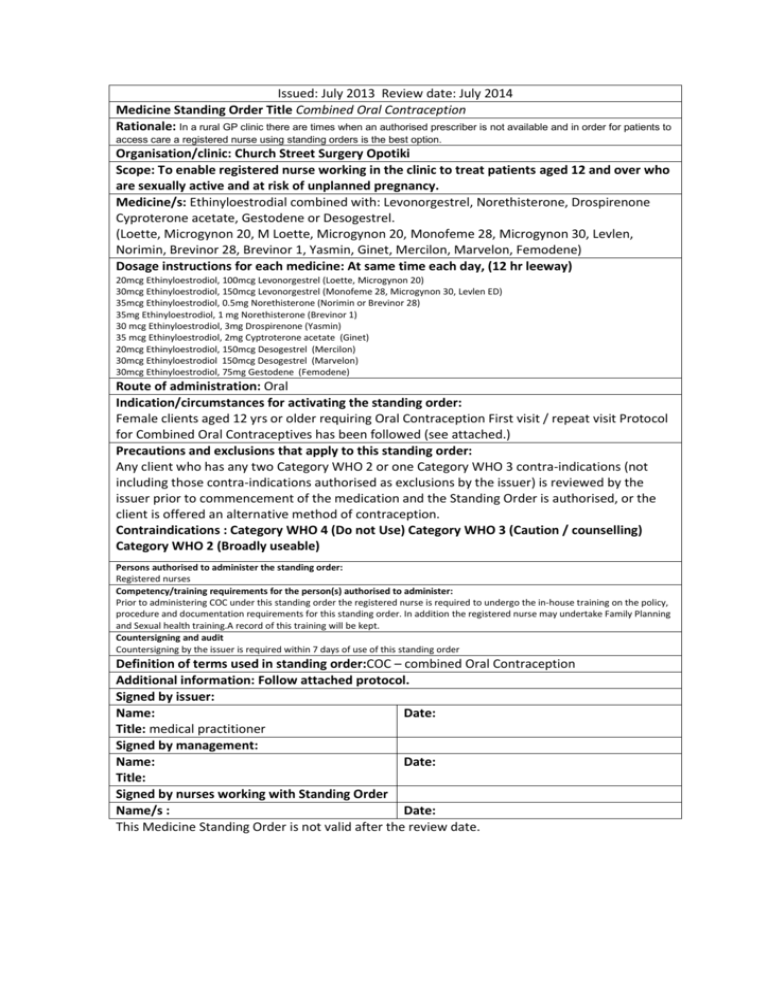
Issued: July 2013 Review date: July 2014 Medicine Standing Order Title Combined Oral Contraception Rationale: In a rural GP clinic there are times when an authorised prescriber is not available and in order for patients to access care a registered nurse using standing orders is the best option. Organisation/clinic: Church Street Surgery Opotiki Scope: To enable registered nurse working in the clinic to treat patients aged 12 and over who are sexually active and at risk of unplanned pregnancy. Medicine/s: Ethinyloestrodial combined with: Levonorgestrel, Norethisterone, Drospirenone Cyproterone acetate, Gestodene or Desogestrel. (Loette, Microgynon 20, M Loette, Microgynon 20, Monofeme 28, Microgynon 30, Levlen, Norimin, Brevinor 28, Brevinor 1, Yasmin, Ginet, Mercilon, Marvelon, Femodene) Dosage instructions for each medicine: At same time each day, (12 hr leeway) 20mcg Ethinyloestrodiol, 100mcg Levonorgestrel (Loette, Microgynon 20) 30mcg Ethinyloestrodiol, 150mcg Levonorgestrel (Monofeme 28, Microgynon 30, Levlen ED) 35mcg Ethinyloestrodiol, 0.5mg Norethisterone (Norimin or Brevinor 28) 35mg Ethinyloestrodiol, 1 mg Norethisterone (Brevinor 1) 30 mcg Ethinyloestrodiol, 3mg Drospirenone (Yasmin) 35 mcg Ethinyloestrodiol, 2mg Cyptroterone acetate (Ginet) 20mcg Ethinyloestrodiol, 150mcg Desogestrel (Mercilon) 30mcg Ethinyloestrodiol 150mcg Desogestrel (Marvelon) 30mcg Ethinyloestrodiol, 75mg Gestodene (Femodene) Route of administration: Oral Indication/circumstances for activating the standing order: Female clients aged 12 yrs or older requiring Oral Contraception First visit / repeat visit Protocol for Combined Oral Contraceptives has been followed (see attached.) Precautions and exclusions that apply to this standing order: Any client who has any two Category WHO 2 or one Category WHO 3 contra-indications (not including those contra-indications authorised as exclusions by the issuer) is reviewed by the issuer prior to commencement of the medication and the Standing Order is authorised, or the client is offered an alternative method of contraception. Contraindications : Category WHO 4 (Do not Use) Category WHO 3 (Caution / counselling) Category WHO 2 (Broadly useable) Persons authorised to administer the standing order: Registered nurses Competency/training requirements for the person(s) authorised to administer: Prior to administering COC under this standing order the registered nurse is required to undergo the in-house training on the policy, procedure and documentation requirements for this standing order. In addition the registered nurse may undertake Family Planning and Sexual health training.A record of this training will be kept. Countersigning and audit Countersigning by the issuer is required within 7 days of use of this standing order Definition of terms used in standing order:COC – combined Oral Contraception Additional information: Follow attached protocol. Signed by issuer: Name: Date: Title: medical practitioner Signed by management: Name: Date: Title: Signed by nurses working with Standing Order Name/s : Date: This Medicine Standing Order is not valid after the review date. Contra-indications table Cardiovascular disease WHO 2 VTE 1st degree relative 45+ years3 VTE in 2nd degree relative3 VTE 1st degree relative < 45 years +/precipitating factor (& client has normal clotting factors)3 After major surgery without prolonged immobilisation1,2 Ischaemic heart disease Migraines Migraine without aura < 35 yrs1 prior to commencing COC. WHO 3 WHO 4 1st degree <45 years + precipitating factor (& thrombophilia screen not available)3 Long term partial immobilisation. Wheelchair / debility3. Client has previous / current VTE2 FH VTE/thrombophilia 1st degree <45 years & client thrombophilia screen unavailable. FH VTE 1st degree relative < 45 years & client has abnormal thrombophilia screen. Client has prothrombotic abnormalities of coagulation / fibrinolysis Multiple risk factors for cardiovascular disease1,3 Severe or combined arterial and venous risks3 Major surgery (for 2 - 4weeks prior to 2 weeks post) with