Action on Diabetes – Calderdale and Greater Huddersfield
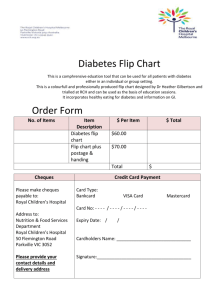
advertisement

Action for Diabetes Improving diabetes care across Calderdale and Greater Huddersfield FIVE YEAR STRATEGY 2014/15 – 2018/19 (OCTOBER 2015 REFRESH) Page 1 of 25 Calderdale & Greater Huddersfield Diabetes 5 year strategy (refresh at October 2015) ACTION ON DIABETES IN CALDERDALE AND GREATER HUDDERSFIELD STRATEGY REFRESH –OCTOBER 2015 It is now a year since we launched the Calderdale and Greater Huddersfield Diabetes Strategy; a strategy with high aspirations to ensure we give our patients the best quality care and support to manage their condition. Diabetes is one of the most difficult health challenges of our times; the steep rise in diabetes cases in recent years has been overwhelming for those charged with planning and providing healthcare services and especially in primary care. In addition, there are a significant number of people whose diabetes is undiagnosed and large numbers estimated to be pre-diabetic. We know that diabetes is manageable, but that management is not always consistent and every individual experiences it in different ways. Whilst there has been progress major gaps still exist - in support for patients and clinicians. General Practice is now carrying more responsibility for managing the condition than ever before; locally we are looking to shift some planned care from hospital settings in line with our Care Closer to Home models. In order to make this a reality, and to make the best use of unplanned care, we need to ensure that EVERY patient and EVERY clinician they have contact with, is well equipped and confident in managing the condition. The Calderdale and Greater Huddersfield Diabetes Strategy has been updated to reflect the following: 1) More recent data, where available (within the body of the strategy) 2) Recent best practice guidance and evidence (Appendix A) 3) Latest Operational Plan showing how we intend to deliver the strategy (Appendix B) Dr Judith Parker GP Governing Board member and Clinical Lead for Diabetes Greater Huddersfield CCG Dr Steven Cleasby GP Governing Body member and Clinical Lead for Diabetes Calderdale CCG Page 2 of 25 Calderdale & Greater Huddersfield Diabetes 5 year strategy (refresh at October 2015) 1. FOREWORD1 Diabetes is one of the greatest threats of the 21st century. It is estimated that more than one in 16 people in the UK has diabetes (diagnosed or undiagnosed). There are 3.9 million people living with diabetes in the UK. The cost to the people affected (and their families) is considerable, with people with diabetes 34% more likely to die earlier than their peers. Diabetes also significantly increases the risks of heart attacks, stroke, blindness, kidney failure and amputation. The statistics tell the story: Every year more than 20,000 people with diabetes die before their time in England and Wales. Diabetes doubles the risk of cardiovascular disease (heart attacks, heart failure, angina, stroke). More than 135 amputations take place each week amongst people with diabetes, and in many cases these are avoidable. Diabetes accounts for around ten per cent of the NHS budget per year; that is around £10 billion. It is estimated that 80% of these costs are incurred in treating potentially avoidable complications. In addition, one in 20 people with diabetes incurs social services costs. More than three quarters of these costs were associated with residential and nursing care. In 2014/15, 47.2m items were prescribed to treat diabetes. £868 million was spent on drugs to treat diabetes in primary care. Many people with diabetes have other long term conditions as well, and there is predicted to be a 252% increase in the number of people with multiple long-term conditions by 2050. Almost 1 in 5 people with diabetes have clinical depression and for those with anxiety and/or depression health care costs increase by around 50%. We want to commission for the people of Calderdale and Greater Huddersfield systematic, high quality, personalised support to help people to avoid or reduce their risk of diabetes and to help those with diabetes manage their condition in a way that reduces the risk of increasing ill health and the risk of developing complications. 1 Data in this section are taken from Diabetes UK ‘Diabetes: Facts and Stats’ (May 2015) Page 3 of 25 Calderdale & Greater Huddersfield Diabetes 5 year strategy (refresh at October 2015) 2. INTRODUCTION Diabetes is a serious long-term condition in which the amount of glucose (sugar) in the blood is too high because the body cannot use it properly. There are two main types of diabetes. Type 1 diabetes develops if the body cannot produce any insulin, and is more prevalent in children and young adults. It is the least common of the two main types; accounting for around 10 per cent of all people with diabetes. Type 2 diabetes is more commonly diagnosed in adults over 40, although it is increasingly being diagnosed in children and young adults. It develops when the body cannot produce enough insulin, or when the insulin that is produced does not work properly. In most cases this is linked with being overweight due to a person’s diet and lifestyle. Diabetes often leads