fcm-derm study guide
advertisement

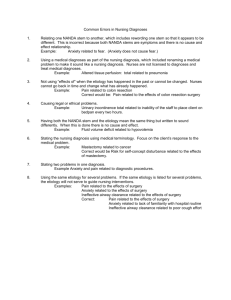
Disorders of the Skin and Subcutaneous Tissues Aug. 26, 2009 1. Basics Text: Harrison’s: Chapter 52 OBJECTIVES: The student should be able to: 1. Describe the structure and function of the skin. a. Protection against microorganisms b. UV rays c. Fluid loss d. Mechanical stress e. Sensory f. Temperature regulation g. Vit D production 2. Skin Lesions OBJECTIVES: The student should be able to: 1. Recognize and differentiate the morphology of the following primary skin lesions: 1. Macule- flat lesion that is typified by change in color example: freckle (ephelid) 2. Papule- raised lesion <5mm (solid) example: white head 3. Plaque- raised w/ flat plateau like surface example: psoriasis 4. Nodule- round lesion >5mm (larger papule) 1. Nodular Tumor Mass Solid raised >5cm Convalescence of many nodules 5. Pustule- raised lesion that has puss- not necessarily infection 6. Vesicle- raised lesion that has fluid, <5mm- NOT PUSS---example: allergic contact dermatitis (poision ivy) 7. Wheal- redish, edematous papule or plaque- normally short lived vasodilatation or penetrability—changes quickly, last only 24-48 in a defined area. 1 8. 9. Bulla- raised lesion that has fluid, >5mm (big vesicle) Cyst- Soft, raised, encapsulated lesion filled with semisolid or liquid contents 1. Sebacaeous Cyst Blockage of follicular canal with sebum Can see a hole where the canal should is o Test- white puss can be squeezed out 10. 11. TumorTelangiectasia- dilated superficial blood vessel—Test- blanch when tested with diascopy 2. Recognize and differentiate the morphology of secondary skin lesions: 1. Scale- Excessive build up of stratum cornium 2. Erosion- loss of epidermis, no harm to dermis 3. Ulcer- loss of epidermis and dermis, results in a scar 4. Fissure- crack in skin or ulcer in mucous membrane 5. Crust- Dried exudate of body fluid (yellow= serous, red=blood) 6. Erythema7. Excoriation- linear or angular lesion caused by scratching 8. Atrophy- An acquired loss of substance. In the skin, this may appear as a depression with intact epidermis or as sites of shiny, delicate, wrinkled lesions (epidermal atrophy) 9. Scar- change in skin secondary to trauma 10. Edema- fluid buildup under skin 11. Hyperpigmentation 12. Hypopigmentation 13. Depigmentation 14. Lichenification- thickening of the skin, makes well defined skin wrinkles 15. Hyperkeratosis- Hypertrophy of the horny layer of the skin, usually associated with hypertrophy of the granular and prickle-cell layers 3. Identify information that should be obtained in all dermatological histories. 3. Dermatologic Therapy Text: OBJECTIVES: The student should be able to: 1. Utilize eight guidelines that should be considered when selecting therapy for patients 1. KISS 2. Have pt. Repeat 3. Give written instructions 4. Topicals, how often, where & how much 5. Prescribe enough 2 6. If chronic, refills 7. Pregnant? 8. Warn of adverse reactions 9. “if its dry wet it, if its wet, dry it” . 2. Identify indications for each of the following: a. Lotions and Creams (for dryness) i. Restore water and lipids to epidermis ii. Creams more lubricating iii. Creams most useful for intertriginous (areas that rub together) area (groin, rectal area, axilla) and scalp iv. Apply to wet skin v. Preparations that contain urea (Carmol), or lactic acid are most effective vi. Menthol and phenol added to keep itching (purities) down b. Gels i. Are greaseless mixtures of propylene glycol and water, some contain alcohol ii. Useful for acute exudative inflammation (poison ivy, scalp areas) c. Ointments (dry lesions) i. Penetration better than creams ii. Grease with little water d. Wet dressings i. Best for exudative inflammatory diseases ii. Wet compresses suppress inflammation and debride crust