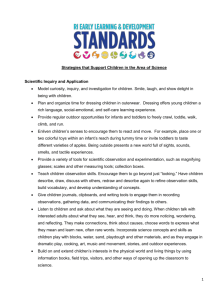
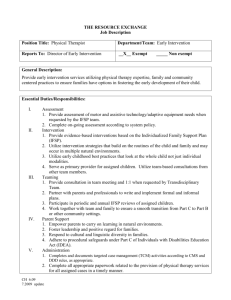
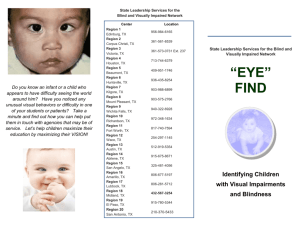
early intervention guidelines for infants and toddlers with visual
advertisement

Early Intervention Guidelines for Infants and Toddlers with Visual Impairment Fiscal Host: Zumbro Education District 801 Frontage Rd NW Byron, MN 55920 Contacts: Christian Wernau 507.775.2037 Kim Lucht 507.251.7925 Table of Contents INTRODUCTION 3 WHO ARE CHILDREN WITH VISUAL IMPAIRMENT 4 APPROPRIATE EVALUATIONS AND ASSESSMENTS 7 WHO CAN PROVIDE VISION SERVICES 10 WHAT ARE VISION SERVICES 11 RESOURCES 13 MNAPVI (MINNESOTA ASSOCIATION FOR PARENTS OF CHILDREN WITH VISUAL IMPAIRMENTS) MINNESOTA STATE ACADEMY FOR THE BLIND (MSAB) AMERICAN FOUNDATION FOR THE BLIND (NEW YORK, NEW YORK) BLIND BABIES FOUNDATION HADLEY SCHOOL FOR THE BLIND: THE PERKINS SCHOOL FOR THE BLIND NATIONAL BRAILLE PRESS TEXAS SCHOOL FOR THE BLIND AND VISUALLY IMPAIRED 13 13 13 13 13 13 13 13 APPENDIX A - ROLES AND RESPONSIBILITIES 14 SCREENING TOOLS 17 NEW MEXICO VISION SCREENING TOOL FAMILY INFANT TODDLER PROGRAM 19 19 APPENDIX B - TOOLS 24 SPECIAL EDUCATION SERVICES 25 APPENDIX C - MEDICAL TERMS TO LOOK FOR 40 APPENDIX D - CURRICULUM LETTERS 45 APPENDIX E LETTER REFERENCES 49 2 EARLY INTERVENTION GUIDELINES FOR INFANTS AND TODDLERS WITH VISUAL IMPAIRMENTS INTRODUCTION Minnesota Teachers of the Blind and Visually Impaired from Region 10, in implementing the Individuals with Disabilities Education Act (IDEA), Part C, is committed to providing quality early intervention services for infants and toddlers, ages birth to three, with disabilities and/or delays, including those with visual impairment. Toward that goal, and using the position paper of the Division of Visual Impairments, Council for Exceptional Children, titled: “Family-Centered Practices for Infants and Young Children with Visual Impairments” (2003) as a basis, we recommend the following guidelines: 1. Early intervention service providers have ongoing professional development to prepare them to screen for and identify risk factors or behavioral indicators of potential visual impairments. 2. When a medical doctor has identified a child, a Functional Vision Assessment may be conducted by a TBVI to identify educational needs and appropriate services for each eligible child, according to Part C requirements. 3. Vision services are delivered by, or with input from a Licensed Teacher of the Blind and Visually Impaired (TBVI). 4. Each local lead agency has a consulting relationship with a TBVI who participates on the IFSP team. Infants and toddlers with visual impairment have unique developmental needs. The following principles are infused throughout these guidelines for services that address these unique needs, and recognize that “vision services” must follow Part C criteria, policies, and procedures. (See helpmegrow) These guidelines are designed to assist families, local lead agencies, and early intervention service providers in providing services to infants and toddlers with a vision impairment. They describe children who qualify for services for students with vision impairments, describe evaluations and assessments that are appropriate for infants and toddlers with visual impairment, define what vision services are and who can deliver them, and assist early intervention teams in accessing those services. Table 1 Principles of Early Intervention for Infants and Toddlers with Vision Impairment 1. Early identification and diagnosis of vision impairment are essential. 2. Qualified professionals conduct ongoing vision evaluation, functional vision assessments, orientation and mobility evaluation, and early intervention. 3. Infants and toddlers with vision impairments and their families receive specialized early intervention services integrated into a program that promotes independence for the child within the context of family-centered, community-based activities. 4. The IFSP team assists the family in learning about the nature of their child’s vision impairment and its potential impact on their child’s development. EARLY INTERVENTION GUIDELINES FOR INFANTS AND TODDLERS WITH VISUAL IMPAIRMENTS 3 WHO ARE CHILDREN WITH VISUAL IMPAIRMENT The Minnesota State Department of Health reported 70,617 births in 2009. http://www.health.state.mn.us/divs/chs/annsum/09annsum/index.html. Based on the national prevalence of visual impairment (1.5 per 1,000 live births), the estimated number of infants with visual impairment born in Minnesota in the year 2009 alone is 105. Students meet Criteria in MN for BVI according the criteria in MN Statutes: https://www.revisor.leg.state.mn.us/rules/?id=3525.1345 It is also important to note that not all visual conditions qualify a child for early intervention (EI) services from a Teacher of the Blind and Visually Impaired (TBVI). Table 2 describes several visual problems that are often dealt with by medical procedures or therapies rather than through TBVI services. Table 3 lists the most common visual disorders that generally qualify an infant or toddler for EI services that may include consultation or direct vision services from a Teacher of the Blind and Visually Impaired (TBVI). This is not an exhaustive list. The need for vision services must be assessed on an individualized and ongoing basis. Please contact your TBVI to Discuss specific student needs. 4 EARLY INTERVENTION GUIDELINES FOR INFANTS AND TODDLERS WITH VISUAL IMPAIRMENTS Table 2 Visual Problems Treated Medically Note: These visual problems alone may not qualify an infant or toddler for early intervention services. However, EI service providers should be alert for these types of visual issues in infants and toddlers who are enrolled in early intervention for other developmental concerns. There are exceptionalities in individual cases. Contact your TBVI for more information. Visual Problem Description Treatment/Comments Strabismus Eyes turn inward, outward, or cross as a result of lack of muscle coordination or imbalance. If left untreated the weaker eye may develop suppression in order to avoid double vision, and amblyopia may result. Treatment may involve patching, eyeglasses, or surgery. In some cases optometric vision therapy may be an option. For infants and toddlers enrolled in EI for other concerns, the role of the early interventionist is to use good observation skills to alert parents of the need for evaluation and possible medical intervention. Refractive Errors: • Myopia • Hyperopia • Astigmatism Near sightedness - Far sightedness - Blurred vision is caused by an irregular curvature of the surface of the cornea or the internal focusing structures. Treatment is provided optically (with glasses). Again, for infants and toddlers enrolled in EI for other concerns, the role of the EI provider is to observe for possible refractive problems and alert the parents of the need for an eye evaluation. Eye Infections Eyes appear red, matted, and/or “gooey.” Symptoms may indicate infection or clogged tear duct and must be treated medically. Good hygiene is necessary to prevent spread of infection to other children. This is a short-term time-limited condition. Ptosis Eyelid droops. The child must be evaluated by an ophthalmologist. If the eyelid droops below the pupil, the child’s vision will be at least partially occluded. Ptosis may be a sign of more significant cranial nerve issues. EARLY INTERVENTION GUIDELINES FOR INFANTS AND TODDLERS WITH VISUAL IMPAIRMENTS 5 Table 3 Common Visual Disorders that Generally Qualify an Infant or Toddler for Vision Services Note: EI service providers should be alert for these terms in a child’s medical history or during interviews with parents and caregivers. (See the glossary for definitions.) If EI personnel encounter these terms or references they should contact their TBVI. Visual acuity of 20/60 or worse in the better eye Visual field loss reducing combined visual fields to 20° or less Albinism Aniridia Anophthalmia Aphakia Cataracts Cortical Vision Impairment (CVI) Familial Exudative Vitreo-retinopathy (FEVR) Glaucoma Leber’s amaurosis Microphthalmia Optic atrophy Optic nerve hypoplasia Papilledema Persistent Hyperplastic Primary Vitreous (PHPV) Phthisis bulbi Retinal detachment Retinopathy of prematurity (ROP), Grade 4 or 5 Septo-optic dysplasia CHARGE association (when accompanied by significant colobomas) Cytomegalovirus (CMV), if it results in vision loss Coloboma Delayed development of vision DeMorsier’s syndrome Down syndrome (with high myopia) Duane’s syndrome Nystagmus Ptosis Retinoblastoma Retinopathy of prematurity (ROP) Neurological Trauma, especially when an MRI indicates brain damage to the occipital lobe CVI Cortical Visual Impairment Periventricular Leukomalacia (PVL) If you have questions about whether a particular infant or toddler qualifies for vision services, ensure that referral is made to Help Me Grow *Pogrund, R., & Fazzi, D. (Eds.) (2002). Early focus: Working with young children who are blind or visually impaired and their families (2nd Ed.). NY: AFB Press, p. 14. 6 EARLY INTERVENTION GUIDELINES FOR INFANTS AND TODDLERS WITH VISUAL IMPAIRMENTS APPROPRIATE EVALUATIONS AND ASSESSMENTS What Are Appropriate Evaluations and Assessments for Infants and Toddlers with Visual Impairments? Infants and toddlers with visual impairment who have been referred to early intervention services need a comprehensive approach to evaluating and assessing their developmental needs, with input from a licensed TBVI. This approach must ensure that: a. Each developmental area is evaluated, i.e., cognition, physical (including vision, hearing, fine or gross motor), social-emotional, adaptive, and communication/ language, with appropriate adaptations made for specific items on the assessment tools that require vision to perform; and, b. A complete picture of the child’s visual status is gained in order to provide the information needed for development of the Individualized Family Service Plan (IFSP) and program planning. A complete evaluation or assessment for an infant or toddler with a visual impairment will address both of the above. It should include results of a functional vision assessment (FVA) and orientation and mobility evaluation, if appropriate, as well as the results of the medical/ophthalmologic evaluation that preceded them. Below are brief descriptions of five different procedures that are typically carried out with infants and toddlers prior to and following diagnosis of a visual impairment. These are: 1) medical ophthalmologic evaluation 2) functional vision assessment, 3) learning media assessment, 4) orientation and mobility evaluation, and 5) developmental evaluation and assessment. 1) Medical Ophthalmologic and Pediatric Optometric Evaluation The goal of the ophthalmologic evaluation is to diagnose and determine a treatment plan to preserve and enhance vision. This examination takes place in the ophthalmologist’s office. In its 2007 Policy Statement, the American Academy of Ophthalmology and the American Association for Pediatric Ophthalmology and Strabismus recommend an ophthalmological examination be performed whenever questions arise about the health of the visual system of a child of any age. *See Document at the end Important: Because of a higher incidence of vision impairments in children who are deaf or hard of hearing, infants and toddlers who have been diagnosed with a hearing loss should have a vision evaluation. EARLY INTERVENTION GUIDELINES FOR INFANTS AND TODDLERS WITH VISUAL IMPAIRMENTS 7 Pediatric Optometric Evaluation A pediatric optometric evaluation refers to the examination of children’s eyes by optometrists who are trained in evaluating and treating visual disorders in children. The vision examination by the pediatric optometrist includes evaluation of the child’s eye muscle movements, focusing skills, eye tracking and fixation skills, the ability of the eyes to aim, move and work together, visual behavior, and dilation of the eyes. The dilation of the eye allows the doctor to determine if there is a need for glasses even if the child is nonverbal. The dilation also allows the doctor to view the structures inside the eye to look for abnormalities of the retina or optic nerve. 2) Functional Vision Assessment Once an infant or toddler has been diagnosed with a visual impairment, completion of a functional vision assessment (FVA) is one of the primary roles of the teacher of the blind and visually impaired (TBVI). Medical documentation is required. The goal of the functional vision assessment, done in collaboration with the IFSP team, is to determine what and how the child sees, and what can be done to best facilitate learning through the visual sense. This assessment is accomplished in the child’s home, childcare facility, and/or other community setting and typically requires several visits over a period of time. During the child’s first years, functional vision assessments need to be reviewed several times. The information that is gathered from a FVA often is quite different from what is gathered from a clinical vision evaluation at a doctor’s office, in that it is not diagnosis or treatment oriented. The goal of a FVA is to determine the child’s visual strengths and needs, and to develop strategies for optimizing and/or promoting the use of visual and non-visual information in the broader developmental sense. The TBVI relies on the eye doctor’s findings to help determine adaptations that are indicated based on a child’s diagnosis. Appropriate team recommendations for early intervention services cannot be made without the information derived from the functional vision assessment. 