to serious complications including heart disease, stroke, blindness, kidney disease and amputations. It is the fifth most common cause of death in the world, and accounts for an estimated 15 per cent of deaths occurring in England, and is a major cause of premature mortality with over 20,000 additional deaths each year. It is estimated that the current annual cost of direct patient care is £1 billion for people with Type 1 diabetes and £8.8 billion for those with Type 2 diabetes, and this is expected to rise to £1.8 billion and £15.1 billion respectively by 2035. Good diabetes care reduces the major risk of people dying prematurely from cardiovascular disease, as well as reducing the risk of developing serious complications, which may begin years before an actual diagnosis has been made, and it is estimated that 80 per cent of these costs are incurred in treating potentially avoidable complications. Preventing diabetes and improving diabetes care are priorities for both NHS Calderdale and NHS Greater Huddersfield Clinical Commissioning Groups (CCGs) for the reasons set out in this strategy, and both organisations are actively working together through the Calderdale and Greater Huddersfield Diabetes Network (the Network) to ensure people with diabetes and those at risk of diabetes, receive the best care and support available. Numerous health and social care services provide direct and indirect care and support to those living with diabetes, and it is the role of the Network to make sure that these services are meeting the needs of the local population in a way that improves health and social wellbeing in the most cost efficient and effective manner. 3. NATIONAL DRIVERS In 2001, a number of standards were developed through the publication of the National Service Framework (NSF) for diabetes, covering various aspects of care and prevention. In addition a number of guidelines and a set of quality standards have been produced by the National Institute for Health and Care Excellence (NICE). The Government Mandate to NHS England and Clinical Commissioning Groups places an emphasis on care and support for people with long-term conditions. Page 4 of 25 Calderdale & Greater Huddersfield Diabetes 5 year strategy (refresh at October 2015) The NHS Outcomes Framework 2013/14, developed by the Department of Health (DH), sets out the accountability process for NHS England in relation to working with CCGs. It includes a number of indicators targeted at improving diabetes care: Domain 1: Preventing people from dying prematurely • Myocardial infarction, stroke and stage five chronic kidney disease in people with diabetes. Domain 2 Enhancing quality of life for people with long term conditions • People with diabetes who have received nine care processes • People with diabetes diagnosed less than a year who are referred to structured education • People with diabetes who have an emergency admission for diabetic ketoacidosis • Complications associated with diabetes • Lower limb amputation in people with diabetes In March 2015, NHS England, Diabetes UK and Public Health England launched the National Diabetes Prevention Programme - a joint commitment to deliver at scale, an evidence based behavioural programme to support people to reduce their risk of developing Type 2 diabetes. LOCAL DRIVERS There are an estimated 26,000 people diagnosed with diabetes in Calderdale and Greater Huddersfield, and these numbers are set to increase due to rising obesity levels, an ageing population and a growing population of south Asian origin. People from south Asian and black ethnic groups have a greater chance of developing Type 2 diabetes than people from white ethnic groups. The risk of diabetes also increases with age, and in 2010 the prevalence of all types of diabetes was 0.4% for people aged 16 to 24 years, rising to 15.1% for people aged 70 to 84 years old. The individual prevalence for Calderdale and Greater Huddersfield is shown in Table 1, which also includes information on the increased risk of other diseases for people with diabetes. Page 5 of 25 Calderdale & Greater Huddersfield Diabetes 5 year strategy (refresh at October 2015) Table 1: Prevalence of diabetes in Calderdale and Greater Huddersfield and impact on other conditions. 2012/13 Calderdale Greater Huddersfield 9,786 10,791 3,395 4,297 Myocardial infarction 83 % 76 % * Stroke 19 % 25 % * Prevalence: People aged 17 and over diagnosed with diabetes2 Estimated further adults with diabetes3 Additional risk of complication for those with diabetes 4: Hospital admission relating to heart failure 81 % 73 % * *Kirklees PCT (which covered the population Greater Huddersfield and North Kirklees CCGs now cover) Statistics published by Public Health England in August 2015 estimated that in Calderdale 19,584 people were pre-diabetic, as were 39,702 people in Kirklees. Diabetes is the most common cause of lower limb amputation, with over 100 amputations carried out each week. The Yorkshire and Humber Public Health Observatory produced Diabetic Footcare Activity profiles for 2012/13 which show Greater Huddersfield and Calderdale as having higher annual rate of amputation than the England average, as illustrated in Table 2. Table 2: Rates per 1,000 population