and serum iii. Repeated cycles of wetting and drying make lesion dry iv. Once lesion is dry, switch to emollient creams and lotions 3. Identify indications for topical, intralesional and systemic corticosteroids. TOPICAL a. Psoriasis, hand eczema Group 1* Not on face, axilla, groin, under breast Limit use to 14 day b. Atopic dermatitis (adult) Group 2 &3 Not on face, axilla, groin or under breast Limit use to 21 days c. Atopic dermatitis (children) Groups 4&5 Limit use to 7-21days and intertriginous areas d. Eyelid and diaper dermatitis Groups 6&7 Reevaluate if no response in 28days INTRALESIONAL • Indicated for nodulocystic (cystic acne) and large pustular lesions, alopecia areata, keloids • May be given at full strength or mixed with saline or xylocaine (more painful) • May cause atrophy*, local reactions, systemic absorption, hypopigmentations, 3 telangiectasia, and sterile abscess 4. Identify contraindications and complications to systemic a. Produces antiinflammatory response b. Indicated when topical are unsuccessful c. Adverse effects include suppression of hypothalamic-pituitary-adrenal axis (HPA) and Cushing’s syndrome 4. Diagnostic Procedures Text: OBJECTIVES The student should be able to: 1. Describe indications and positive findings associated with the following diagnostic procedures: a. Potassium Hydroxide Prep (KOH) i. Consider when scaling fungal lesion is suspected ii. Dissolves keratin allowing visualization of fungal elements: hyphae, budding yeast b. Fungal Culture i. Indicated for hair and nail infections ii. Utilize cotton swab technique* c. Scabies Test i. Touch lesion with blue or black felt-tip pin ii. Wait a few minutes for ink to dry iii. Wipe of ink with alcohol pad iv. Burrow are highlighted as a dark line v. Scrape away with a curved #15 scapel blade and transferred to glass microscope slide d. Tzanck Smear i. For herpesvirus or varicella zoster virus infections ii. Base of vesicular lesion is scraped and placed on slide, air-dried, and stained with Giemsa or Wright’s stain iii. + multinucleated epithelia giant cells e. Wood’s Lamp Examination i. Perform in a dark room ii. Erythrasma-coral pink (corynebacterium m.) iii. Pseudomonas-pale blue iv. Tinea capitis secondary to dermatophytes-pale green to yellow 4 f. g. h. i. j. Curettage and Electrodesiccation Shave Biopsy Punch Biopsy Snip Excision Cryosurgery Aug 28, 2009 5. Tumors of the Skin Text: Harrison’s Chapter 83 A. Benign Neoplasm OBJECTIVES: Regarding the following, the student should be able to: 1. Describe and identify. 2. Establish a diagnosis. 3. Indicate the prognosis. 4. Establish a treatment plan. a. Acrochordon (Skin Tag) b. Callus/Chavus c. Cherry angiomas d. Nevus e. Seborrheic Keratosis f. Solar Lentigo B. Premalignant and Malignant Neoplasms OBJECTIVES: The student should be able to: 1. Describe and identify the following. 2. Recognize the diagnostic and therapeutic challenges associated with each. a. Actinic Keratosis b. Keratoacanthoma c. Melanoma d. Basal Cell Carcinoma e. Squamous Cell Carcinoma 3. The student should relate risk factors as genetic influence and the inherent dangers of sun exposure and tanning booths. 5 Aug.31, 2009 7. Infections of the Skin Text: Harrison’s Chapter 53 A. Viral Diseases OBJECTIVES Regarding the following, the student should be able to: 1. Recognize and define the pathogenesis. 2. Establish the diagnosis. 