3. Learning Media Assessment Formal learning media assessments typically are not done during the birth-to-three years; however, the process begins via observation of the infant/toddler’s preferred sensory mode (i.e., auditory, visual, tactual) and developing visual skills. By the time a child enters preschool, the team usually has a fair idea of how to support a child’s developing literacy. The following describes prerequisite skills for emergent Braille literacy in infants and toddlers with visual impairment. A similar skill area description exists for emergent print literacy skills for infants and toddlers who will read using large print or other accommodations. “Supporting early literacy development in early childhood settings such as the home and childcare; teaching early literacy skills and modeling techniques for fostering development of those skills in the home and childcare, such as reading aloud to the child, developing book concepts, encouraging early reading and writing skills (e.g., pretend reading, scribbling); working with parents and others to expand child’s experiential base and general concepts; developing hand/finger skills; helping parents and others acquire books, labels, and other materials in accessible media; helping parents acquire knowledge of Braille and resources for learning the Braille code; assuring models of proficient Braille readers; bridging emergent literacy to early formal Braille literacy.” Project SLATE (2003) 8 EARLY INTERVENTION GUIDELINES FOR INFANTS AND TODDLERS WITH VISUAL IMPAIRMENTS For children with visual impairment age three years and older, the decision on whether they will read print, Braille, or both is based on a systematic assessment process called a “learning media assessment” and is required by the Individuals with Disabilities Education Act (IDEA). It assumes that educational teams will provide for instruction in Braille literacy skills for a child who is blind or visually impaired unless a learning media assessment shows that Braille is not appropriate for the child. *From Project SLATE Research (2003). 4. Orientation and Mobility Evaluation The evaluation is done by a certified orientation and mobility specialist (COMS)(see Section IV). For infants and toddlers, the concept of orientation represents a developmental process of becoming aware of oneself as a separate being, where one is and wants to move in space, and how to get to that place. Mobility refers to general gross motor development, including the normal integration of reflexes, acquisition of motor milestones, refinement of quality-of-movement skills, and purposeful, self-initiated movement. For this age group, orientation and mobility is also a gradual process through which the basic concepts and skills of safe movement develop. An orientation and mobility evaluation is performed by interviewing the parents, collaborating with the team’s physical and occupational therapists, and directly observing and interacting with the child. In addition to overall developmental information, the O&M specialist is concerned with the child’s level of functional vision, hearing, tactile skills, and specific mobility skills. He or she also considers the natural learning opportunities presented to the child within the conditions of the assessment and their possible influence on the child’s observed performance. The scenario below describes how an orientation and mobility specialist might work with an early intervention team. *Pogrund, R., & Fazzi, D. (Eds.) (2002). Early focus: Working with young children who are blind or visually impaired and their families (2nd Ed.). NY: AFB Press, p. 395. 5. Developmental Evaluation and Assessment Collaboration between the early intervention service provider and the teacher of the visually impaired (TBVI) is important throughout the evaluation and assessment process. The TBVI can participate in two ways: (a) as a direct participant by assessing in his/her particular area of expertise, or (b) as a facilitator or consultant by observing testing to point out when the vision impairment affects the testing items or scoring, and to recommend modifications for the visual impairment. Evaluation and assessment tools usually are not designed for a child with a visual impairment. Children with visual impairments need special accommodations for assessment and evaluation. The use of standardized measures to determine a young child’s present level of functioning may not result in valid scores for the infant or toddler with a visual impairment. EARLY INTERVENTION GUIDELINES FOR INFANTS AND TODDLERS WITH VISUAL IMPAIRMENTS 9 WHO CAN PROVIDE VISION SERVICES When a vision impairment has been diagnosed in an infant or toddler, two kinds of specialists with expertise in the area of vision impairment may be included on the team: (a) a certified teacher of children with visual impairments (Teacher of the Blind and Visually Impaired or TBVI), and (b) a Certified Orientation and Mobility Specialist (COMS). Either of these specialists brings a unique perspective for supporting families with children with vision impairments. Early intervention service providers must seek out these services and, at a minimum, establish consulting relationships with TBVIs and COMS in their communities or through state agencies, in order to complete individualized evaluations and assessments. The Individualized Family Service Plan (IFSP) must address each child’s identified developmental needs and, in this case, the child’s need for vision services. Descriptions of specialized service providers for infants and toddlers with visual impairments, both educational/developmental and medical, are provided in Table 4 on the following page. Table 4 Descriptions of Specialized Vision Service Providers Teacher of the Blind and Visually Impaired (TBVI) A licensed teacher of the visually impaired (TBVI) provides “vision services” to children aged birth through twenty-one years of age. The training of TBVI’s is specific to children diagnosed with vision impairment. TBVI’s provide early intervention vision services specific to the needs of infants and toddlers, i.e., functional vision assessments, pre-Braille, evaluating the need for adaptive equipment, and enhancing development of compensatory skills. Certified Orientation & Mobility Specialist A Certified Orientation and Mobility Specialist (COMS) is a professional instructor who teaches a person with a visual impairment how to move safely and efficiently in a variety of environments. This specialist can help the family of an infant or toddler modify the environment and learn strategies to promote movement and safe exploration, for example. Pediatric Ophthalmologist A pediatric ophthalmologist is a physician specifically trained to diagnose and treat infants and toddlers with eye diseases. As a medical doctor, he/she is able to prescribe medication and perform surgery when necessary. Optometrist Optometrists may screen for common eye problems and prescribe corrective lenses when necessary. Pediatric Optometrist A pediatric optometrist has specialized training and experience to work with young children with eye problems in need of corrective lenses. Low Vision Optometrist These optometrists specialize in evaluating and prescribing special low vision devices for patients with vision impairments. Optician Opticians provide the aids (e.g., glasses) prescribed by ophthalmologists and optometrists. 1 0 EARLY INTERVENTION GUIDELINES FOR INFANTS AND TODDLERS WITH VISUAL IMPAIRMENTS WHAT ARE VISION SERVICES Components of Early Intervention for Infants and Toddlers with Visual Impairment The following vision service components may be considered in developing a child’s IFSP. 1. Development of attachment and meaningful social relationships and communication skills (listening, turn-taking, personal expression, nonverbal communication, emergent literacy) 2. Assessment of sensory capabilities and preferences in order to facilitate the effective use of all senses, including the use of low vision devices if appropriate 3. Adaptation of environments, toys, and learning materials to make them more accessible 4. Use of compensatory skills to accommodate for vision loss (e.g., strategies for accomplishing tasks using touch rather than vision; learning to use all senses as effectively as possible) 5. Cognitive development opportunities that are experienced based and designed to teach concepts that are acquired primarily through vision (basic concepts, problem-solving skills) 6. Facilitation of emergent literacy including pre-literacy for potential Braille and print readers through collaboration with families and other professionals 7. Gross and fine motor development (as well as the development of physical control and stamina) with special attention to prerequisite skills required for age appropriate orientation and mobility, and Braille, print reading and writing if appropriate 8. Development of age appropriate orientation and mobility instruction (self-directed, independent movement in the environment) 9. Instruction in daily living skills typically acquired through incidental visual learning that must be taught using hands-on, step-by-step procedures to infants and toddlers with visual impairments in order for them to function independently within natural environments (e.g., self-care skills, ability to do household chores) 10. Comprehensive family support that includes emotional support and access to information and resources that will help families become life-long advocates for their children 11. Thorough understanding of medical and visual conditions and their implications for early intervention and education services 12. Recreational opportunities that enhance creativity and enjoyment *Note: This table is not intended to be a “menu of services” for infants and toddlers with visual impairment. Adapted from the 2003 Policy Statement of the Division of Visual Impairment, Council for Exceptional Children. EARLY INTERVENTION GUIDELINES FOR INFANTS AND TODDLERS WITH VISUAL IMPAIRMENTS 1 1 Role and Function of Vision Professionals Consulting with Early Intervention Service Providers 1. Participate in the multidisciplinary evaluation and assessment of infants and toddlers with visual impairment: a. Perform functional vision assessments. b. Perform orientation and mobility assessments (Certified Orientation and Mobility Specialist (COMS)). c. Obtain and interpret all ophthalmologic, optometric, and functional vision reports for families and other IFSP team members. d. Assist with comprehensive developmental evaluation/assessment of infant or toddler, providing input on adaptations of assessment tool items as necessary for visual impairment and assisting with interpretation of results. e. Assist with communication skill assessments in pre-reading and listening. f. Help to address the infant or toddler’s need for assistive technology. g. Recommend assessment by other vision specialists as needed (e.g., orientation and mobility). h. Assist families in assessing their concerns, priorities and resources regarding their infant or toddlers’ visual development. 2. Participate in the development of the Individualized Family Service Plan: a. Contribute to the infant’s or toddler’s present levels of performance by discussing how performance is affected by the visual impairment and by providing information on the child’s learning style, use of visual information, and other strengths unique to individual infants or toddlers. b. Identify outcomes related to the visual and orientation and mobility needs of the infant or toddler and their family. c. Identify frequency, intensity, method, location, and services for meeting 3. IFSP outcomes. 