and number of lower limb amputations in people with diabetes in Calderdale and Greater Huddersfield between 2011/12 and 2013/14 compared to England average5 Major amputations Minor amputations Calderdale Greater Huddersfield England average 1.1 1.1 0.8 (31) (36) 2.4 2.7 (69) (88) 1.8 2 Source: Quality and Outcomes Framework 2012/13 Source: APHO Diabetes Prevalence Model 4 Source: National Diabetes Audit 2011/12 5 Hospital Episode Statistics and Quality and Outcomes Framework 3 Page 6 of 25 Calderdale & Greater Huddersfield Diabetes 5 year strategy (refresh at October 2015) It is also worth noting the changes in the amputation rates from 2009/12 to 2011/14. For Calderdale: the major rate has dropped by 0.1, and the minor rate has not changed. For Huddersfield: the major rate is unchanged; the minor rate has increased by 0.7. Diabetes is also the second most common cause of blindness in adults of working age, accounting for 14.4% of certifications of blindness between 1st April 2009 and 31st March 20106 Another major complication relates to kidney failure, which is one of the most severe and life threatening complications of diabetes. It is more common in people who have high blood pressure and it is important to undertake regular checks of kidney functions, while good weight management and other informed lifestyle choices help to maintain good glucose levels. Additionally, gestational diabetes is a type of diabetes that arises during pregnancy and women with diabetes are five times as likely to have a stillborn baby and three times more likely to have a baby that dies prematurely. Good diabetes care reduces the major risk of people dying prematurely from cardiovascular disease, as well as reducing the risk of developing serious complications, which may begin years before an actual diagnosis has been made. It is essential that people with diabetes are managed in a way that attempts to reduce the above complications and mortality rates and a key area in achieving this is through good management of the care processes delivered through primary care. 4. LOCAL SPEND AND ACTIVITY Primary care In Calderdale there are no specific services commissioned from primary care for Diabetes – GP practices and pharmacies provide different levels of care according to their expertise/interest as part of their core work. In Greater Huddersfield, thirteen practices provide a community service for diabetes injectable therapies. 6 A comparison of the causes of blindness certifications in England and Wales in working age adults (16-64 years), 1999-2000 and 2009-10 Page 7 of 25 Calderdale & Greater Huddersfield Diabetes 5 year strategy (refresh at October 2015) In terms of primary care data, the National Diabetes Audit focuses on the achievement of the following eight care processes7: • Blood glucose (HbA1c) • Blood pressure • Cholesterol • Eye check (retinopathy screening) • Foot check • Kidney function (urinary albumin) • Kidney function testing (blood) • Weight check (BMI) • Smoking status check The data from the 2012/13 Audit (latest available) demonstrates that there is a significant variation between GP practices in the achievement of care processes. Several examples are show in the table below. Table 4. Percentage checked and within target 2012/13 by process8 Calderdale Greater Average for (Individual practice Huddersfield similar CCGs range) (Individual practice England average range) HbA1c Cholesterol Blood pressure 65% 64% (50% – 73%) (44% - 77%) 76% 72% (59% - 88%) (55% - 86%) 68% 63% (44% - 92%) (31% - 83%) 61% 60% 73% 73% 68% 67% Note. The HbA1c figures should be treated with caution as a national data quality issue has been identified in relation to some submissions. This is in the process of being resolved. 77 These are eight of the nine processes recommended by NICE – the ninth, eye screening, is not currently included in the National Diabetes Audit 8 National Diabetes Audit 2011/12 Page 8 of 25 Calderdale & Greater Huddersfield Diabetes 5 year strategy (refresh at October 2015) More recent primary care diabetes data can be accessed through the Quality and Outcomes Framework (QoF), which was introduced in 2003 as part of the contracting process with GP Practices. Data is collected and published annually at practice level and Primary Care Trust (and now CCG) level. The latest data are at the link below, and show a significant variation in performance between individual practices. http://qof.hscic.gov.uk/ Prescribing Spend on prescribing for diabetes items in 2012-13 was £2.9m for each CCG. The average spend per adult with diabetes was slightly higher than the England average for Calderdale and slightly lower for Greater Huddersfield. Secondary care Most hospital activity for people from Calderdale and Greater Huddersfield takes place with Calderdale & Huddersfield NHS Foundation Trust. Table 3 sets out forecast expenditure and activity for 2013/14 for the two CCGs relating to different types of hospital care. Table 3: Forecast expenditure and activity 2013/14 Adults (over 18 years) Calderdale Greater CCG Huddersfield CCG Exp £000 £218 108 Inpatients Spells 130 106 Exp £000 560 465 Outpatients Spells 4,630 3,864 Exp £000 11 9 Accident & Emergency Spells 91 77 Paediatrics (18 years and