3. Assess and individualize the treatment. a. Erythema Infectiosum/5ths disease/ slapped cheek i. Red Flags 1. Prodrome of flu-like symptoms followed by “slapped cheek” appearance 2 days later. Few days later reticulated erythematous rash on trunk, lasting about 1 week. 2. Can recur for weeks to months ii. Etiology 1. Parvo B-19 2. Peaks at ages 5-14 iii. Diagnosis 1. PV B19 IgG, IgM, clinical appearance iv. Treatment 1. Symptomatic v. ADULT 1. pruitus, arthopathy, fever, rash and adenopathy 2. hydrops fetalis 3. RBC aplastic crisis b. Herpangina i. Red Flags 1. Gray/White Papulovesicles with erythematous ring that ulcerate. Commonly on tonsillar fauces, palate. ii. Etiology 1. Coxsackievirus, Enteroviruses, echovirus iii. Diagnosis 1. Associated with fever, HA, cervical LAD, sore throat iv. Treatment 1. symptomatic, usually lasts 4 – 6 days v. HAND FOOT AND MOUTH DISEASE- coxsackie 6 c. Herpes Simplex (type 1) i. Red Flags 1. HSV 1 “cold sore” “fever blister” Primary gingivostomatitis Children and young adults (only seen about 1%) Fever, sore throat, painful (burning) vesicles in oral mucosa Seropositive 85 – 90%; 1/3 symptomatic 2. Recurrent Herpes Labialis Grouped vesicles on an erythematous base Virus dormant in trigeminal ganglia until reactivated Lifetime infection ii. Etiology 1. HSV 1 iii. Diagnosis 1. APPEARANCE 2. Tzanck smears 3. IgG antibody titer 4. culture iv. Treatment 1. Symptomatic 2. Oral meds: a. Acyclovir - 200 mgm 7-10 day b. Valacyclovir – 1 Gm BID x 10 days c. Famcyclovir – 250 mgm TID x 5 days 3. Topical: Denavir as effective d. Herpes Zoster- Shingles i. Red Flags- Red rash w./ papules on dermatome. Doesn’t break midline (normally) ii. Etiology 1. Herpesvirus varicellae (reactivated in system) iii. Diagnosis 1. clinical, PCR, Biopsy, Culture, Tzanck smear iv. Treatment 1. antivirals e. Herepes Simplex (Type 2) i. Red Flags- cold sore on the ex organs ii. Etiology 7 iii. Diagnosis 1. : clinical, PCR, Biopsy, Culture, Tzanck smear 2. Treatment: 3. Antiviral: Valtrex, acyclovir, famcylcovir iv. Treatment 1. Antiviral: Valtrex, acyclovir, famcylcovir f. Roseola Infantum (6ths disease, 3 day fever) i. Red Flags1. 3day of high fevers then as fever falls get morbilliform rash 2. 6 – 36 month old child) ii. Etiology 1. HHV-6 iii. Diagnosis 1. clinical iv. Treatment 1. Symptomatic, antipyretics g. Varicella- chicken pox i. Red Flags1. “Dew on a red rose petal” (red patche with raised vesicle in center…several) 2. pruritus, fever, HA, malaise ii. Etiology 1. Herpesvirus varicellae iii. Diagnosis 1. lesions at different stages spreads centripetally, culture, Tzanck smear iv. Treatment 1. Acyclovir for adults or immunocomprised, cool compresses, Sarna lotion h. Verruca i. Red Flags 1. Hyperkeratotic papules with black dots ii. Etiology 1. Spread: by touch, sites of trauma a. Human Papillomavirus, HPV b. Verruca Vulgaris – common warts HPV-2 c. Verruca Plantaris – Plantar warts HPV-1 d. Verruca Plana – Flat wars HPV-3 e. Condyloma Acuminata – HPV 6, 11, 16, 18 8 iii. Diagnosis 1. Clinical or biopsy iv. Treatment 1. Cryotherapy, Salicylic acid, excision, lasers, podophyllin, cantharidin, Candida antigen, praying, aldara etc. i. Viral exanthema i. ii. iii. iv. B. Red Flags- non Etiology Diagnosis Treatment specific viral rash Bacterial Diseases Text: OBJECTIVES Regarding the following, the student should be able to: 1. Recognize and define the pathogenesis. 2. Establish the diagnosis. 3. Identify genetic factors 4. Assess and individualize the treatment. a. Impetigo i. Red Flags1. Contagious, acute, purulent (honey colored drainage) infection of the skin. ii. Etiology 1. Non-bullous (crusted) - Group A Beta-hemolytic Strep +/- Staph 2. Bullous - Staph aureus iii. Diagnosis 1. Appearance: vesicles > pustules > crusting 2. Culture: not recommended iv. Treatment 1. Systemic- Dicloxicillin or cephalosporin 2. Topical - (Bactroban) 3. Soaks- for debridement b. Erysipelas i. Red Flags 1. Sharply demarcated erythema usually on face or extremities possible plaques and edema, 9 ii. Etiology 1. Group A Beta Hemolytic Strep. iii. Diagnosis 1. appearance, poss culture: group A strep iv. Treatment 1. antibiotics, oral or IV c. Folliculitis, etc i. Red Flags 1. infection