4. Address development of pre-literacy skills and, by age three, recommend appropriate reading and writing media. For further information, TBVIs are directed to: “Infant Teacher of the Visually Impaired: Roles and http://tsbvi.edu/infants/3231-infant-teacher 1 2 EARLY INTERVENTION GUIDELINES FOR INFANTS AND TODDLERS WITH VISUAL IMPAIRMENTS RESOURCES NAPVI (National Association for Parents of Children with Visual Impairments) maintains a Parent Directory, sponsors conferences, and has publications, and suggests useful links on its website: www.spedex.com/napvi/ MNAPVI (Minnesota Association for Parents of Children with Visual Impairments) Contact: Info@mnapvi.org Phone: 612/486-2784 Website: www.mnapvi.org/Minnesota_NAPVI/Welc ome.html Minnesota State Academy for the Blind (MSAB) Phone: 800-657-3634 Address: 400 SE 6th Ave Faribault, MN 55021 Web site: www.msab.state.mn.us Minnesota Braille and Talking Book Library (MBTBL) Phone: 507-333-4828 Address: 400 SE 6th Ave Faribault, MN 55021 Web site: www.msab.state.mn.us American Foundation for the Blind (New York, New York) Phone: 800/232-5463 Web Site: www.afb.org Email: afbinfo@afb.net Browse their pull-down menu of topics relevant to infants and families. Assorted informational brochures and fact sheets for parents and service providers Hadley School for the Blind: Parent/Child Program Contact: Ask for a parent/child instructor Phone: 800/323-4238 Web site: www.hadley.edu Address: 700 Elm Street Winnetka, IL 60093 Free distance education courses for parents and grandparents of blind children The Perkins School for the Blind Phone: 617/924-3434 Web site: www.perkins.org Email: Info@Perkins.org National Braille Press Phone: 888/965-8965 Web site: www.nbp.org/ic/nbp/readbooks Free packet of Braille books for birth-to-five year olds. Texas School for the Blind and Visually Impaired Website: www.tsbvi.edu/Education Phone: 800-872-5273 See Early Childhood Instruction (ECI) – Infants & Toddlers with Visual Impairments. Blind Babies Foundation Phone: 510/446-2229 Web Site: www.blindbabies.orgEmail bbfinfo@blindbabies.org Address: 1814 Franklin Street, 11th Floor Oakland, CA 94612 EARLY INTERVENTION GUIDELINES FOR INFANTS AND TODDLERS WITH VISUAL IMPAIRMENTS 1 3 APPENDIX A - Roles and Responsibilities Infant Teacher Of The Visually Impaired: Roles And Responsibilities Infants: Below are additional roles and responsibilities that the VI teacher assumes for infants. Acquire and expand information about impact of visual impairment on child's development, working with families, current research, resources, etc. Acquire information and follow all IDEA Part H (ECI) timelines and requirements. Administer Functional Vision Assessments for identified infants. (On-going; update for progress reports) Administer Learning Media Assessments for identified infants. (On-going) Consult with Early Childhood Intervention staff and parents concerning assessments (INSITE, E-LAP, Hawaii, Oregon, etc.) and evaluations, modifications, strategies, impact of vision loss, vision screening. Develop IFSP with team. Attend IFSP meetings. Provide services to visually impaired infants and parent training as outlined on the IFSP. Areas may include: Learning Media--ensure the child has opportunities to have toys and activities to use all sensory modalities. Enhance bonding between family members Motor--Gross, Fine, and O&M/Early Movement Self-Help--Eating and Drinking, Dressing and Undressing, Toileting, Personal Hygiene, Sleeping Patterns Cognition--Body Concepts, Object Exploration and Manipulation, Experience-Based Early Concept Development, Problem-Solving Social-Emotional Communication--Receptive and Expressive Sensory--Vision (Low Vision Efficiency Training, Large Print/Pictures/Books, Optical Devices), Auditory/Listening Skills, Tactual (Pre-Braille/Tactile Symbols), Vestibular, Sensory Integration Family Needs Adaptive Devices Act as consultant to day care providers, extended family members, Early Childhood Intervention staff, Related Service Staff, etc. when needed. Order adaptive and tactual aids. Monitor identified visually impaired students. Act as a liaison and consultant with the following persons/staff: o Commission for the Blind o Case workers o Doctors o Ophthalmologists o Neurologists o Parents and other caregivers o District support personnel o Orientation and mobility specialist o Occupational therapist o Physical therapist o Speech therapist o Education Service Center staff 1 4 EARLY INTERVENTION GUIDELINES FOR INFANTS AND TODDLERS WITH VISUAL IMPAIRMENTS o Early Childhood Intervention staff Provide information and materials to help ensure the VI infant's home is an appropriate learning environment (lighting needs, wide variety of objects/toys to explore and manipulate, Little Room, light box, etc.) Ensure that parents have opportunities to meet and obtain information about visual impairment issues at parent meetings, workshops, conferences, etc. These can be held locally or regionally. Participate in transition planning. Perform other duties as required for Special Education such as: o Attend IFSPs. o Update Cumulative (CUM) folders o Follow IDEA Part H timelines and requirements o Complete paperwork for re-evaluation o Maintain materials inventory *Developed by TSBVI Outreach Texas school for the Blind. Modified by Region 10 Low incidence MN EARLY INTERVENTION GUIDELINES FOR INFANTS AND TODDLERS WITH VISUAL IMPAIRMENTS 1 5 Certified orientation and mobility specialists (COMS) have many roles, including: Assessment and Evaluation Conducting the functional vision evaluation. Conducting the orientation and mobility evaluation. Evaluating student progress and providing progress notes as per district policy. Direct Instruction in the Expanded Core Curriculum Encouraging purposeful movement, exploration of immediate surroundings and motor development for infants with visual impairments. Teaching spatial and environmental concepts and use of information received by the senses (such as sound, temperature and vibrations) to establish, maintain, or regain orientation and line of travel (e.g., using traffic sounds at an intersection to cross the street). Providing support to the student to facilitate development of self-esteem, self-determination and social acceptance. Orienting students to unfamiliar environments. Instructing in efficient use of low vision for movement. Teaching efficient use of low vision devices. Teaching use of mobility tools, including the long cane and adaptive mobility devices, for safely negotiating the environment. Providing travel experiences in the community, including residential and business environments and public transportation systems. Supporting Educational Teams Supporting families of young children in developing gross and fine motor skills, sensory skills, basic concepts and other developmental milestones. Ensuring continuity from early childhood intervention services to school-aged programs. Ensuring that appropriate vision-specific supports are in place and the necessary skills attained for transitioning from school to adult life. Modifying the environment to accommodate specific mobility needs. Modeling appropriate O&M techniques for other team members. Providing, creating and acquiring adapted materials such as tactual maps and mobility devices. Providing in-service training and consultation to other team members in home, school and community settings. Recommending orientation and mobility strategies for access to the general curriculum such as physical education class, and participation in school and community extracurricular activities. Administrative/Record Keeping Duties Maintaining records on all evaluations, IFSP/IEPs, and progress reports. Attending IFSP and ARD meetings. Ordering and providing adapted materials from the American Printing House for the Blind through the Federal Quota program and from other resources. 1 6 EARLY INTERVENTION GUIDELINES FOR INFANTS AND TODDLERS WITH VISUAL IMPAIRMENTS Screening Tools EARLY INTERVENTION GUIDELINES FOR INFANTS AND TODDLERS WITH VISUAL IMPAIRMENTS 1 7 NEW MEXICO VISION SCREENING TOOL FAMILY INFANT TODDLER PROGRAM NEW MEXICO SCHOOL FOR THE BLIND AND VISUALLY IMPAIRED (NMSBVI) “An accurate understanding of the status of a child’s vision and hearing is necessary when determining his/her developmental status. Vision and hearing are integral to overall development. This provides information that assists in the assessment of a child’s development abilities in areas such as communications, cognition, gross/fine motor, social or emotional, and adaptive behavior. Further, vision and hearing screening help early intervention personnel and parents identify which children need additional assessment by professionals who specialize in these areas of development”. NM Family Infant Toddler Program, Technical Assistance Document, Evaluation and Assessment, February 2006. The New Mexico FIT program requires that every child entering the Family Infant Toddler Program receive a vision screening. The New Mexico vision Screening Tool was designed to help programs have a consistent method of screening vision for children in New Mexico. The screening tool includes parent interview, as it is important to ask parents if they have noticed any vision problems. 1) Medical history is often related to vision problems and is included in the screening tool to help you think about medical history, which might be related to vision issues. Exposures during pregnancy are included as certain exposures can also increase the possibility of vision problems. Family history is included because some vision issues in immediate family may be genetic. 2) Appearance of Eyes: Sometimes-visual problems can be noted by observation of the appearance of the eyes and this area indicates some of the observations that can be important. 3) Behaviors That Are Often Associated with Visual Impairment: Children often demonstrate behaviors, which can indicate that they are having some difficulty with their vision. This checklist area is a reminder for the evaluator of some of these behaviors, which can be related to vision problems. 4) Development Vision Screening: vision develops in a sequential, predictable sequence similar to other areas of development. This page is included to remind you of what typical visual skills you might expect for certain ages. Many of these items are related to your other developmental assessment tools. 5) The summary area of the vision screening tools is to discuss your observations about vision with the parent and to obtain permission to make a referral to NMSBVI for further vision assessment if needed. Professional judgment within the team is a strong component of the decision-making process about whether to refer the child for further vision assessment. Because of the important role of vision in the early developmental sequence, NMSBVI would prefer “over” referrals to a “wait and see” approach. 1 8 EARLY INTERVENTION GUIDELINES FOR INFANTS AND TODDLERS WITH VISUAL IMPAIRMENTS NEW MEXICO VISION SCREENING TOOL Referred to NMSBVI Yes No Date: FAMILY INFANT TODDLER PROGRAM Referred to Ophthalmologist & NMSBVI Yes No Date: Copies to family for Ophthalmologist Yes No Date: Child’s Name: Parent’s name/Phone: Chronological Age: Signature (person doing screening): Eye Care Specialist: DOB: Adjusted Age: Date: Date of last exam: PARENT INTERVIEW Results of parent interview; describe any concerns: I. HISTORY: (check all that apply) A. Child’s History Low birth weight <3.5lbs. Hydrocephaly/microcephaly PVL (periventricular leukomalacia) Prematurity w/oxygen <32 wks Syndrome Shaken Baby Syndrome Small for gestational age Cerebral hemorrhage Significant illness: Meningitis/encephalitis No Concerns Hypoxia, anoxia, low apgars Hearing loss Head trauma/tumor Neurological disorder Sepsis Medications: SeizuresRetinopathy Intraventricular hemorrhage (IVH) Vacuum Extraction Cerebral Palsy B. Exposures during pregnancy Rubella Toxoplasmosis Cytomegalovirus (CMV) Significant illness Herpes Alcohol/drugs Shaken Baby Syndrome C. Immediate family history of childhood vision loss Strabismus/Amblyopia Retinal Dystrophy/degeneration Systemic syndromes w/ ocular manifestations Congenital Cataracts Glasses in early childhood Retinoblastoma Congenital Glaucoma Sickle cell disease Other: EARLY INTERVENTION GUIDELINES FOR INFANTS AND TODDLERS WITH VISUAL IMPAIRMENTS 1 9 II. APPEARANCE OF THE EYE (S): (check all that apply) Cloudy or milky appearance Abnormal constriction or dilation of pupil(s) Keyhole pupil Difference between eyes (size, shape, etc.) Sustained eye turn inward or outward? (after 4-6 months) No Concerns Excessive tearing Droopy eyelids Jerky eye movements (nystagmus) Absence of eyes moving together III. BEHAVIORS THAT ARE OFTEN ASSOCIATED WITH VISUAL IMPAIRMENT: No Concerns Tilt or hold head in unusual position? Seem to look beside, under, or above and Visually inattentive/uninterested? object Hold objects close to eyes or bend close to High sensitivity to room light or sunlight? look? Stare at lights, ceiling fans? (after 3 months or Inconsistent visual behavior? age) Difficulty sustaining eye contact 2 0 EARLY INTERVENTION GUIDELINES FOR INFANTS AND TODDLERS WITH VISUAL IMPAIRMENTS IV. DEVELOPMENTAL VISION SCREENING (Check each item observed) YES NO Comments: YES NO Comments: YES NO away Comments: YES NO BIRTH: Responds to movement or light with a blink reflex Pupil responds to light on/off Makes momentary eye contact Uses locomotion to seek or avoid Comments: YES NO BY 1-2 MONTHS: Looks at objects, follows visually Looks at adult; responds to voice Follow person with eyes Observes movement in room indicates BY 2-4 MONTHS Holds and looks at rattle Social smile Shows interests by reaching Scans visual environment or turns Comments: BY 4-7 MONTHS Reaches and grasps for toys Retrieves lost pacifier or bottle Initiates social contact Facial mimic Creates social contact (reaches) YES NO self Comments: YES NO Comments: YES forth NO BY 7-10- MONTHS Works to obtain out of reach toy Uncovers toy Matches cubes Reacts to strangers Shows distinct stranger reaction Plays peekaboo, pat a cake, so-big Comments: YES NO BY 13-18 MONTHS Walks well alone Places pellet in bottle Builds tower of two cubes builds tower of 3-4 cubes Finds toy under cup Explores drawers and cabinets needs by pointing Identifies one body part Plays “where is your eye?” etc Looks for hidden objects Begins to detour around obstacles Points or asks for desired object BY 18-24 MONTHS Walks upstairs, holding rail Kicks large ball after demonstration Runs well Dumps pellets Builds tower of 5-6 cubes Places forms in formboard with help Names on picture Identifies 5 objects or pictures feeds well with spoon Imitates adult activities (use of tools, housekeeping, etc) BY 18-36 MONTHS Tries to do things for self Begins to play cooperatively with peers Comments: BY 10-13 MONTHS Tries to build a cube tower Imitates scribble Explores toys Puts one object inside another Finds toy behind solid screen Uses object in imitation of an adults Hanks toy or other object back and Rolls ball to another Imitates actions EARLY INTERVENTION GUIDELINES FOR INFANTS AND TODDLERS WITH VISUAL IMPAIRMENTS 2 1 YES NO BY 24-30 MONTHS Walks upstairs, alternating feet Holds crayon with fingers (adult grasp) Builds tower of 9 cubes Imitates vertical and horizontal strokes Knows use of 3 objects Uses objects in play to represent others Places forms in form board without help Names 5 objects or pictures Identifies 7 pictures Helps with dressing YES NO Comments: YES NO cube Comments: YES NO Comments: BY 24-36 MONTHS Helps parents Begins cooperative play Understands