under) Calderdale Greater CCG Huddersfield CCG 27 36 26 36 51 83 352 618 0.2 2 2 22 Data descriptions Inpatients - Inpatient spells where spell primary diagnosis relates to diabetes Outpatients - Mandatory Outpatient attendances - assigned to 300 - General Medicine which include Diabetes & Endocrine clinics A & E Inpatient and Outpatient Spells – patients who have had an A & E attendance where primary diagnosis is related to Diabetes Page 9 of 25 Calderdale & Greater Huddersfield Diabetes 5 year strategy (refresh at October 2015) 5. ‘HOUSE OF CARE’ APPROACH The CCGs support a ‘House of Care’, approach (described by the King’s Fund9) to ensuring quality of life for people with long-term conditions, including diabetes. This approach, which is set out in Figure 1 was developed initially for patients with diabetes specifically, and centres around a care planning process, where people with long-term conditions, their carers and health professionals work in partnership to agree goals and outcomes, taking a whole life approach that goes beyond the symptoms or a single condition. The Diabetes Network adopted this approach (Figure 2) to demonstrate the dependencies within the programme and how these support the strategy. Figure 1 – National ‘house of care’ model The ‘House of Care’ has a solid foundation built on the commissioning cycle, pillars of patient empowerment and clinical collaboration, and a roof composed of guidance, tools and resources. The ‘House’ falls down if all the constituent parts are not strong and working together; each part needs equal and sustained focus. 9 King’s Fund Delivering better services for people with long-term conditions: building the house of care (2013) Page 10 of 25 Calderdale & Greater Huddersfield Diabetes 5 year strategy (refresh at October 2015) The Calderdale and Greater Huddersfield CCGs and the Diabetes Network have agreed to develop this strategy and a more detailed operational plan to steer the development and improvement of local diabetes care in the future. We have used the ‘House of care’ approach, localised to include the priority areas, set out in Figure 2 below. Figure 2: Local ‘house of care’ model Specialist diabetes services Foot Care Education and training Primary care Supported self-care Prevention High quality care and support Excellent patient/carer experience Calderdale and Greater Huddersfield Diabetes Network ‘Action on Diabetes’ Strategy Local prescribing strategies Operational plans Page 11 of 25 Calderdale & Greater Huddersfield Diabetes 5 year strategy (refresh at October 2015) 6. LOCAL MODEL OF CARE The local model of care is shown below in Figure 3. This model supports the priority areas as described above in the ‘House of Care’. Hospital Specialist service Foot care Community specialist service Primary Care Supported self-care Education and Training Figure 3. Local model of diabetes care in Calderdale and Huddersfield Prevention The levels can be described as follows: Prevention: focuses on support to pursue healthy lifestyles as a means of preventing or reducing risk of disease. Supported self-care: focuses on self-care where the individual, as much as possible, manages his/her health and wellbeing. This will mean that people are able to take more control of their lives, feeling involved, supported, confident and resilient. Primary care: focuses on primary and community health and social care services and general management of conditions to maintain stability and reduce the risk of exacerbation. Community specialist service: focuses on community based specialist services, which support and maximise the capacity of multidisciplinary professionals to quickly manage early exacerbation that cannot be managed in level 3, with the aim of moving care back down to level 3. Page 12 of 25 Calderdale & Greater Huddersfield Diabetes 5 year strategy (refresh at October 2015) Hospital specialist service: focuses on highly specialised hospital based clinical input which must be delivered in a hospital environment for reasons of patient complexity, safety and/or economies of scale. Services within this model will: empower and support patients to control their own condition and self care provide co-ordinated care with effective communication to provide smooth transitions between sectors deliver proactive care to reduce risks, complications and unnecessary hospital admissions/ attendances be commissioned on use of competencies, not roles, to deliver care involve multidisciplinary working provide safe use of all diabetic medicines including insulin provide early information and specialist support for pre-conception and pregnancy in women with diabetes ensure smooth transition into adult services for children and young people with diabetes ensure dignity and respect Every service commissioned by the CCGs will support/empower people to move to the lowest level possible in the pyramid during every episode of care, giving them the highest level of appropriate control of their care. This model of care will also support the wider work of the CCGs in developing their Care Closer to Home models. 