of the hair follicles- mistaken for spider bites a. Pustule b. Furuncle i. acute tender fluctuant deep seated nodule c. Carbuncle i. multiple coalescent furuncles with multiple draining sinuses 2. Common on buttocks, back of neck, beard, back and chest ii. Etiology 1. - Staphylococcus aureus 2. Predisposing Factors-topical steroids, injury, abrasion or surgical wound iii. Diagnosis 1. Culture/apperance iv. Treatment 1. Incision and Drainage + antibiotics, culture, warm compresses d. Acne vulgaris i. Red Flags- acne-yeah ii. Etiology 1. Proliferation of propionbacterium acnes (P. acnes) in follicles 2. Hypertrophy of sebaceous gland and increased sebum (androgen) blocks the pilosebaceous units causing inflammation and rupture of the follicle iii. Diagnosis 1. Mild: papules few, more pustules, no nodules 2. Moderate: many papules and pustules, few nodules 3. Severe: several papules, pustules and nodules iv. Treatment 1. Topical benzoyl peroxide, 5-10%, daily 2. Topical tretinoin - reverses the abnormal keratinization, 2-3 weeks 3. Topical antibiotics - Erythromycin or Clindamycin 10 4. Accutane - systemic Vit A C. Superficial Fungal Diseases Text: OBJECTIVES Regarding the following, the student should be able to: 1. Recognize and define the pathogenesis. 2. Establish the diagnosis. 3. Assess and individualize the treatment. a. Tinea –RING WORM – Tinea capitis – scalp – Tinea corporis – body – Tinea cruris – groin – Tinea manus – hand – Tinea pedis – feet – Tinea unguium Onychomycosis – nail Capitis i. Red Flagsa. Alopecia with “black dots”. Erythema and scaling in an annular configuration ii. Etiology a. 3 main types of fungus i.Trichophyton ii.Microsporum iii.Epidermophyton b. Can be transmitted by direct contact, animal exposures, and fomites iii. Diagnosis a. KOH of hair b. Wood’s lamp (20%) c. Culture (Sabouraud’s medium) iv. Treatment a. Systemic antifungals 11 Corporis i. Red Flagsa. . Annular with central clearing and well defined borders. ii. Etiology a. Same as capitis iii. Diagnosis a. KOH - hyphae, culture iv. Treatment a. Topical (2-3 weeks) Oral (2-4 weeks) ONYCHOMYCOSIS i. Red Flags a. Fungi toenails ii. Etiology a. Same as capitis iii. Diagnosis a. Need to make prior to treatment b. KOH iv. Treatment a. Treatment (oral) i.Griseofulvin ii.Sporanox iii.Lamisil Manus i. Red Flagsa.Usually unilateral with bilateral feet involvement (‘two feet one hand disease’) b. Appearance: hyperkeratotic ii. Etiology a. Same as capitis iii. Diagnosis a. KOH, Cx iv. Treatment a. may require months if nails involved Pedís v. Red Flagsa. Appearance - Subclinical to severe secondary infection. Varies 12 with species. vi. Etiology a. Same as capitis vii. Diagnosis a. Appearance b. KOH c. Culture viii. Treatment a. Topical b. Oral if secondary infected c. Burrow’s solution if macerated d. Cotton socks, sandals, powders Tinea versicolor b. i. ii. iii. iv. Red Flagsa. patches of skin that don’t tan (SUNSPOTS) b. Usually on central upper trunk Etiology a. Yeast (superficial Malassezia) Diagnosis a. KOH shows spaghetti and meatballs look (budding yeast and hyphae) Treatment a. Selsun blue b. Topical and oral d. Candidiasis “yeast infection” i. Red Flags 1. Erythematous papules and plaques with satellite pustules, can involve scrotum a. diaper area in infants b. intertrigenous (rub together spots) areas in adults c. Thrush- yeast infection of mucous membranes of mouth d. Paronychia- occurs around the nails ii. Etiology 1. Candida (type of yeast) iii. Diagnosis 1. KOH/culture, pseudohyphae iv. Treatment 1. local treatment to keep area dry and topical/oral antifungals 13 September 02, 2008 8. Miscellaneous Skin Disorders Text: A. Arthropods OBJECTIVES: For the following, the student should be able to: 1. Describe the associated skin problems. 