taking turns children Comments: BY 30-36 MONTHS Strings small beads Builds 3-cube structure Imitates cross Imitates 3-cube structure Builds tower of 10 cubes Copies circle Solves formboard (rotates) Tells use of 3 objects Puts shoes on Feeds self competently BY 36-42 MONTHS Cuts paper with scissors builds 3structure from model Names 10 pictures Washes and dries hands and face Does simple errands and chores Plays cooperatively with other SUMMARY OF VISUAL CONCERNS: 2 2 EARLY INTERVENTION GUIDELINES FOR INFANTS AND TODDLERS WITH VISUAL IMPAIRMENTS NEW MEXICO VISION SCREENING TOOL FAMILY INFANT TODDLER PROGRAM NMSBVI SUMMARY FORM Child’s Name: Birth Date: Parent/Caregiver: Phone: Parents Address: City: State: Referring Agency: Contact Person: Phone: Date: Zip Code: SUMMARY We have no concerns regarding this child’s vision at this time; based on the parent interview child/family medical history and developmental screening: Caregiver Signature: _________________________________________ Date: __________________ We have identified risk factors/signs/observations, as noted in the vision screening. I authorize you to refer my child to an optometrist or a pediatric ophthalmologist for follow up. Caregiver Signature: _________________________________________ Date: __________________ We have identified risk factors/signs/observations, as noted in the vision screening. I authorize you to release my child’s information to the district teacher of the blind/visually MN Help Me Grow Program impaired for follow-up. If necessary, provide a summary of concerns: Caregiver Signature: _________________________________________ Date: __________________ REFERRAL INFORMATION Phone: 1-866-693-GROW (4769) Online: Help Me Grow http://www.parentsknow.state.mn.us/parentsknow/age1_2/HelpMeGrow_SpecialNeeds/ReferChild/index.html EARLY INTERVENTION GUIDELINES FOR INFANTS AND TODDLERS WITH VISUAL IMPAIRMENTS 2 3 APPENDIX B - Tools 2 4 EARLY INTERVENTION GUIDELINES FOR INFANTS AND TODDLERS WITH VISUAL IMPAIRMENTS Special Education Services NAME OF DISTRICT Education District #DISTRICT NUMBER ADDRESS, CITY, STATE ZIP To The Doctor: An eye report can help teachers to understand more thoroughly the educational needs of children with a degree of eye difficulty. It may be appropriate for a teacher of the visually impaired to provide consultative and/or direct services to this learner, or review the nature of present services. Medical information is needed to determine appropriate service. Medical entrance criteria for programming is based on an acuity of 20/60 or worse in the best eye with correction, and/or a visual field of 20 degrees or less, and/or a congenital, degenerative or progressive eye condition. If you find you are unable to get an accurate acuity we request you estimate it to the best of your ability. MN Rule 3525.134 reference: (a) estimation of acuity is acceptable for difficult-to-test pupils; and (b) for pupils not yet enrolled in kindergarten, measured acuity must be significantly deviant from what is developmentally age-appropriate” Thank you very much for your assistance, This information is required by federal and state laws to ensure special education services including the use of federal quota monies to provide equipment from American Printing House for the Blind, including but not limited to reading stands, Braillers, equipment to read specially formatted electronic books, electronic magnifiers, wide line notebooks and many other items available through American Printing House for the Blind ENTER YOUR NAME, Teacher for the Blind/Visually Impaired CELL: FAX: APLICANTS NAME: SEX M F BIRTHDATE: Ophthalmological Information Eye condition primarily responsible for visual loss: Secondary condition, if any: _________________________Right Eye? __________Left Eye? _________ Etiological factor for primary eye condition: _____________________________ Family members with visual loss: _____________________________ Describe the appearance of eye, including fundi: _______________________________________________________________________________________ Central Visual Acuity With Best Correction Evaluation tool used to determine Distance (20’) Acuity readings - Right Eye Acuity readings –Left Eye Acuity readings – Both Eyes Near (14”) EARLY INTERVENTION GUIDELINES FOR INFANTS AND TODDLERS WITH VISUAL IMPAIRMENTS 2 5 If unable to determine the “visual acuity with best correction”, give estimation. Refraction: Should child wear glasses? __________________________Contacts? __________________________ What is the purpose of the glasses? __________________________ Are low vision aids likely to be of assistance to him/her? __________________________ Does the child have color vision deficiencies and for what colors? __________________________ Is this vision condition progressive and/or degenerative? __________________________ What is the prognosis of the condition? __________________________ Is there any limitation in the field of vision? __________________________ Right Eye? __________________________ Left Eye? __________________________ What is the widest diameter in Degree of remaining visual field? (attach perimetric chart if significant) Right Eye? __________________________ Left Eye? __________________________ Please comment on other factors that may affect the child’s visual functioning: **************************************************************************************** Date of examination: _______________________________ Date of report:_________________________ ________________________________________________________________________________________ Signature of Eye Specialist ________________________________________________________________________________________ Type of Eye Specialist ________________________________________________________________________________________ Address Please return the form to: NAME ADDRESS CITY, STATE ZIP FAX EMAIL 2 6 EARLY INTERVENTION GUIDELINES FOR INFANTS AND TODDLERS WITH VISUAL IMPAIRMENTS FOUNDATIONS OF ORIENTATION AND MOBILITY: BIRTH TO THREE YEARS BIRTH TO SIX MONTHS Concurrent Motor Skills In prone holds head up Brings hands together Rolls over Grasps object intentionally Sits with support Reaches for objects Brings hands to mouth Shakes and plays with rattle Sensation Expose to indoor and outdoor sounds and sound toys; isolate each sound if possible—follow by touching/holding. Begin basic vision stimulation; incorporate with reaching, tactual stimulation and auditory cues; keep visually attractive sound-producing objects within reach at all times. Provide daily tactual stimulation by massage and stroking; use variety of textures and substances; during play times, give interesting textures to hold and mouth - including fabric, household objects, toys, food in various forms, etc. Environmental Concepts Expose to household activities on a daily basis with child as close to activity as possible (e.g., front carrier); give object associated with the activity to child to hold and explore; provide simple description during activity. Begin including infant in errands and community activities as soon as possible; position child close to the action and arrange for maximum involvement, hopefully hands-on. Body Language Provide daily movement stimulation in the form of bouncing, swinging in prone, gentle spinning, rolling, and gentle roughhousing. Include all body parts and areas in tactual stimulation with emphasis on hands and feet; proceed slowly if this appears to be aversive; consult with OT or PT. Susan Shier Lowry Governor Morehead Preschool 319 W. Margaret Lane Hillsborough, NC 27278 919-732-6462 susan.lowry@ncmail.net EARLY INTERVENTION GUIDELINES FOR INFANTS AND TODDLERS WITH VISUAL IMPAIRMENTS 2 7 Space/Time Relationships Establish predictable daily routine, i.e., the same events in the same order each day. Arrange a “defined space” in child’s crib and/or playpen: place a solid row of attractive toys, household objects, textures, and other materials around the infant. These should form a perimeter located just slightly beyond infant’s reach. Any random movement should result in contact with an object, preferably a noisy one. Move this perimeter of objects further away as child begins to scoot or roll. Also hang object near chest from above. Place in defined space several times each day (not just at nap times) for 15-20 minutes each. For the low vision child, begin encouraging reaching to an object viewed; use sound of object as necessary; begin with most familiar objects. For the blind child, begin preparing for reaching to a sounding object; use objects that have great meaning for infant such as bottle, favorite rattle, etc.; have infant handle and explore tactually just prior to expecting him to reach for it; initially sound it while in contact with hid body, later sound it on tray of high chair in front of infant. Gross Motor Encourage developmentally appropriate motor skills; position in variety of ways throughout the day—prone, supine, side-laying, sitting supported, infant seat, front carrier; emphasize infant getting accustomed to prone while awake. Concurrent Motor Skills Sits up with support Transfers objects Grasps with thumb and forefinger Crawls Pulls to standing Finger feeds SIX TO TWELVE MONTHS Builds tower of cubes (2-3) Creeps Stands alone Places cube in cup Walking emerging Sensation Continue exposure to variety of sounds; provide direct experience; repeat exposure often. Continue incorporating vision stimulation and massage, but also encourage more active exploration of textures; increase variety of textures, shapes, temperatures, and consistencies; encourage play with semi-wet substances. Expose to novel smells, tastes, and textures by routinely introducing new foods or new textures and/or forms of familiar food; repeat as often as necessary to achieve acceptance. 2 8 EARLY INTERVENTION GUIDELINES FOR INFANTS AND TODDLERS WITH VISUAL IMPAIRMENTS Environmental Concepts Encourage exploration of furniture, appliances, household products, foods, and household activities; give consistent names to all objects but emphasize action words, i.e., use simple words to describe how the infant is acting upon the object. Continue including in errands and community activities; provide for more and more direct involvement as motor skills progress. Supervise frequent direct experience with sand, soil, mud, gravel, grass, leaves; exposure to trees, shrubs, sidewalks, streets, vehicles, etc., as much as possible; emphasize what the child is doing with object or substance. Arrange a “defined space” in child’s crib and/or playpen: place a solid row of attractive toys, household objects, textures, and other materials around the infant. These should form a perimeter located just slightly beyond infant’s reach. Any random movement should result in contact with an object, preferably a noisy one. Move this perimeter of objects further away as infant begins to scoot or roll. Also hang objects near chest from above. Place a defined space several times each day (not just at nap time) for 15-20 minutes each. For the low vision child, begin encouraging reaching to an object viewed, use sound of object as necessary, and use most familiar objects. For the blind child, begin preparing for reaching to a sounding object; use objects that have great meaning for infant such as bottle, favorite rattle, etc.; have infant handle and explore tactually just prior to expecting him to reach for it; initially sound it while in contact with their body, later sound it on tray of high chair in front of infant. Gross Motor Encourage developmentally appropriate motor skills; position in variety of ways throughout the day—prone, supine, side-lying, sitting supported, infant seat, front carrier; emphasize infant getting accustomed to prone while awake. Body Image Continue to provide daily movement stimulation, in addition to what infant can provide for himself. Begin passive differentiated movement of body parts accompanied by simple labeling of body parts and action, begin simple hand games and finger-plays that incorporate body parts; accompany with tactual stroking/massage; emphasize eyes, nose, mouth, arm, hand, leg, foot, stomach. EARLY INTERVENTION GUIDELINES FOR INFANTS AND TODDLERS WITH VISUAL IMPAIRMENTS 2 9 Space/Time Relationships Begin changing daily routine occasionally, but allow enough time to thoroughly adjust before introducing yet another change. Expand infant’s defined space to correspond with their gross motor skills, i.e., to playpen, then later to small corner of room; position one large toy, object or texture on each side of child’s space—each should be very different from the other—fasten them permanently—continue to use loose toys and objects around perimeter in addition to the permanent landmarks. When able to sit up, use defined space idea by providing tray attached to seating; tray should have edge to prevent toys/objects from “disappearing”; allow free play time with several objects on tray; also, when giving toys, food or bottle to infant, place on tray and help infant reach for it instead of placing in infant’s hand. For low vision child, begin incorporating reaching for toy/object viewed with vision stimulation activities; give intermittent tactual and auditory cues to reinforce looking; incorporate with feeding, i.e., have infant reach for spoon, jar, bowl, box, etc. For the blind child, continue reaching to sound but place object on tray in front of child while sounding; continue intermittent tactual input and always permit tactual exploration before; begin encouraging localization by headturn as reaching becomes consistent; begin decreasing auditory input to intermittent; later provide initial sound only. When reaching to sound is well established, begin object permanence activities; again, use meaningful and highly desirable objects; permit brief tactual exploration or play before requiring pursuit; begin by placing screen (cloth) over object as infant is holding it; later, proceed to containers over object (plastic tub, square cake pan, shoe box); use immediate physical prompting initially; also initially, have infant help place object under cover. Begin using “defined spaces” in feeding by using tray with edge; consistently position dish, cup, spoon and/or bottle even if infant is not independently using these items. Gross Motor Continue to encourage developmentally appropriate gross motor skills; do so within familiar defined spaces (e.g., playpen) and also in open space; from very beginning encourage to walk from a specific location (landmark) to another location within 2-3 feet; encourage cruising by arranging furniture close together for ease of transfer. For the low vision child, begin incorporating motor planning with vision stimulation by having child detour around obstacle and crawling under to retrieve a desire object. Provide daily opportunity for free movement and exploration; keep furniture in predictable arrangement; use a constant low-volume sound source for each room or area (fan, ticking clock, radio, etc.); avoid constant or even frequent medium-to-high volume TV or radio; remove articles unsafe or breakable and replace with interesting materials and household objects. 