7. PRIORITIES FOR SERVICE IMPROVEMENT The Network held an event in January 2014 with over 60 people from key stakeholder groups to identify the priorities for service improvement across the patch. The six priorities identified and these are described below form the pillars of our local ’House of Care’ (see above), along with the vision relating to each. Page 13 of 25 Calderdale & Greater Huddersfield Diabetes 5 year strategy (refresh at October 2015) Prevention The best way to avoid Type 2 diabetes is to follow a healthy lifestyle. Two key factors that impact on risk of conditions such as diabetes are being overweight or obese and being physically inactive. The CCGs and Public Health will work in partnership to ensure services are available to support people to lose and manage their weight better and to help people become more physically active. Better local use will also be made of the NHS check to help identify people at increased risk of cardiovascular diseases and diabetes and to use it as a lever to promote local health improvement services and encourage patients to attend the services on offer. For individuals not attending services, the CCGs and Public Health will work to make sure that relevant and easy to understand information is available for individuals who may be willing to make some small changes to their lifestyle in order to have a big impact on their health. Supported self-care/education It is very important for patients to be aware of and involved in managing their own condition. They will be encouraged and supported to take part in screening programmes such as diabetic retinopathy10 and footcare screening. The CCGs will expect commissioned services to involve patients/carers in care planning, focusing on what the patient is able to do for themselves, and will provide and develop a variety of opportunities for education for patients/carers, using a range of media. The CCGs want to see a personalised holistic care plan for each person with diabetes developed and agreed in partnership with their clinical team through the careplanning process including action to be taken when problems arise. This care plan will be shared with relevant people to ensure prompt, consistent action. The CCGs want to see all those people with diabetes who use insulin as a treatment being supported to use it safely – both in and out of hospital, including all pregnant women with diabetes being supported to minimise risk to their babies. 10 The Diabetic Retinopathy Screening Programme is a nationally commissioned programme, and therefore does not form part of this strategy Page 14 of 25 Calderdale & Greater Huddersfield Diabetes 5 year strategy (refresh at October 2015) Education/training Health care professionals play a critical role in caring for and supporting people with diabetes. To do this in the most effective way they need to receive accredited relevant training and opportunities for development in relation to diabetes. The CCGs will ensure that systems are in place to enable this, examples being taught courses, mentorship, etc. Primary care Most diabetes care can be delivered through primary care; however, at present there is significant variation across practices. The vision of the Network is for all GP practices to be upskilled to deliver a specific level of care, utilising the skills and experience of the workforce within and outside each practice. The eight care processes set out in NICE guidance will be undertaken with each patient with diabetes. Comprehensive annual health checks will be undertaken, covering other co-morbidities where appropriate, and reviewing all medicines being prescribed. GP practices will also be encouraged to identify their patient cohorts who are most at risk of admission to hospital, using a multi-disciplinary approach to work with health and social care professionals to deliver an enhanced care package for these patients. Foot Care It has been shown that regular foot checks can identify patients at risk of diabetic foot disease and subsequent amputation. In future all patients with diabetes will receive an annual foot check at which their risk status will be identified, and appropriate care/review provided. Health and social care staff will be trained in awareness of foot disease and action to be taken, as will patients/carers/families Specialist diabetes services Those with more complex needs requiring specialist care/support to help them manage their condition will be cared for by specialist services delivered in the community where possible; where this is not possible the diabetes patient will be cared for by a specialist hospital team. Both these services will use the skills of the workforce in the most appropriate way. Page 15 of 25 Calderdale & Greater Huddersfield Diabetes 5 year strategy (refresh at October 2015) 8. MEASURING PROGRESS National and local metrics for each priority area will be used or developed by the Network and progress against them will be monitored regularly through the Network, with a highlight report being submitted to each meeting. Progress will also be reported back through the CCG governance and contract management structures. Page 16 of 25 Calderdale & Greater Huddersfield Diabetes 5 year strategy (refresh at October 2015) APPENDIX A RECENT GUIDANCE AND BEST PRACTICE The following guidance and best practice documents have been produced since the original