Aortic Dissection
advertisement

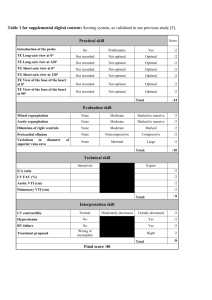
2/9/2016 1 CHEUNG AT UPDATE IN ISCHEMIC MITRAL VALVE DISEASE Albert T. Cheung, M.D. Department of Anesthesiology and Critical Care University of Pennsylvania Philadelphia, PA Learning Objectives: 1. List the effects of ventricular remodeling in patients with ischemic mitral regurgitation (IMR) and differentiate IMR from other mitral valve (MV) pathologies. 2. Identify the latest advances in diagnosis and nonsurgical management of IMR. 3. Describe the results of IMR trials evaluating MV repair, MV replacement, or CABG alone for the treatment of IMR. The Left Ventricle (LV) in Ischemic Mitral Regurgitation (IMR): By definition, IMR is mitral regurgitation caused by ischemic disease affecting the left ventricle. In contrast to IMR, degenerative mitral regurgitation is mitral regurgitation caused by diseases that specifically affect the mitral valve apparatus. Examples of degenerative mitral regurgitation include myxomatous disease, rheumatic disease, mitral valve prolapsed, or flail leaftet from a ruptured chordae tendinae. Functional mitral regurgitation (FMR) is a term that is sometimes used interchangeably with IMR to describe pathophysiologic conditions that cause mitral regurgitation through the same mechanisms as IMR with the exception that they are a consequence of non-ischemic diseases of the left ventricle. Examples of conditions that result in FMR include chronic atrial fibrillation, non-ischemic cardiomyopathy, or eccentric LV hypertrophy from chronic aortic regurgitation. IMR can be further subclassified as acute or chronic. Acute IMR may be the consequence of papillary muscle rupture from infarction or acute myocardial ischemia causing papillary muscle dysfunction, LV segmental asynchrony, or LV chamber dilation. Chronic IMR is the consequence of ischemic cardiomyopathy producing alterations of the MV apparatus that impair leaflet coaptation and is typically associated with heart failure. Examples of alterations that lead to IMR include MV annular dilation, MV annular flattening, MV leaflet tethering, and papillary muscle scarring and fibrosis. Existing clinical experience suggests that IMR affects between 13% to 50% of patients who have had myocardial infarctions and more than 50% of patients with LV ejection fraction less than 40% from ischemic heart disease. Survival and prognosis in patients with IMR is a function of the severity of MR. Even mild MR in patients with ischemic heart disease is associated with decreased long-term survival. 2/9/2016 2 CHEUNG AT Advances in the Diagnosis of IMR Doppler echocardiography is the conventional method for detecting and grading the severity of mitral regurgitation based on characteristics of the mitral regurgitant jet such as the regurgitant orifice area, vena contracta width, and proximal isovelocity surface area radius. However, Doppler echocardiographic assessment of IMR can be problematic because the severity of mitral regurgitation in this condition is dynamic and may vary according to the hemodynamic state of the patient. For example, severe mitral regurgitation in a patient with IMR caused by papillary muscle dysfunction or displacement may only manifest in the presence of myocardial ischemia. In another common scenario, a patient with significant IMR while in decompensated heart failure or during exercise stress testing may only manifest mild mitral regurgitation during intraoperative assessment under general anesthesia. For these reasons, Doppler echocardiography alone is often inadequate to fully assess the severity of FMR or IMR. The sensitivity of Doppler echocardiography for diagnosis of functional mitral regurgitation can sometimes be improved by provocative testing. Exercise, volume expansion, and vasopressor administration are sometimes necessary to elicit mitral regurgitation that can then be detected and graded by Doppler echocardiography. Eliciting patient symptoms of flash pulmonary edema, episodic dyspnea on exertion, or repeat hospitalizations for congestive heart failure in the preoperative history is important for assessing the risk of IMR. Because IMR is the consequence of left ventricular dysfunction, the first step in the echocardiographic assessment of the disease is characterization of left ventricular size, shape, and function. Left ventricular volume is increased and left ventricular ejection fraction decreased in patients with FMR or IMR compared to controls. In patients with FMR associated with ischemic or non-ischemic cardiomyopathy, left ventricular enddiastolic volume index (170 ml/m2 v. 60 ml/m2) and end-systolic volume index (135 ml/m2 v. 25 ml/m2) was more than twice normal and left ventricular ejection fraction was less than half normal (30% v. 65%). In addition, some studies have demonstrated an increase in the spherical shape of the ventricle as measured by the cavity diameter to length ratio in patients with IMR or FMR. In ischemic mitral regurgitation, other echocardiographic features that may be present include ruptured papillary muscle or left ventricular segmental wall motion abnormalities in the segments adjacent to the anterolateral or posteromedial papillary muscles. Both clinical and experimental models of IMR have demonstrated mitral annular enlargement and annular flattening. Because the mitral valve annulus is non-circular and non-planar, annular dimensions cannot be easily characterized based on geometric assumptions. In studies performed using 2-dimensional echocardiography, mitral annular diameter was larger in IMR, averaging 20% to 30% larger than controls (35 mm v. 28 mm). To provide a more precise description of mitral annular size, 2-D echocardiography can be used to provide the septal-lateral diameter of the mitral annulus (from the midesophageal long-axis view) together with the transverse (commissure-commissure) diameter (from the mid-esophageal mitral