2. Identify the etiologic agent and establish the diagnosis. 3. Outline treatment and patient management. a. Scabies i. Red Flags 1. intense pruritus worse at night 2. Location - finger webs, flexor surf, genitals ii. Etiology 1. Sarcoptes Scabiei (mites) iii. Diagnosis 1. Appearance of burrow (felt pen) 2. scrapings with KOH a. Once they start scratching hard to see burrow b. Secondary to scratching pin point red dots iv. Treatment 1. Eurax daily x 5 days, repeat 1 wk 2. Continued pruritus after treatment b. Pediculosis- lice i. head (capitus) - children (hats, combs, etc.) body (corporis)- unclean setting, seams of clothing genitals (pubis) – aka crabs is sexually transmitted Red Flags 1. Itches w/o rash ii. Etiology 1. lice (pediculus humanus) iii. Diagnosis 1. appearance, 2. nits (eggs) , 3. Wood’s lamp iv. Treatment 1. Apply Nix(permethrin)cream rinse x 10 min to dry clean hair 2. “nit comb” 3. Repeat 1 wk 14 c. Tick bites Ticks are ectoparasites that act as vectors for o spirochetal, o bacterial, o rickettsial, o parasitic infections- Lyme, RMSP, Tularemia i. Red Flags 1. presence of tick, FB reaction, macules and papules ii. Etiology 1. See above iii. Diagnosis 1. presence of tick, FB reaction, macules and papules iv. Treatment 1. remove tick< 48 hr. decrease risk 2. prevention with tick spray Lyme Disease o NE, Wisconsin, Minnesota, CA o erythema migrans- large red area, inside gets clear- “bulls eye” o flu-like symptoms o Serology, Elisa Most of the time this is false positive…if you suspect just treat o Rx: doxycycline Can be given prophlatically if bite suspected d. Fire ant bites i. Red Flags1. really itchy, 2. pustules, 3. inflammation ii. Etiology1. um, really, you don’t know this? iii. Diagnosis 1. appearance iv. Treatment 1. Steroid for bad inflammation 2. Antihistamines for itching e. Spider bites Black Widow i. Red Flags 1. small local reaction 2. hours later cramps due to neurotoxin ii. Etiology 1. Venom of black widow 15 iii. Diagnosis 1. Appearance, symptoms, and hx of exposure iv. Treatment 1. IV opiods plus benzodiazepines, 2. antivenom antiserum, 3. PO muscle relaxant, 4. Ice 5. Tet tox Brown recluse i. Red Flags a. severe local reaction, rare systemic b. symptoms i. fever, n/v, weakness and myalgia c. Hemolysis d. Necrotic ulcers ii. Etiology a. BR venom iii. Diagnosis a. Appearance, exposure iv. Treatment a. RICE, Antihistamines, Dapsone b. Monitor CBC for severe bites f. Flea bites i. Red Flags 1. Around ankles usually 2. Macular to bolus in apperence 3. itchy ii. Etiology 1. Again, really? iii. Diagnosis 1. Appearance and presence of pets or indignant circumstances iv. Treatment 1. Relieve itching B. Papulosquamous and Other Miscellaneous Disorders OBJECTIVES: In regards to the following, the student should be able to: 1. Identify in terms of configuration and distribution and describe the pathophysiology. 16 2. 3. 4. Establish a diagnosis. Recognize genetic risks Identify treatment and outline a treatment plan. a. Atopic Dermatitis i. Red Flags 1. pruritic skin disorder 2. lichenification ii. Etiology 1. Unknown, strongly familial 2. Possibly co morbid with chronic staph iii. Diagnosis 1. Appearance 2. Family or personal history iv. Treatment 1. Pimecrolimus cream 2. Topical steroids 3. Antibiotics 4. Tacrolimus ointment 5. Antihistamines 6. Psychological v. Other 1. family or personal hx of hay fever, asthma, dry skin, eczema 2. Onset - early infancy, childhood or adolescence b. Contact Dermatitis i. Red Flags 1. pruritic, reactionary skin disorder 2. Irritant o nonallergic, results from chronic exposure. o dryness, scaling, fissuring, and mild inflammation 3. Allergic o requires sensitization, thus previous exposures. o 1 - 4 days after exposure - presentation varies, redness, bulla, pruritus, vesiculation, oozing, crusting, lichenification ii. Etiology 1. Exposure to irritant or allergen 2. Long line caused by scratching iii. Diagnosis 1. history, itching, locality iv. Treatment 1. removal 2. symptomatic - antihistamines, soothing lotions 17 3. 