publication of the strategy. Five Year Forward View This document was published on 23 October 2014 and sets out a vision for the future of the NHS. 2015/16 NHS Outcomes Framework The 2015/16 NHS Outcomes Framework, which sets out how NHS England will work with CCGs, includes a number of outcomes relating to long term conditions including diabetes. https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/385749/NHS_Outcomes_Fr amework.pdf Diabetes State of the Nation: Challenges for 2015 and beyond In March 2015, Diabetes UK published ‘The State of the Nation: Challenges for 2015 and Beyond’, which sets out fifteen healthcare essentials for people with diabetes, with actions to be taken by organisations and individuals to put them in place. The healthcare essentials are set out at Appendix C. The Network will use this report to guide its work. https://www.diabetes.org.uk/Documents/About%20Us/What%20we%20say/State%20of%20the%20nation %202014.pdf NICE guidance NICE guidance on the management of Type 2 diabetes (CG87) has been updated, and was reissued in December 2014. http://www.nice.org.uk/guidance/cg87/resources/guidance-type-2-diabetes-pdf NICE guidance about gestational diabetes has also been updated and reissued https://www.nice.org.uk/guidance/ng3 Type 1 diabetes in adults: diagnosis and management has been updated and reissued https://www.nice.org.uk/guidance/ng17 Type 1 diabetes in children and young people: diagnosis and management has been updated and reissued https://www.nice.org.uk/guidance/ng18 Page 17 of 25 Calderdale & Greater Huddersfield Diabetes 5 year strategy (refresh at October 2015) Diabetic foot problems: prevention and management has been updated and reissued. https://www.nice.org.uk/guidance/ng19 Diabetes in pregnancy: management of diabetes and its complications from preconception to the postnatal period has been updated and reissued https://www.nice.org.uk/guidance/ng3 NICE pathway for prevention of Type 2 diabetes http://pathways.nice.org.uk/pathways/preventing-type-2-diabetes What to expect at your annual foot check This leaflet was produced by Diabetes UK in May 2015. It provides a checklist of the steps that a foot check should include, a space to record the date of the check and the outcomes, as well as a useful list of the signs to look out for that may indicate a foot problem. https://www.diabetes.org.uk/Documents/What-to-expect-at-annual-foot-check.pdf Quality and Outcomes Framework 2014-15 The Quality and Outcomes Framework (QOF) is the annual reward and incentive programme detailing GP practice achievement results. http://qof.hscic.gov.uk/ Page 18 of 25 Calderdale & Greater Huddersfield Diabetes 5 year strategy (refresh at October 2015) APPENDIX B CALDERDALE AND GREATER HUDDERSFIELD DIABETES STRATEGY REFRESH OPERATIONAL PLAN 2015-2017 Where are now? Where do we want to be? How we are going to get there? Lead Timescale Make information on local services/support available through various media Communications Team November 2015 Identify action to be taken to address gaps/issues Public Health/CCGs December 2015 Identify areas to target for improving uptake of health checks, using local data, and develop action plan Public Health To be confirmed Develop local approach to motivation segmentation and action plan Public Health To be confirmed Prevention Local public health strategies Food, Activity and Weight Plan Weight Management Services Better Living Programme (Calderdale) Practice Activity and Leisure Scheme (Kirklees) Huddersfield Giants Exercise Programme NHS Health Checks for people aged 40 – 74 Food programmes (Food for Life partnership) – community, schools, hospitals Active Travel (Calderdale) e.g. cycling, safer walking Stop smoking services Identify people most at risk or with most causal factors with aim of reducing conversion to diabetes Increase diagnosis rates to reduce gap between estimated prevalence and number diagnosed Page 19 of 25 Calderdale & Greater Huddersfield Diabetes 5 year strategy (refresh at October 2015) Where are now? Where do we want to be? Supported self-care – structured education Co-production/ DESMOND (Newly empowerment of people diagnosed and Foundation in Greater with diabetes Huddersfield, Newly People with diabetes can Diagnosed in access a suite of supported Calderdale) self-management education, linked to DAFNE motivation segmentation X-Pert Programme in Urdu and Punjabi (Calderdale) Safer Ramadan Expert Patients Programme (Kirklees) How we are going to get there? Lead Timescale Review capacity and content of programmes, identify any gaps CCGs/Education providers November 2015 Take action to address them CCGs December 2015 Review recommendations from All Party Parliamentary Group on Diabetes report on Structured Education and identify actions to be taken. Network January 2016 Map local and national supported self-care services/support CCGs/Public Health November 2015 Communications Team December 2015 Identify action to be taken to address gaps/issues CCG December 2015 Evaluate services/support and use the outcomes to inform commissioning CCGs Ongoing Work with Practice Participation Groups to help inform the diabetes agenda Engagement and Quality Teams Ongoing Develop community champions programmes