prolonged immobilisation Leg immobolisation3 High altitudes if other risk factor3 Amaurosis fugax (transient complete loss of vision)3 Known hyperlipidaemia and responding to treatment3 FH familial hyperlipidaemia or idiopathic event in 1st degree <45yrs & clients lipids not available 3 Personal past or present history of: Ischaemic heart disease, MI, TIA, angina, ATE disorder, CVA. Familial hyperlipidaemia – persistant despite treatment Migraine without aura ≥ 35 yrs prior to commencing COC. Migraine without aura < 35 yrs since commencing COC + one other arterial risk 3 Migraine with aura (any age) > 5 years ago2 Migraine with aura at any age. Migrianes without aura ≥35yrs since commencing COC . Migraine without aura lasting > 72 hours2 Aura no headache2 All migraines and taking ergotamine2 Contra-indications table WHO 2 WHO 3 WHO 4 Age (uk) < 35yrs and smoking any amount with no other risk factor2 ≥ 35 yrs and smoking < 15 a day2. - ≥ 35 yrs and one other risk factor / smoke ≥ 15 a day2 Weight 30 – 34 kg/m22 ≥35 – 392 ≥401 Smoking < 35 yrs + no other risk factor. < 35 yrs+ one other risk factor ≥ 35 yrs + smoking < 15 day. ≥ 35 yrs + smoking ≥ 15 day Smoking ≥40 day3 Hypertension Previous pregnancy related & now normal. BP regularly upper limit normal1 Previous hypertension and BP unmeasured (including pregnancy) Controlled (on meds) & BP measured and Normal Systoloc: 140-1592,3 Diastolic: 90-993 Systolic ≥1601,2,3 Diastolic ≥1001,2,3 Vascular disease3 Diabetes No vascular complications. With nephropathy, retinopathy, neuropathy or other vascular disease. Diabetes > 20 years. Structural Heart Disease Uncomplicated valvular heart disease Varicose veins History of superficial thrombophlebitis in lower limbs & no DVT3 - Current superficial thrombophlebitis in upper thigh3 Following VV surgery until dressings removed3 Liver & Gall Bladder Disease Pregnancy related cholestasis. Gallstones – asymptomatic or treated Gilberts disease3 Glandular fever > 3months ago with no complications Previous COC related cholestasis Mild cirrhosis. Symptomatic gall stones / gall bladder disease (current or medically treated). Other porphyria3 Cholestatic jaundice (COC related). Active liver disease(acute viral hepatitis, severe cirrhosis). Benign / malignant adenoma or hepatoma Acute hepatic porphyria3. During /after severe glandular fever or other viral hepatitis until 3 months after LFT's normal. Complicated valvular heart disease (with pulmonary hypertension,atrial fibrillation, previous SBE). Contra-indications table WHO 2 WHO 3 Serious condition affected by sex steroids/related to previous COC use WHO 4 Cholestatic jaundice, Chorea. Pancreatitis due to hyper-trigylceridaemia Pemphigoid (herpes) gestationis. Stevens-Johnson syndrome or erythema multiforme(if COC related). Trophoblastic disease – until HCG not detected3 Rheumatic Disease SLE +/- Severe thrombocytopenia or Immunosuppressive therapy1 Breast Disease First degree relative < 40 years had breast cancer. Benign breast disease. Undiagnosed breast lump occurring whilst on COC2 History, remission more than 5 years. Benign with epithelial atypia. Undiagnosed breast lump occurring on commencing COC2 Known carrier of BRCA1 mutation2 Current breast cancer or remission < 5 years. Premalignant epithelial atypia3 Pregnancy / Post Partum/ Breast feeding > 6 months post partum and breast feeding 6 wks to 6 months post partum & partial BF2 < 3 weeks post partum. Known pregnancy. 6 wks to 6 months post partum & primarily BF Breastfeeding < 6 weeks post partum Vaginal Bleeding Unexplained (pending evaluation). Chronic Systemic Diseases All others not listed in category 3. Sickle cell disease (trait WHO 1) Inflammatory bowel disease1,2 Chronic renal disease. Medications NNRTI1,2 En zyme inducing medication Ritonavir boosted protease inhibitor1,2 SLE + positive (or unknown) anti-phospholipid antibodies1 Ovarian, Cervical, Cancers. Endometrial Diseases Benign ovarian tumour. Abnormal smears during monitoring. CIN during and after treatment Miscellaneous Very severe depression worsened by COC3 Secondary Raynauds disease without lupus Hyperprolactinaemia3 GB only Past benign intracranial hypertension3 Haemolytic urameic syndrome3 Contra-indications table WHO 2 anticoagulant 2 WHO 3 WHO 4 Thrombocytopenic purpura3 Allergy to constituents. Secondary Raynauds disease with lupus anticoagulant2 combined oral contraceptive policy First Visit 1. Describe how COC works, failure rate, advantages/disadvantages. 