3 0 EARLY INTERVENTION GUIDELINES FOR INFANTS AND TODDLERS WITH VISUAL IMPAIRMENTS To prevent or discourage self-stimulation, arrange the child’s environment so they will contact interesting materials, toys and objects almost constantly; also provide one-on-one sessions daily that encourage interaction with a variety of objects; keep infant busy. TWELVE TO TWENTY-FOUR MONTHS Concurrent Motor skills Scribbles spontaneously Places several cubes in cup Walks steadily Runs Crawls up steps and down Turns pages of book singly Climbs into adult chair Throws ball Walks up stairs with assistance Completes circle, square, triangle formboard Jumps in place Sensation Expose to variety of sounds; provide direct experience; help child produce the sound themselves; give simple names for sounds they hear that have meaning for them; repeat experiences often. Continue incorporating vision stimulation with reaching and other fine motor tasks, but begin more advanced skills; incorporate use of vision with loco-motor tasks (ball play, hid and seek, egg hunt, etc.); continue use of distance vision outdoors; give simple names for objects viewed; repeat experiences often. Continue tactual exposure by continually increasing child’s involvement in many household and outdoor events; use textures to mark personal possessions, furniture, storage bin, etc; continue play with variety of dry and semi-wet substances; encourage exploration and manipulation of object parts; through physical modeling increase child’s repertoire of hand and finger movements (e.g., with Playdoh); demonstrate effort of movement (e.g., gentle, hard, lightly, firmly); begin matching grossly different textures. Expose to new and familiar smells with and without food; begin giving simple names for distinct and meaningful smells (bacon, bubble bath, mother’s cologne, pet, medicine, etc.); later begin asking to identify these smells with aid of other naturally occurring clues; teach how to sniff. Environmental Concepts Continue exploration of furniture, appliances, and household products; give name of each object and describe action on it (e.g., “Bill closed the door”); increase direct involvement in various household activities as motor abilities increase (e.g., have child help with different phase of dinner each night—setting table, putting vegetables in pan, pouring drinks, or cracking eggs); if child cannot do it, have child feel it being done. Continue errands and community activities; increase direct involvement; begin having child select grocery item and give money to cashier; point out sights, sounds, smell, and let child touch and explore if possible. Expand outdoor experiences and sensations (see 6-12 months) and provide frequent mediation; give labels for and demonstrate new actions with objects and substances; begin experiences with sidewalk, driveways, curbs, streets, corners, vehicles; vehicle-behavior, and weather; simple labeling of object and action associated with it; incorporate with use of distance vision. EARLY INTERVENTION GUIDELINES FOR INFANTS AND TODDLERS WITH VISUAL IMPAIRMENTS 3 1 Body Image Provide daily movement stimulation; teach how to use motor equipment that will provide high level of activity on child’s own. Continue hand games that incorporate body parts; try hide and seek game in which child searches for small object (raisin) attached to named body part; label facial features, hair, head, neck, fingers, stomach, elbow, knee, toes, bottom, back, etc.; ask child to point to these parts; later should be able to name when asked. Space/Time Relationships Continue predictable daily routine with frequent minor and occasional major changes. Expand child’s defined space by using small room or corner of a larger room; continue to use landmarks within these spaces; set up define spaces all over the house (or classroom), for example, play corner in bedroom, corner in living room, cabinet beside refrigerator that holds child’s own pots and pans; be sure to set up favorite toys and objects that are stored in each of these areas. Continue to use tray on high chair (see 6-12 months); later use place mat on table to define child’s space. Practices reaching to sound using only initial and intermittent sound; return to continual sound to encourage greater head turn (localization); begin presenting object in space (as opposed to on body or tray) and at increasing variety of angles; continue intermittent play and tactual exploration. Encourage child to walk to a continual sound source with 12-18 inches; as in reaching, use much initial and intermittent tactual exploration and play; later have child localize sound, “face” it, and walk to it; gradually increase distance and angles. Continue conventional object permanence activities and increase in difficulty; fade use of sound but reintroduce whenever new task appears too difficult; use defined spaces widely and assist child in replacing toys stored in each of these spaces; provide physical assistance to immediately retrieve dropped or thrown object and fade assistance; show child where household objects are kept (accessible) and help child obtain and replace them when helping with that activity (cutlery, soap/washcloth, paper bags for trash can, own clothes/diapers, etc.). Define child’s feeding space with place mat or, later, cafeteria tray; begin requiring child to find and replace cup, for/spoon, and napkin in proper position by themselves; while scooping, encourage child to use “resting hand” as a point of reference by holding bowl with it while scooping towards it with the other. Enhance concept of vertical space by encouraging climbing, sliding, and beginning jumping; teach filling and emptying vertical containers; stack large-to-medium interesting objects (shoe boxes, small pillows, coffee cans, etc.). Encourage child to climb on and crawl under and in various familiar and novel equipment/furniture; emphasize these spatial terms; later ask child to follow these same simple directions; work with variety of objects and containers (varying in size, shape and texture) to emphasize in, out, empty, and full. 3 2 EARLY INTERVENTION GUIDELINES FOR INFANTS AND TODDLERS WITH VISUAL IMPAIRMENTS Gross Motor Encourage appropriate gross motor skills; provide regular opportunities to try emerging running skills in familiar open space (yard, tennis court, gym, large garage, large open living area). Begin encouraging goal-directed movement, i.e., encourage child to move to a goal in mind rather than wander; if child is wandering, spinning, etc., persist in making sure child has plenty of opportunities for appropriate motor expression (rocking horse, sit’n spin, swing, trampoline, bouncing toy, etc.); initiate goal-directed movement by guiding child to familiar landmark then having child walk to child’s goal very close (by 3 ft); gradually increase these distances; later, introduce obstacles. Teach simple routes, 3 to 5 feet in length; only teach routes to a goal (landmark) that represents a familiar and desirable activity (bath tub, trampoline, refrigerator, record play, snack table, etc.); initially assure that child gets to participate in at least part of that activity upon completing the route, give enough physical assistance to move quickly in order to maintain time and space perception. Encourage beginning motor planning by assisting with the following: Opening cabinets Shutting drawers Crawling under furniture and into tight places Crawling over obstacles Later, demonstrates using stool, box, etc. to reach desired object; always reward motor exploration by discovery of desired and/or meaningful object. Formal Techniques Teach child to search for dropped object immediately; co-actively model accurate reach accompanied by quick sweeping motion; model with each hand alone; later encourage child to sweep farther and persist longer. Teach modified sighted guide by having child hold on to adult’s index finger; encourage firm grasp; work on walking in rhythm and at a faster pace; discourage pulling back; with curb greatly exaggerate your body motion and step; teach child to wait until you step first; give verbal reminders as necessary, fade. Encourage very selective trailing; if child cannot use standard trailing try two-handed method or use sighted guide with ont-trailing hand; give frequent verbal reminders to trail; use concrete language cues, e.g., “Hand on wall”. Teach a modified upper hand and forearm technique since laterality and midline concepts are not wellestablished; for example: both arms out in front, palms outward, hands on top of each other; use concrete and/or simple language cues such as, “hands out” or “upper arm”. Internalization Use constant environmental stimulation to discourage mannerisms; arrange for child to come in contact with interesting toys and objects often; expand repertoire of interactions with objects; provide movement stimulation and regular opportunities for physical exhaustion; use mild physical prompting to discontinue mannerism accompanied by one or two-word verbal reminder. EARLY INTERVENTION GUIDELINES FOR INFANTS AND TODDLERS WITH VISUAL IMPAIRMENTS 3 3 Discourage “spacing out” by intervening immediately—get child involved with motor equipment or toys and materials. Watch for “fiddling about”, i.e., sensory-motor preoccupation such as hitting surfaces, jiggling door knobs, repeated opening and closing doors, etc.; a certain amount is normal initially, if a particular habit lasts for more than 1-2 months, begin discouraging; physically model appropriate associated activity, e.g., opening and closing cabinets; show child how to open, crawl in, empty contents, replace, and close door; do this each time child begins the opening and closing; use non-punitive physical prompt with simple verbal reminder also, if necessary. TWENTY-FOUR TO THIRTY-SIX MONTHS Concurrent Motor Skills Makes train of cubes Jumps from chair Tower of 8-10 cubes Walks on line Alternates feet on stairs Walks on tiptoe Adapts to reversal of formboard Unscrews lids Two-dimensional shape discrimination Hops of one foot Imitates drawing vertical, horizontal and circular line Sensation Continue to draw attention to environmental sounds; have simple and brief discussions of sound descriptions: high, low, loud, soft, near, far, in front, behind, beside; identify sound sources, but only those that child has had hands-on experience with: cat, dog, bird, cow, horse, car, truck, air conditioner, typewriter, TV, washer/dryer, etc.; begin encouraging use of sound for traveling in home and classroom: initially expect to use appropriate sound as a goal, later teach to turn self in relation to sound and move to silent goal. Continue use of distance vision with loco-motor games, etc.; include negotiation of uneven surfaces, obstacles, steps; begin simple analysis and identification of objects followed by tactual confirmation; encourage child to use simple description. Continue play with novel textures and substances; teach more advanced tactual matching; begin tactual discrimination of common textures using feet and hands—ask child to name. Expose to more smells and their sources; take on regular field trips and teach beginning associations of smells with locations: grocery store, doctors, cafeteria, bakery, zoo, gas station, etc. Environmental Concepts Continue child’s involvement in household activities but expand extent of each task and number tasks; have child carry out at least one task from beginning to end as soon as child is capable 9e.g., undressing—including putting clothes in hamper); expand number of tasks child can do with complete independence. Expose to unfamiliar errands and community events as well as continue familiar ones; expand involvement in the latter; begin teaching independent travel in small, familiar store; more advanced participation in purchasing; more in depth discussion of sights, sounds, smells, landmarks, etc. 3 4 EARLY INTERVENTION GUIDELINES FOR INFANTS AND TODDLERS WITH VISUAL IMPAIRMENTS Continue exposure to residential concepts and landmarks, have child name familiar landmarks; guide child through beginning street crossing; listen