Calderdale CCG Greater Huddersfield CCG January 2016 March 2016 (tbc) Supported self-care – services and support Calderdale Diabetes UK Support Group Honeyzz (Greater Huddersfield) Self care handbook (Kirklees) Improving Access to Psychological Support Buddies (Greater Huddersfield) Health Trainers (Kirklees) Better Living Programme (Calderdale) Co-production/ empowerment of people with diabetes Everyone with diabetes has a co-created care plan People with diabetes can access a suite of supported self-management education, linked to motivation segmentation People with diabetes can access peer support in the community Make information on supported self-care services/support available through a variety of media Page 20 of 25 Calderdale & Greater Huddersfield Diabetes 5 year strategy (refresh at October 2015) Where are now? Education and training Free resources from Diabetes UK to help with skills, knowledge and confidence No specific programme of education and training around diabetes for staff. No specific education/training standards for GPs and primary care staff Where do we want to be? Skilled, knowledgeable and confident workforce, with workforce development programmes to continue learning and development planned and available to all who need them. A skilled, confident and competent care home workforce Inconsistency around care and treatment of individuals with diabetes living in care homes How we are going to get there? Lead Timescale Research models of psychological support and identify transferable work and learning to inform future services and commissioning Network members and others with interest in diabetes January 2016 Research models of support for people with severe mental health/alcohol/drugs issues Diabetes specialist team/Network January 2016 Research the use of technology for supported self-care. Feed that information into the Network for further dissemination Network/specialist staff/patients and others with interest January 2016 Explore possible funds for the provision of training e.g. pharma Greater Huddersfield CCG November 2015 Develop and agree education/ training standards for GPs and primary care staff. Source and agree funding routes Greater Huddersfield CCG December 2015 and ongoing Work with Huddersfield University on the development of a rolling programme of education for all GP and primary care clinicians CCGs/providers/ Clinical Network December 2015 Work with Continuing Care Teams and with Local Authority contracting teams to support and encourage training and education through, for example, the session run in conjunction with the Diabetes Clinical Network CCGs Ongoing Page 21 of 25 Calderdale & Greater Huddersfield Diabetes 5 year strategy (refresh at October 2015) Where are now? Where do we want to be? How we are going to get there? Lead Timescale Develop improvement plans for the implementation of the nine care processes CCGs December 2015 Implement the Level 3 diabetes service in Calderdale with specialist training/mentoring/ support Calderdale CCG/CHFT December 2015 Incorporate primary/community care functions including collaborative care planning into care closer to home models CCGs/Locala/CHFT December 2015 (Greater Huddersfield) June 2016 (Calderdale) Research the use of technology to support clinicians Network January 2016 Feed in learning from Year of Care work CCGs/providers Ongoing People with diabetes receive information about foot care and prevention/identification of foot problems Development of business case to change the criteria for access to podiatry so that ‘at Risk’/ high risk Diabetic patients can be seen more rapidly. Greater Huddersfield CCG To be confirmed Review future capacity and demand in Calderdale Calderdale CCG November 2015 Fewer admissions to hospital for a diabetic foot problem Development of foot protection assurance framework Strategic Clinical Network December 2015 Primary/community care Variation in level of care received by people with diabetes Improved delivery of and outcomes from care processes Levelling off of achievement around QOF diabetes targets Increased skills, knowledge and confidence of workforce Care Closer to Home models being developed Diabetes injectable therapies community service in 13 GP practices in Greater Huddersfield (ending Sept) Keyworker function (Diabetes Specialist Nurses – formal, Practice Nurses – informal) Forthcoming changes in the way of delivering social care Foot care Provision of foot screening for all patients with diabetes in Calderdale by podiatry service Foot screening undertaken in primary care in Greater Huddersfield by nurses or Health Care Assistants Page 22 of 25 Calderdale & Greater Huddersfield Diabetes 5 year strategy (refresh at October 2015) Where are now? Foot care (continued) Foot Protection Team function provided by podiatry in both areas Where do we want to be? How we are going to get there? Lead Timescale Fewer amputations Evidenced learning from Root Cause Analysis of samples of amputations CHFT/Locala To be confirmed Develop a process and template for Root Cause Analysis of samples of amputations CHFT/Locala To be confirmed Develop community services as part of the care closer to home model Greater Huddersfield CCG/Locala December 2015 Develop