4. v. Other 1. 2. steroids treat with p.o. meds in by eyes Exthanmatous drug eruption: ampicillin Photosensitivity drug-induced (not pictured) a. Bacterium, ampicillin, etc 3. Posion Ivy a. LINEAR VESICLES b. Does not spread by fluid in vesicles c. Spreads by resin on hands, clothes, and pets c. Seborrheic Dermatitis i. Red Flags 1. GREASY, SCALY PLAQUES 2. common, chronic, scaling, erythematous, eruption ii. Etiology 1. Pityrosporum ovale (yeast), 2. Genetic 3. environmental factors iii. Diagnosis 1. Appearance 2. KOH…remember it can be yeast iv. Treatment 1. Medicated shampoos frequently (Head and Shoulders) 2. Steroid lotions or solutions 3. Ketoconazole cream or shampoo if resistant 4. IF PUSTLES TREAT FOR STAPH v. Other 1. Location - cradle cap (infants), dandruff, scalp, face, upper chest, extent varies. 2. All ages but usually adults d. Pityriasis Rosea i. Red Flags 1. lines of cleavage in Christmas tree distribution, 2-10 wks duration 2. preceded by a short lived salmon colored oval “Herald patch” ii. Etiology 1. Unknown, may be viral iii. Diagnosis 1. Christmas tree apperance 2. NEGATIVE yeast on KOH iv. Treatment 1. Control itching 2. Possibly use steroids 18 3. UVB photo therapy e. Psoriasis i. Red Flags 1. chronic, recurrent, hyper proliferative disease of skin 2. early - red macules covered with dry silvery scales 3. later - may coalesce ii. Etiology 1. unknown - 1/3 have family history, 2. freq follows strep pharyngitis infection in children iii. Diagnosis 1. Appearance 2. Family and Personal History iv. Treatment 1. keep skin moist and lubricated 2. < 20% - topical steroid, Dovonex, coal tar preparations 3. >20% - light therapy, antimetabolites, retinoids, stress management 4. Avoid b-blockers, lithium and systemic steroids v. Other 1. Presentation - joints, ext surfaces, lower back and buttocks 2. Course - remissions and exacerbations, freq preceded by trauma or strept inf - STRESS! f. Stasis Dermatitis i. Red Flags 1. Early - hyperpigmentation 2. Late - Plaques, vesicles, bullae, cellulitis 3. Later – Ulceration, fibrotic skin ii. Etiology 1. chronic venous insufficiency 2. Predisposing conditions: DM, obesity, familial, topical allergies iii. Diagnosis o Appearance and history iv. Treatment 1. Mild o Elevate o support hose o Exercise o Steroid cream 2. Ulceration 19 o o o o Duoderm (bandage to protect wounds) unna boot (ace wrap with calamine and other healing lotions) Avoid steroid creams applied to ulcer Ulcers have long healing time v. Other 1. Location: medial malleolus g. Vitiligo i. Red Flags 1. Acquired skin depigmentation due to lack of melanocytes 2. Patches of depigmented skin ii. Etiology 1. Unknown, Autoimmune? Genetic? iii. Diagnosis 1. clinical, Woods light iv. Treatment 1. Sun protection 2. Look for assoc. diseases a. Addisons Disease b. Diabetes c. etc 3. dermatologist v. Other 1. 1% of population 2. Generalized (symmetrical) and segmental (nonsymmetrical) h. Erythema Multiforme i. Red Flags 1. target lesions that begin as macules and develop vesicles in the center with cyanotic center 2. may have fever, malaise, or itching and burning…SELF LIMITING ii. Etiology 1. hypersensitivity reaction a. drugs infections b. physical agents c. pregnancy d. malignancies iii. Diagnosis 1. Clinically and history iv. Treatment 1. 1-3 wks of prednisone 40-80mg/d 2. oral acyclovir for HSV assoc. EM v. Other 1. Location: Backs of hands, palms, soles, extensor limbs, generalized. 