2. Assess client suitability for COC and fully discuss risks and side effects. 3. - Check level of understanding, if in doubt do not issue medication, refer to doctor 4. Check History and exclude contraindications as per WHO tables above. 5. If there is a possible( relative) contraindication discuss on the day with doctor prior to commencing on alternative eg. POP 6. Check BP, height and weight & start on 2nd generation subsidised COC (currently either Levlen one tablet daily,or Norimin one tablet daily). Give script for 3 month supply from stock if available, information sheet VTE risk sheet, and condoms. Explain how to take pill and the 7day rule. Advise to continue with condom use in addition to the COC where acceptable. 7. Countersigning is to be completed by issuer (To be set for the doctor on Medtech task list) Subsequent visits 1. Check compliance and suitability - May change to alternative 2nd generation or a 3rd generation if having problems on initial pill choice and fully informed especially re thromboembolic risks. 2. Check no new contraindications 3. BP check first two visits and then annually. Weight check if indicated by complaint of weight gain or BMI is borderline ie. 28 4. Enquire if needs STI check and/or smear. 5. Check understanding of 7 day rule. 6. Give repeat script for 6 months. 7. Countersigning is to be completed by issuer (To be set for the doctor on Medtech task) combined oral contraceptive (COC) protocol Combined oral contraceptive checklist for commencement or continued supply of COC pill Describe how COC works Advantages -99% effective, convenient, regular periods usually lighter, not permanent, reduces risk or cancer of ovary and endometrium by 50%, may improve acne, PMT and iron deficiency anaemia Serious side effects Absolute contraindications - oestrogen dependent neoplasms - undiagnosed genital tract bleeding - BMI > 39 -pregnancy - Focal migraines ( with focal aura) - Hypertension (BP > 160/95 on repeat testing - History of venous thromboembolism (VTE) - Liver disorder/disease - Heart disease - Medications, rifampicin, griseofluvin, barbiturates, phenytoin, carbamazepine, primidone, topiramate, ritonavir - Acute pophria Check - BP, Height, Weight and BMI Pill start: - day 1 –3 of cycle – safe straight away - any other time – safe after 7 hormone pills – use condoms - Encourage client to discuss personal health and contraception needs with family/ caregiver/whānau esp. if under 16 yrs - Check level of understanding, if in doubt do not issue medication, refer to doctor. Oestrogen and Progestogen in pill stops ovaries from ripening Disadvantages -Remembering to take it, bleeding between periods, breast tenderness, nausea, headaches, sexual feelings, skin changes Chest pain(heart attack) Cough up blood (blood clot in lung) Breathless (blood clot in lung) Pain in the lower leg (blood clot) Severe headache (migraine, stroke) Possible (relative) contraindications Must see Medical Practitioner. From family history: - Heart disease – if primary relative <45 years (test fasting lipids) - VTE – if primary relative < 45 years - (test APC resistance, protein C, Protein S, Factor 5 Leyden) - Breast Cancer Enzyme inducing drugs - management by Medical Practitioner Also: - Cigarette smoking > 40/day - Diabetes mellitus - BMI 30 –39 - Prolonged immobilisation - St Johns Wort Start on 2nd Generation subsidised COC - Levlen, or Norimin 7 day rule: - use condoms until 7 hormone pills are taken, if you: miss two hormone pills, vomit within 3 hrs of taking hormone pill, diarrhoea, taking other medications eg. SJW - Provide client with FP information re: pill start if commencing on COC - Countersigning is to be completed by issuer (To be set for the doctor on Medtech)