community services as part of the care closer to home model Calderdale CCG/ CHFT June 2016 Ensure that people with diabetes in hospital are identified on admission so they can receive specialist diabetes input and receive a foot check as part of their overall care CHFT Ongoing Introduce wi-fi system to enable review of HbA1c results for self-testing by patients with diabetes in hospital (with review of results by clinician) CHFT To be confirmed Recruit additional hospital diabetes specialist nurse CHFT Multidisciplinary Foot Team (consultant, podiatrist, vascular, DSN) on each site Specialist services - community Community Diabetes More care taking place in Specialist Nurses (Greater the community (therefore Huddersfield) reduced outpatient appointments) No formal community diabetes specialist services in Calderdale Specialist services - hospital One hospital diabetes specialist nurse covering both sites Patients encouraged and supported to self-manage while in hospital CQUIN around supporting people with diabetes in hospital to manage their own condition To be confirmed Page 23 of 25 Calderdale & Greater Huddersfield Diabetes 5 year strategy (refresh at October 2015) Where are now? Where do we want to be? How we are going to get there? Lead Timescale Look into having a local ‘service champion’ from Diabetes UK to link between the Network and the community Network November 2015 Commissioners/ Engagement and Comms Teams Ongoing Arrange a further stakeholder event and ensure strong representation from people with diabetes and their families/carers Network January 2016 Identify and facilitate opportunities for people with diabetes and their families/carers to be involved in specific service improvement projects Network Ongoing Map health inequalities for Network to use to target efforts Public Health To be confirmed Look at ways to work with community pharmacies on diabetes Network December 2016 Look into the application of near patient testing for HbA1c CCGs January 2016 Patient/carer engagement and involvement No formal arrangement for patient/carer engagement and involvement People with diabetes and their families/ carers are engaged in discussions about local diabetes services and support No direct patient/carer input into the Network Develop an engagement and communication strategy, including co-production Reducing health inequalities Lots of data relating to health inequalities Commissioners have a good understanding of the needs of their populations, and are able to identify where efforts need to be targeted, so that health inequalities are reduced Medicines Management Community Community pharmacies pharmacies providing supporting and signposting varying degrees and people with types of support to diabetes/families/carers people with diabetes and their Technologies/ processes families/carers considered for implementation where appropriate Page 24 of 25 Calderdale & Greater Huddersfield Diabetes 5 year strategy (refresh at October 2015) APPENDIX C Diabetes UK – Healthcare essentials for everyone with diabetes 1. Get your blood glucose levels (HbA1C) measured at least once a year. This will measure your overall blood pressure control and help you and your healthcare team to set a target. 2. Have your blood pressure measured and recorded at least once a year, and set a target that is right for you. 3. Have your blood fats, such as cholesterol, measured every year. You should have a target that is realistic and achievable. 4. Have your eyes screened for signs of retinopathy every year. 5. Have your feet checked. The skin, circulation and nerve supply of your feet should be checked annually. You should then be told if you have any risk of foot problems and how serious they are. 6. Have your kidney function monitored annually. This should involve two tests: a urine test for protein and a blood test to monitor kidney function. 7. Have your weight checked and your waist measured to see if you need to lose weight. 8. Get support if you are a smoker, including advice and support on how to quit. 9. Engage in care planning discussions with your healthcare team to talk about your individual needs and set targets. 10. Attend an education course in your local area to help you understand and manage your diabetes. 11. Receive care from a specialist paediatric team if you are a child or young person. 12. Receive high quality care if admitted to hospital from specialist diabetes healthcare professionals, regardless of whether or not you have been admitted due to your diabetes. 13. Get information and specialist care if you are planning to have a baby as your diabetes control has to be a lot tighter and managed very closely. You should expect care and support from specialists at every stage, from preconception to postnatal care. 14. See specialist diabetes healthcare professionals to help you manage your diabetes, such as podiatrists, ophthalmologists and dietitians. 15. Get emotional and psychological support. Being diagnosed with diabetes and living with a long-term condition can be difficult and you should be able to talk about issues and concerns with specialist healthcare professionals. Page 25 of 25 Calderdale & Greater Huddersfield Diabetes 5 year strategy (refresh at October 2015)