20 Occur in crops for 2-3 wks i. Stevens-Johnson Syndrome i. Red Flags 1. vesicobullous, mucosa affecting skin, mouth, eyes, and genitals a. trunk, palms, soles 2. Preced by cough, fever, and patchy changes on chest Xray ii. Etiology 1. severe hypersensitivity reaction following drug reaction a. phenytoin, phenobarbital, sulfonamides, PCN 2. May be variant of Erythema Multiforme iii. Diagnosis 1. clinical, skin biopsy iv. Treatment 1. systemic steroids?, 2. antihistamines for itching, 3. wet cool compresses, 4. topical steroids for plagues and papules, 5. antibiotics for infections v. Other 1. Most often in children and young adults j. Urticaria- hives i. Red Flags 1. Pruritis 2. Angioedema 3. Lumps and bumps ii. Etiology 1. histamine release o Immunologic and non-immunological o Physical stimulation o Skin contact o Small vessel vasculitis iii. Diagnosis iv. Treatment 1. H1 blockers (histamine blocker) 2. H2 blockers (histamine blocker) 3. Doxepin 4. Steroids v. Other 1. Dermatographia a. Scratching skin causes red raised line i. Can write name on skin 21 b. Acute uticaria /angioedema k. Erythema Nodosum i. Red Flags 1. Nodular erythematous eruption limited to extensor side of extremtities ii. Etiology 1. Hypersensitivity reaction to antigenic stimuli associated with several diseases a. Infections*, immunopathies, malignancies, and drug therapies iii. Diagnosis 1. History and clinically iv. Treatment 1. Self limiting 2. Help symptoms a. Antinflammatory b. Cool compress c. elevation v. Other 1. Fever, malaise, arthralgia (joint pain) 2. URI (upper respiratory tract infection) precede eruption by 1-3 wks 3. 55% are idiopathic 4. Familial form 5. Females> males 6. Burns Text: OBJECTIVE: 1. Define first, second and third-degree burns. a. Superficial=1st i. ii. iii. iv. v. b. Epidermal layer only Don’t blister Red, dry, painful, blanches with pressure Cause: UV, short flash Heal: 3-6 d Superficial Partial Thickness= 2nd i. epidermis and the superficial (papillary layer) dermis are injured ii. Blisters, appear moist, red weeping, blanches with pressure iii. Painful to temp and air 22 c. Deep Partial Thickness= 2nd drgree i. All epidermal and dermal structures are destroyed including hair follicles and glandular tissue ii. Blisters, wet or waxy dry with variable color iii. Doesn’t blanch iv. Pain with pressure only d. Full Thickness= 3rd degree burns i. ii. iii. iv. Extend through and destroy the dermis Painless, usually Skin appearance is waxy white to leathery gray to charred and black Doesn’t blanch 2. Estimate degree of burn using (Rule of 9’s) a. 23 3. Recognize systemic effects of burns. 1. Burn shock w/in 24-48 hrs for major burns a. Myocardial depression b. Increased capillary permeability c. Intravascular volume depletion d. Treatment: IV crystalloids such as Ringer’s lactate (LR) 2. Smoke inhalation Note cough, singed hair, deep facial burn or blistering of oral pharynx, hypoxia 3. Infection 4. Mesenteric vasoconstriction September 04, 2009, 1:00pm 10. Office Dermatology Macule -> Patch (same thing just bigger >5mm) (problem is in dermal/ epidermal junction) Papule -> Plaque (cluster of papules) (problem is in dermis) Vesicle -> Bulla (same thing just bigger >5mm) Pustule (same as vesicle just filled with puss- yellowish, etc.) (Fluid in epidermis) Random Tidbits A cluster of vesicles on the face is Herpes Simplex Linear Vesicles= Poison Ivy/Oak Don’t call it a vesicle until you have popped one and gotten fluid out. Always do KOH on borders of rash where fungus is still fresh Scaring occurs at the junction point of dermis/epidermis…SO if they have an erosion (loss of dermis) they won’t scar. If they have an ulcer (loss of derm and epiderm) they will. Panniculus= subcutaneous Crust= scab Squamous= scale Pimples on chest= possible steroid reaction o Ask about steroid use Lichenification comes from rubbing Stria= stretch marks o Red are early stages and can be corrected o White are late stages and can’t be fixed 24