to traffic, discuss when to cross, use sighted guide to cross at appropriate time, help child note textures, sounds and landmarks during crossing. Body Image Continue providing opportunity for daily movement stimulation and physical exhaustion through: Dancing Climbing Use of obstacle courses Trampolines Pools Jumping Running Swings Tricycles Continually introduce and teach novel equipment and games. Playground equipment Continue games involving naming body parts; introduce more advanced naming: wrist, waist, hips, shoulders, ankles, etc.; incorporate with comprehension of spatial prepositions (in, out, behind, in front, under, etc.) by having child place body parts in relation to own body and environmental objects; have child imitate your body position or action by doing it. Space/Time Relationships Continue using defined spaces set up all over house and at school; may be able to achieve total orientation in a small room now, although one may have to frequently encourage goal-directed movement and verbally and physically remind child of location of objects in relation to landmarks; arrange defined space in corner of yard adjacent to door; if appropriate, set up another area that includes favorite tree, swing set, etc. Continue to expect child to maintain consistent spacial relationships with all utensils during independent eating times. Use verbal and physical (if necessary) reminders to encourage child to replace toys/objects, clothes, etc.; continue building on object permanence by asking child to retrieve named objects within known location in large room, then later from adjacent room; introduce systematic search patterns of child’s immediate space and also perimeter of a room; encourage child to pursue beeper ball, jingle ball and bouncing (regular) ball. Continue concept of vertical space by providing more complex climbing equipment and teaching new skills; have child stack, build and connect increasingly small objects. Expand child’s understanding of spatial prepositions: in, out, under, on top, above, below, behind, in front, between; begin naming object-to-object relationships after child has considerable experience manipulating the objects; initially ask child to place objects as you describe, later have child tell you about how to the objects are positioned. Begin stressing activities that emphasize the sides of the body and spatial terms that reflect laterality (side-toside, side step, beside, sideways, etc.); encourage distinction between the two sides of the body; do not expect left/right labeling yet, but do refer to left and right in your description. EARLY INTERVENTION GUIDELINES FOR INFANTS AND TODDLERS WITH VISUAL IMPAIRMENTS 3 5 Teach one-quarter and one-half turn in relation to wall; use simple, concrete language cues, such as, “Side to wall” or Back to wall; use prop to enable tactual confirmation of alignment; later stress head, body and feet alignment; make lesions brief and within context of daily routine; use appropriate reward for age level. Teach pointing to continual distant sound source; initially use stationary source and vary angles (encourage head turn); later have child point to approaching sound source (mechanical toy, beeper ball, car, etc.) and track across midline; use physical modeling as necessary). Gross Motor Support and encourage advancing gross motor skills; devise adaptations as necessary to teach these skills; assure that child has opportunity to utilize on daily basis at home and school. Continue expecting goal0directed movement; may need t use additional sound cue at goal occasionally, but encourage using more landmarks, direction taking, straight-line walking and indirect auditory clues. Continue more advanced motor planning activities. Build child’s repertoire of body movements by physical modeling of adults and peers: dance movements, swaying, spinning, twisting, duck-walking, crab-walk, walking backwards, tumbling; no action is too meaningless to teach; teach how to move major body parts in isolation (shoulders, arms, rib cage, hips, feet, knees, head, etc.); build into child the desire to imitate peers. Continue stressing effort of movement; incorporate with dance; teach child to use appropriate effort of movement according to type of music (rock, classical, etc.). Begin stressing straight-line travel using squaring-off (“Back to wall”)’ initially use very short distances and physical assistance to maintain direction and gait; use meaningful and valued object at goal and initially pair with auditory clues; later use landmarks or large tactual aids at goal. Formal Techniques Introduce individualized modification of formal dropped objects technique; use favorite familiar objects; incorporate into game. Allow play with the objects; demand immediate searching, encourage persistence and teach soliciting assistance after thorough search. Continue sighted guide techniques, have variety of unfamiliar indoor settings in which trailing is appropriate; have child use conventional one-handed trailing; initially may need auditory goal to distract from extra tactual input; expect only very brief trailing to locate a specific object within familiar settings. Introduce narrow passage technique; use simple language; initially offer simple verbal description of situation, then fade. Introduce beginning sighted guide door technique; if possible, have child on the side closest to door, open door so that child will easily contact it, have child help hold it, then close the door; introduce concepts such as pull, push, toward, and away. 3 6 EARLY INTERVENTION GUIDELINES FOR INFANTS AND TODDLERS WITH VISUAL IMPAIRMENTS Continue modified upper hand and forearm; teach one-handed, cross body position when laterality/midline concepts are established; consult with OT or PT if possible. Begin teaching simple perimeter search of small room; include much simple discussion of each landmark encountered and the activities associated with each one; repeat no less than once/week initially, later review periodically; assure that child has frequent opportunities within the classroom routine to move to all landmarks in the room (e.g., to retrieve a necessary item for the teacher, to place something in the trash, to turn on the record play, to open the window, etc.). Introduce short, functional routes within the classroom routine and at home: utilize simple direction-taking, selective trailing, landmarks, and auditory clues; child may continue to require verbal and physical reminders for some time; only require use of route travel in situations where child cannot maintain orientation or adequate speed and efficiency; discontinue if and when child is able to use direct, free space movement toward the objective; do not require long or complex routes that involve a great deal of trailing. Introduce a protective device when child is demonstrating good orientation and has the occasion to travel a long, clear route (hallway, walkway, sidewalk, etc.) on a daily basis; use doll stroller, toy lawn mower, toy grocery cart, hula hoop, or modified pre-cane device; allow child to tactually explore obstacles encountered until child has become familiar with the route; emphasize accurate correction away from the obstacle and maintaining mental image of goal (must use meaningful location/activity as the goal, not just drill); may need to use additional auditory goals initially; later see if child can name obstacle encountered without tactual confirmation; evaluate on the use of the long cane— Consider the following: Ability to maintain grip Ability to keep tip in front Ability to use safely Ability to respond to obstacles Need Availability of adults to reinforce techniques and frequency of use… EARLY INTERVENTION GUIDELINES FOR INFANTS AND TODDLERS WITH VISUAL IMPAIRMENTS 37 Oregon Project B-7 Vision Screening Tool By Month The Oregon Project, Sixth Edition has several significant changes and additions: More than 200 skills have been added Newly designed recordkeeping with the ability to use a computer to graph the child's developmental profile New teaching activities for every skill An expanded resource section with glossaries and a comprehensive listing of beneficial educational materials Comprehensive list of agencies serving children who are blind or visually impaired Instruction for making toys and teaching materials For technical questions regarding The Oregon Project Curriculum and Skills Inventory, call (541) 245-5196 or email or_project@soesd.k12.or.us. For ordering questions regarding The Oregon Project Curriculum and Skills Inventory please see the "Ordering Information" link on the right side of this page. If there are additional questions, call (541) 776-8580 or email Suzanne_Vaughn@soesd.k12.or.us. The Oregon Project for Preschool Children who are Blind or Visually Impaired (The OR Project) is a comprehensive assessment and curriculum designed for use with children birth to six who are blind or visually impaired. It can be used by parents, teachers, vision specialists, or counselors in the home or in the classroom setting. The sixth edition of the OR Project includes several significant changes. Approximately 200 additional skills were added, totaling more than 800 distinct developmental skills, each with corresponding teaching activities. This new edition provides computer graphing of an individual child's profile to clearly depict the child's strengths and areas for instruction. The OR Project can be used with any child functioning at developmental levels between birth and six years. The Oregon Project consists of a: Manual Teaching Activities Reference Section Skills Inventory The MANUAL contains instructions and procedures, which will make best use of The OR Project materials. It includes a philosophical overview of the education and teaching of preschool children who are blind or visually impaired. The TEACHING ACTIVITIES include ideas for each skill taught either in the home or classroom setting. They are suggestions for the parent and teaching staff, not designed as step-by-step "recipes," but rather, as starting points for instruction. The skills and activities can serve as frameworks for writing prescriptive programs to fulfill 3 8 EARLY INTERVENTION GUIDELINES FOR INFANTS AND TODDLERS WITH VISUAL IMPAIRMENTS IFSP/IEP objectives. The REFERENCE SECTION includes a Glossary of educational and vision terms needed by those working with children who are visually impaired, a list of references, resources for obtaining educational materials and literature, things to make and do, articles on play and development, and blank copies of all the forms, checklists, and informal evaluations which can be copied and used. The SKILLS INVENTORY consists of more than 800 behavioral statements, organized in eight developmental areas: Cognitive Language Compensatory Vision Self-Help Social Fine Motor Gross Motor Skills have been developmentally sequenced and arranged in age categories. All major skills needed by a child who is blind or visually impaired are included. The Skills Inventory is a criterion-referenced assessment, and enables educators to find the performance level, select long and short-term objectives, and record the acquisition of information from a completed OR Project Skills Inventory. EARLY INTERVENTION GUIDELINES FOR INFANTS AND TODDLERS WITH VISUAL IMPAIRMENTS 39 APPENDIX C - Medical Terms to look for This section contains words or terms commonly used in the identification, evaluation, assessment, and service provision of children with significant vision loss or blindness. ACCOMMODATION - The ability to change focus from a distance point to a near point and vice versa ACUITY LOSS - The loss of the ability to discriminate detail and, thereby, the experience of blurred vision ALBINISM - Full or partial lack of pigment; may affect eyes only or entire body; may cause abnormal visual development depending on the severity of the condition because of abnormal development of the macula of the eye AMBLYOPIA - Reduction in acuity, especially that in which there is no apparent pathologic condition of the eye. Amblyopia is often associated with strabismus ANIRIDIA - Congenital, traumatic, or surgical total or partial absence of the iris ANOPHTHALMIA - Absence of one or both eye globes APHAKIA - Absence of the crystalline lens in the eye, most commonly due to surgery ASTIGMATISM - A refractive error where blurred vision is caused by an irregular curvature of the surface of the cornea or the internal focusing structures BINOCULAR VISION - Coordinated use of the eyes to focus and align on one object and to fuse the two separate images into one visual image BLINK REFLEX - Spontaneous eyelid blinking, which occurs approximately every 5 10 seconds or is induced by sudden sounds or approaching objects CATARACTS - A condition in which the lens of the eye becomes cloudy, resulting in a loss of acuity CENTRAL SCOTOMA - Loss of perception of objects directly in the line of sight COLOBOMA - Incomplete closure in development of certain parts of the lower eye such as the retina or iris with frequent optic nerve involvement CONGENITAL - Present at birth CONJUNCTIVITIS - Inflammation of the membrane lining the eyelids and portions of the globe CONVERGENCE - When the eyes turn inward to maintain the line of sight on a near object/word 4 0 EARLY INTERVENTION GUIDELINES FOR INFANTS AND TODDLERS WITH VISUAL IMPAIRMENTS CORTICAL VISUAL IMPAIRMENT (CVI) - Inability of the brain to understand and process visual information regardless of eye health status (Also known as cerebral visual impairment) DEPTH PERCEPTION - The ability to perceive the relative positions of objects in space DETACHED RETINA - Separation of retina from the layers of the eye to which it is normally attached DIAGNOSTIC VISION EVALUATION - Vision evaluation given by an ophthalmologist or an optometrist to treat or diagnose the visual status of the patient DIPLOPIA - Double vision. EARLY INTERVENTION SERVICES – http://www.health.state.mn.us/divs/fh/mcshn/ecip.htm ESOTROPIA - Condition when one or both eyes turn in EXOTROPIA - Condition when one or both of the eyes turn out EYE TEAMING - Both eyes working together properly FARSIGHTEDNESS - See hyperopia FIELD LOSS - Inability to see in certain directions relative to the central line of sight FIELD OF VISION - The area that can be seen while looking straight ahead FIXATION - To direct a gaze and hold an object in view FOVEA - Small depression in the macula of the retina; area of sharpest vision FUNCTIONAL VISION EVALUATION - A vision evaluation administered by a vision teacher (TVI). The purpose of the evaluation is to determine how the individual being tested is able to use his/her vision. This helps to show what the individual can see in the everyday environment. GAZE SHIFT - Process of looking from one object to another GLAUCOMA - increased internal eye pressure with possible nerve damage and vision loss HYPEROPIA - (farsightedness) a refractive error that is usually caused by the eyeball being too short front to back or focusing power is too weak. With this condition, one can see objects at a distance using accommodation. Close objects require even more accommodation. HYPERTROPIA - Turning upward of one or both of the eyes LEBER'S CONGENITAL AMAUROSIS - Genetic disease that causes a progressive loss of vision EARLY INTERVENTION GUIDELINES FOR INFANTS AND TODDLERS WITH VISUAL IMPAIRMENTS 41 LEBER'S OPTIC ATROPHY - Genetic rare disease resulting in progressive difficulty for the optic nerve to send messages to the brain - Usually only in males and onset late in childhood LEGAL BLINDNESS - Central visual acuity of 20/200 or less in the better seeing eye with corrective lenses or a peripheral field loss in which the widest diameter of the field in the better eye is no greater than 20 degrees (14" diameter at 1 meter). LIGHT PERCEPTION - Ability to distinguish a light stimulus LOW VISION - Vision that cannot be corrected to normal with conventional lenses, but is functional. People with low vision can be prescribed low vision aids (optical and non-optical devices) to help maximize their visual skills. MACULA - The central area of the retina that surrounds the fovea and with the fovea comprises the area of most acute vision. MICROPHTHALMIA - Abnormally small eyeball, usually congenital MYOPIA - (nearsightedness) A refractive error caused by the eyeball being too long or focusing power being too strong. With this condition, one can see close objects, but objects at a distance appear out of focus. NEARSIGHTEDNESS - See myopia. NYSTAGMUS - A condition that involves small involuntary rapid movements of the eyes from side to side, in a circular, jerky, or pendular motion, or in a combination of these. It may be secondary to poor visual acuity or due to abnormality in brain function. OPHTHALMOLOGIST - A physician who specializes in the diagnosis and treatment of the eye, performs surgery, and prescribes glasses, medicine or therapy. OPTIC ATROPHY - Reduced ability of the optic nerve to send nerve impulses from the retina to the brain OPTIC NERVE - The cranial nerve that is responsible for carrying nerve impulses from the retina to the brain OPTIC NERVE HYPOPLASIA (ONH) - Congenital underdevelopment of the optic nerve OPTICIAN - An individual who specializes in fitting, adjusting and dispensing glasses and other optical devices prescribed by the ophthalmologist or optometrist. OPTOMETRIST - An individual who specializes in the diagnosis and treatment of the eyes and related structures, and prescribes glasses, medicine, prisms, low vision-devices and therapy. ORIENTATION AND MOBILITY (O&M) - A sequential process in which people with visual impairments are taught to utilize their remaining senses to determine their position within the environment and to negotiate safe movement from one place to another. 4 2 EARLY INTERVENTION GUIDELINES FOR INFANTS AND TODDLERS WITH VISUAL IMPAIRMENTS ORIENTATION AND MOBILITY SPECIALIST (COMS) - A certified professional trained to teach orientation and mobility skills to people with visual impairment. ORTHOPTIC TRAINING - Series of eye exercises for developing or restoring binocular vision PEDIATRIC OPHTHALMOLOGIST - An ophthalmologist with fellowship training in pediatric ophthalmology specializing in the diagnosis and treatment of the ocular problems in children, performs surgery, and prescribes glasses, medicine or therapy. PEDIATRIC OPTOMETRIST - An individual who works with the pediatric population and specializes in the diagnosis and treatment of the eyes and related structures, and prescribes glasses, prisms, low vision devices and therapy. This is an optometrist who has completed additional training in order to work with the pediatric population. PERIPHERAL FIELD - Vision allowing the perception of objects and movement outside of the direct line of sight. PHOTOPHOBIA - Abnormal sensitivity to light PROSTHESIS - A substitute for a missing body part such as the eye PTOSIS - A drooping of an eyelid PUPILLARY RESPONSES - Contractions or dilations of the pupil due to various changes in brightness REFRACTION - The measurement of the eye to determine refractive errors and the need for prescriptive lenses REFRACTIVE ERROR - A focusing error in the eye that prevents light rays from focusing accurately on the retina REHABILITATION TEACHER - Teachers trained to instruct persons with visual impairments in the use of compensatory skills and assistive technology that will enable an individual to live a safe, productive, and independent life. RETINA - Innermost layer of the eye formed of light sensitive receptors and nerves that connect the retina through the optic nerve to visual centers in the brain RETINITIS PIGMENTOSA (RP) – A hereditary progressive degeneration, often hereditary, of the retina, which leads to peripheral and eventually central field loss RETINOBLASTOMA - The most common malignant intraocular tumor of childhood occurring prior to the age of 5 years. RETINOPATHY OF PREMATURITY (ROP) - Condition resulting from complications of oxygen administration after low birth weight which may lead to reduced visual acuity, visual impairment or total blindness. EARLY INTERVENTION GUIDELINES FOR INFANTS AND TODDLERS WITH VISUAL IMPAIRMENTS 43 SCANNING -the ability to accurately change fixation from one object in space to another by use of eye and head movements. SCATTERED SCOTOMAS - Patches of vision loss in visual field. STRABISMUS - Eye muscle imbalance, e.g., esotropia (eye turning in), exotropia (eye turning out), or hyper/hypotropia (eye turning up or down). TEACHER OF THE VISUALLY IMPAIRED (TVI) - An individual who has completed a four-year teaching degree (or a Master’s degree) in the special education field specific to visual impairments. TRACKING - The ability to visually follow moving objects horizontally, vertically, or in an oblique plane VISUAL ACUITY - Ability of the eye to perceive detail; sharpness of vision VISUAL DISCRIMINATION - The ability to accurately compare and contrast visual images VISION SPECIALISTS – A generic term that includes certified teachers of children with visual impairments, orientation and mobility specialists, and Rehabilitation Teachers. Teachers of the visually impaired (TVIs) typically have special education certification to teach children. VISION THERAPY – A treatment regimen to correct or improve specific dysfunctions of the visual system identified by standardized diagnostic criteria. This type of therapy must be prescribed and administered by an optometrist. It is a medical therapy rather than a developmental or educational treatment. VISUAL EFFICIENCY - Degree to which a child can use vision; a skill that needs to be developed with visually impaired students. 4 4 EARLY INTERVENTION GUIDELINES FOR INFANTS AND TODDLERS WITH VISUAL IMPAIRMENTS Appendix D - Curriculum Letters Accessible Instructional Material Guidance The 2004 reauthorization of the Individuals with Disabilities Education Act (IDEA) includes a requirement that students who are visually impaired and students who are print disabled receive their textbooks and core instructional materials in specialized formats at the same time as their non‐disabled peers. The 2006 regulations implementing the 2004 IDEA includes guidance on how states and local districts are to respond to this legislation. The two sections of this legislation are the National Instructional Materials Accessibility Standards (NIMAS) and the National Instructional Materials Accessibility Center (NIMAC). Providing accessible formats in a timely manner is not a new requirement, however, collaboration with the NIMAC will improve this process for the students covered under these regulations. The NIMAS are standards used by textbook publishers to prepare electronic files of textbooks, which can be converted to specialized formats. Specialized formats means braille, audio, large print, digital or audio text, which can be used by students who are blind, visually impaired, physically disabled, and reading disabled. The NIMAC’s duties are to receive and maintain a catalog of these electronic files. Publishers, at the direction of local school districts, send these files to NIMAC. When a student in a local school district requires one of these specialized formats to have access to the general education curriculum, the local district will contact an Authorized User (AU), designated by the State of Minnesota to obtain from the NIMAC the particular files for core curricular and associated materials. The Authorized User assigns the electronic file to an Accessible Media Producer (AMP) to convert the file into the specialized format. Once the specialized format has been converted, the AMP will send the formatted file or hard copy to the local district that requested the materials. In some cases, the AU and the AMP will be the same entity. Current authorized users and accessible media producers for Minnesota are: State Services for the Blind Communication Center Bookshare.org Learning Ally In addition, Joan Breslin Larson at the MDE is an authorized user and can assign files from the NIMAC to an AMP. EARLY INTERVENTION GUIDELINES FOR INFANTS AND TODDLERS WITH VISUAL IMPAIRMENTS 45 Students with Print Disabilities IDEA refers to blind or other persons with a print disability as children who are served under the Act and who qualify in accordance with the Library of Congress regulations for the Act to Provide Books for the Adult Blind of 1931 as Amended. Persons who are blind or other persons with disabilities who have been certified by a competent authority as unable to read or use standard printed materials because of: Blindness A visual impairment Physical limitations A reading disability due to an organic dysfunction Certification of Eligibility In cases of Blindness, Visual Impairment, or Physical disability, certifying authorities include doctors of medicine or osteopathy, ophthalmologists, optometrists, registered nurses, nurse practitioners, physician assistants, therapists, professional staff of hospitals, institutions, and public agencies (e.g., local education agency related service personnel, teachers of the visually impaired, social workers, counselors, or rehabilitation teachers). In the absence of any of these, certification may be made by professional librarians or by any person whose competence under special circumstances is acceptable to the Library of Congress. In the case of a Reading Disability from an organic dysfunction, the certifying authority must be a doctor of medicine or osteopathy, who may consult with colleagues in associated disciplines. A family member is not eligible to be the certifying authority. LEA Responsibilities It is the responsibility of the LEA to provide curricular materials in alternate formats to students who need them for access to FAPE. At the time of purchase of any curricular materials, LEAs should direct publishers to submit an appropriately formatted file to the NIMAC. This language has been suggested for Textbook Adoption Contracts and LEA Purchase Orders: “By agreeing to deliver the materials marked with "NIMAS" on this contract or purchase order, the publisher agrees to prepare and submit, on or before ‐‐/‐‐/‐‐* a NIMAS fileset to the NIMAC that complies the terms and procedures set forth by the NIMAC. Should the vendor be a distributor of the materials and not the publisher, the distributor agrees to immediately notify the publisher of its obligation to submit NIMAS filesets of the purchased products to the NIMAC. The files will be used for the production of specialized formats as permitted under the law for students with print disabilities. Please note that the delivery of print versions should not be delayed in cases where the NIMAS fileset has yet to be validated and cataloged by the NIMAC. For additional information about NIMAS, please refer to aim.cast.org. For additional information about the NIMAC, refer to nimac.us . We would also be interested in learning about accessible versions of your instructional materials that may be available for purchase to support students with print disabilities who do not qualify for specialized formats created with files available from the NIMAS 4 6 EARLY INTERVENTION GUIDELINES FOR INFANTS AND TODDLERS WITH VISUAL IMPAIRMENTS * Use a date that is timely, perhaps at the same time that delivery is expected of hard copy books. It must allow for enough time for the NIMAC to receive a file, validate it, enter it into their data base, allow for it to be converted to an appropriate format and delivered to the school so that the student receives their alternative formatted text at the same time as their typically developing peer. Identifying eligible students: 1. Follow all LEA special education eligibility standards and child find/evaluation procedures including the policies and procedures for paying for a medical diagnosis. 2. Follow competent authority guidance 3. Identify eligibility for files from the NIMAC on the IEP form Identifying Accessible formats: Use appropriate assessments such as the Learning Media Assessment given by the Teachers of the Visually Impaired Assistive Technology Consultants or others with specific information should be involved and present at IEP meetings. If they cannot be present, their reports need to be available to IEP team members. Describe textbooks and related core materials to be provided in accessible formats on the IEP form. If an assessment to determine the accessible format has been completed, results should be reported also. Timely Manner Process: Definition: “timely manner” language has been interpreted by OSEP as “at the same time as other children receive instructional materials.” The regulation requires the Department to “ensure that all public agencies take all reasonable steps to provide instructional materials in accessible formats to children with disabilities who need those instructional materials at the same time as other children receive instructional materials.” 34 C.F.R. § 300.172(b)(4). OSEP’s commentary lists the following examples of reasonable steps: Reasonable steps, for example, would include requiring publishers or other contractors to provide instructional materials in accessible formats by the beginning of the school year for children whom the public agency has reason to believe will be attending its schools. Reasonable steps might include having a means of acquiring instructional materials in accessible formats as quickly as possible for children who might transfer into the public agency in the middle of the year. Reasonable steps would not include withholding instructional materials from other children until instructional materials in accessible formats are available. Considering the need for Accessible Instructional Materials in the IEP: An IEP team could consider adding language in the IEP such as “Does the student require accessible, alternate‐format versions of printed textbooks and printed core materials that are written and published primarily for use in elementary and secondary school instruction and are required by an SEA or LEA for use by students in the classroom?” A query of this kind is designed to prompt the IEP team to consider each print‐disabled student's need for accessible, alternate‐format versions of print instructional materials. EARLY INTERVENTION GUIDELINES FOR INFANTS AND TODDLERS WITH VISUAL IMPAIRMENTS 47 If a student with a print disability does need a specialized format, the IEP should specify the following: The specific format(s) to be provided (Braille, audio, digital text, large print, etc.) The services and/or assistive technology tools the student may need to access the specialized format The individual or individuals responsible for providing the specialized format, and The training and supports for the student, staff and family to effectively use the accessible materials and any related assistive technology What formats are required to be used in what setting in order for the student to receive a free appropriate public education. Suggested process for obtaining accessible formats in a timely manner: IEP teams make the determination of need using competent authorities as defined in IDEA. Team members also use data to make the decision about need and type of accessible format required by an individual student. The LEA representative on the IEP team will assume responsibility for following district procedure for obtaining accessible formats. This might include having a specific district person designated as a Digital Rights Manager (DRM). The contact between the LEA representative and the DRM will be identified on the IEP services page as a linkage that needs to occur so all textbooks and related core materials can be ordered in the accessible format required by students in a timely manner. The DRM can contact an Authorized User to identify textbooks and related core materials needed, the type of accessible format required, and to indicate any preference in the Accessible Media Producers (AMP) who will generate the accessible materials. If a student does not qualify to receive a file from the NIMAC, the LEA continues to have an obligation under IDEA to provide accessible instructional materials in a timely manner to all students who require them. For additional information, contact: Joan Breslin Larson, Minnesota Department of Education, 651.582.1599 or joan.breslin‐larson@state.mn.us 4 8 EARLY INTERVENTION GUIDELINES FOR INFANTS AND TODDLERS WITH VISUAL IMPAIRMENTS APPENDIX E LETTER REFERENCES POLICY STATEMENT Vision Screening for Infants and Children A Joint Statement of the American Association for Pediatric Ophthalmology and Strabismus and the American Academy of Ophthalmology Policy: The American Academy of Ophthalmology and the American Association for Pediatric Ophthalmology and Strabismus recommend timely screening for the early detection and treatment of eye and vision problems in America's children. This includes the institution of rigorous vision screening during the preschool years. Early detection of treatable eye disease in infancy and childhood can have far-reaching implications for vision and, in some cases, for general health. Background: Good vision is essential for proper physical development in growing children and educational progress. The visual system of the young child is not fully mature. Equal input from both eyes is required for proper development of the visual centers in the brain. If a growing child’s eye does not provide a clear, focused image to the developing brain, irreversible loss of vision may result. Early detection provides the best opportunity for effective treatment. The American Association for Pediatric Ophthalmology and Strabismus, the American Academy of Ophthalmology, the American Academy of Pediatrics, the American Academy of Family Physicians, and the American Association of Certified Orthoptists recommend early vision screening. Vision screening programs should provide widespread, effective testing of preschool and early school-age children. Many school systems have regular vision screening programs that are carried out by volunteer professionals, school nurses, and/or properly trained laypersons. Screening can be done quickly, accurately, and with minimum expense by one of these individuals. The screener should not have a vested interest in the screening outcome. As with all screening programs, vision screening should be performed in a fashion that maximizes the rate of problem detection while minimizing unnecessary referrals and cost. Beginning in the preschool years, those conditions that can be detected by vision screening using an acuity chart include reduced vision in one or both eyes from amblyopia, uncorrected refractive errors or other eye defects and, in most cases, misalignment of the eyes (strabismus). Amblyopia is poor vision in an otherwise normal appearing eye that occurs when the brain does not recognize the sight from that eye. Two common causes are strabismus (misaligned eyes) and a difference in the refractive error (need for glasses) between the two eyes. If untreated, amblyopia can cause irreversible visual loss. The best time for treatment is during the preschool years. Improvement of vision in children over the age of ten is seldom achieved. Strabismus is misalignment of the eyes in any direction. Amblyopia may develop when the eyes do not align. If early detection of amblyopia secondary to strabismus is followed by effective treatment, excellent vision may be restored. The eyes can be aligned in some cases with glasses and in others with surgery. However, restoration of good alignment does not ensure elimination of amblyopia. EARLY INTERVENTION GUIDELINES FOR INFANTS AND TODDLERS WITH VISUAL IMPAIRMENTS 49 Refractive errors cause decreased vision, visual discomfort (eye strain), and/or amblyopia. The most common form is nearsightedness (poor distance vision). It is usually seen in school-age children and is treated effectively, in most cases, with glasses. Farsightedness can cause problems with focusing at near and may be treated with glasses. Astigmatism (imperfect curvature of the front surfaces of the eye) also requires corrective lenses if it produces blurred vision or discomfort. Uncorrected refractive errors can cause amblyopia, particularly if they are severe or are different between the two eyes. In addition to detecting vision problems, effective screening programs should also emphasize a mechanism to inform parents of screening failures and attempt to ensure that proper follow-up care is received. Recommendations: The American Academy of Ophthalmology and the American Association for Pediatric Ophthalmology and Strabismus recommend that an ophthalmological examination be performed whenever questions arise about the health of the visual system of a child of any age. They recommend that infants and children be screened for vision problems as follows and that any child who does not pass these screening tests have an ophthalmological examination. 1. An ophthalmologist, pediatrician, family physician, or other properly trained health care provider should examine a newborn's eyes for general eye health and perform a red reflex test in the nursery. The baby with an abnormal red reflex requires urgent consultation. An ophthalmologist should be asked to examine all high-risk infants, i.e., those at risk of developing retinopathy of prematurity (ROP); those with a family history of retinoblastoma, glaucoma, or cataracts in childhood; those with retinal dystrophy/degeneration or systemic diseases associated with eye problems; or when any opacity of the ocular media or nystagmus (purposeless rhythmic movement of the eyes) is seen. An ophthalmologist should also examine infants with neurodevelopmental delay. 2. All infants should be screened by six months to one year of age for ocular health. This should include a red reflex test by an ophthalmologist, pediatrician, family physician, or other properly trained health care provider during routine well-baby follow-up visits. 3. Vision screening should also be performed on children between 3 and 3 1/2 years of age. A pediatrician, family practitioner, ophthalmologist, optometrist, orthoptist should assess vision and alignment, or individual trained in vision assessment of preschool children. Emphasis should be placed on checking visual acuity as soon as a child is cooperative enough to complete the examination. Generally, this occurs between ages 2 ½ and 3 ½. A child who is uncooperative at a second attempt at vision testing should be referred for a comprehensive pediatric medical eye evaluation. It is essential that a formal testing of visual acuity be performed by the age of 5 years. 4. Some evidence currently exists to suggest that photo screening may be a valuable adjunct to the traditional screening process, particularly in preliterate children. 5. Further screening examinations should be done at routine school checks or after the appearance of symptoms. Routine comprehensive professional eye examination of the normal asymptomatic child has no proven medical benefit. 5 0 EARLY INTERVENTION GUIDELINES FOR INFANTS AND TODDLERS WITH VISUAL IMPAIRMENTS 6. Children with presumed or diagnosed learning disabilities such as dyslexia should undergo a comprehensive pediatric medical eye examination so that any undiagnosed vision impairment can be identified and treated. They should be referred for the appropriate medical, psychological, and educational evaluation and treatment of the learning disability. There is not adequate scientific evidence to suggest that “defective eye teaming” and “accommodative disorders” are common causes of educational impairment. Hence, routine screening for these conditions is not recommended. Many serious ocular conditions, which can be found at screening, are treatable if identified during the preschool and early school-aged years. Many of these conditions are associated with a positive family history. Therefore, additional screening emphasis should be directed to high- risk infants and children, and screeners should readily refer such children to an ophthalmologist for a comprehensive medical eye evaluation. Approved by: Revised and Approved by: Revised and Approved by: Revised and Approved by: American Association for Pediatric Ophthalmology and Strabismus, May 1991 American Academy of Ophthalmology, Board of Directors June 1991 American Association for Pediatric Ophthalmology and Strabismus, September 1996 American Academy of Ophthalmology Board of Trustees, September 1996 American Association for Pediatric Ophthalmology and Strabismus, August 2001 American Academy of Ophthalmology, Board of Trustees October 2001 American Association for Pediatric Ophthalmology and Strabismus, October 2006 American Academy of Ophthalmology, Board of Trustees March 2007 ©2007American Academy of Ophthalmology® P.O. Box 7424/ San Francisco, CA 94102/ 415.561.8500 EARLY INTERVENTION GUIDELINES FOR INFANTS AND TODDLERS WITH VISUAL IMPAIRMENTS 51