valve commissural view). Recent developments in 3-dimensional echocardiography have made it feasible to measure 2/9/2016 3 CHEUNG AT precisely mitral annular dimensions, mitral annular circumference, and mitral annular height. Mitral annular height provides a measure of the degree of alteration or flattening of the normally non-planar saddle-shaped annulus that occurs in association with functional mitral regurgitation. Normally, the left atrial surface of the leading edges of the anterior and posterior leaflets of the mitral valve coap below the plane of the mitral valve annulus within the left ventricular cavity. Normally, the contact distance between the anterior and posterior mitral valve leaflets at their leading edges during systole is 1-2 mm in length. Normally, the maximum distance between the point of coaptation and the plane of the mitral valve annulus is less than 1.0 cm. In IMR, echocardiographic features of leaflet tethering include decreased contact distance between the anterior and posterior mitral valve leaflets along their coaptation (≤ 1 mm), increased depth of coaptation below the plane of the mitral valve annulus (≥ 0.9 cm), and a steeper angle formed between the anterior (≥ 25˚) and posterior leaflets (≥ 45˚) with the plane of the mitral valve annulus in mid-systole. Tethering of the anterior leaflet at the site of a secondary chord produces an acute bend at the site of attachment between the chord and the body of the anterior leaflet in systole. Other parameters of leaflet tethering include tenting area and tenting volume measured using 2D and 3-dimensional echocardiography. When mitral regurgitation is detected using Doppler color flow imaging, characterizing the location and direction of the regurgitant jet is useful for verifying the clinical significance of the anatomic alterations associated with ischemic mitral regurgitation. Bileaflet tethering will produce a central regurgitant jet along the line of coaptation. Asymmetric tethering of the posterior mitral valve leaflet will produce an eccentric mitral regurgitant jet directed away from the anterior mitral valve leaflet and overriding the tethered posterior leaflet. A classification system based on leaflet motion devised by Carpentier is often used to characterize the mechanism of mitral regurgitation. In this classification, type 1 lesions have normal leaflet motion with mitral regurgitation caused by annular dilation or leaflet perforation. Type II lesions are characterized by excessive leaflet motion with mitral regurgitation caused by leaflet prolapse or flail (ruptured chordae). In type III lesions, mitral regurgitation is caused by leaflet restriction such as fibrosis in rheumatic heart disease or by leaflet tethering in cardiomyopathy Type III lesions can be further subclassified as Type IIIa (diastolic tethering) or Type IIIb (systolic tethering). Type I lesions typically cause a central mitral regurgitant jet, type II lesions cause an eccentric jet directed away from the diseased leaflet segment, and type III lesions cause a regurgitant jet overlying the tethered leaflet. IMR can be a consequence of Type I, II, or IIIb lesions. Chronic IMR is typically associated with annular dilation (Type I) and systolic leaflet tethering (Type IIIb). Acute ischemic mitral regurgitation caused by papillary muscle rupture would be classified as a Type II lesion. 2/9/2016 4 CHEUNG AT Clinical Trials in the Surgical and Non-surgical Management of IMR Consensus guidelines recommend mitral valve repair for patients with severe ischemic or functional mitral regurgitation, but evidence and expert opinion is controversial when the severity of ischemic mitral regurgitation is mild to moderate. At present, several randomized controlled trials have been performed to address this question. Even though the existing trials have not been adequately powered to demonstrate a mortality benefit, results suggest that both surgical or nonsurgical correction of IMR results in functional improvements. Although it is widely recognized that the efficacy of mitral valve repair is controversial, the basis for recommending mitral valve repair is that ischemic or functional mitral regurgitation is associated with symptomatic heart failure and poor outcomes with an average 50% survival in 5 years. Further arguments to support the decision for mitral valve repair include mitral regurgitation contributes to the progression of heart failure, mitral regurgitation contributes to the symptoms of heart failure, mitral valve repair is the best treatment option available for this condition, and that mitral valve repair produces excellent echocardiographic results in the short-term. For these reasons, mitral valve repair can be justified in patients with severe mitral regurgitation detected preoperatively combined with pathological features such as left ventricular dilation, reduced left ventricular ejection fraction, and mitral leaflet tethering detected by intraoperative TEE even when the intraoperative TEE examination reveals only mild to moderate mitral regurgitation. In addition, anatomic and pathophysiologic alterations associated with ischemic mitral regurgitation can be used to justify mitral valve repair even if the Doppler examination only reveals mild to moderate mitral regurgitation. Arguments against surgical treatment of IMR include the incremental risk of MV operation and the risk of recurrent mitral regurgitation. Existing clinical reports indicate that improvements in surgical and perioperative management have decreased the risk associated with MV surgery in patients with ischemic heart disease such that there is little incremental risk above the risks associated with coronary revascularization alone. If ischemic or functional mitral regurgitation is associated with severe anatomic pathophysiologic alterations, an argument can be made to perform mitral valve replacement because mitral valve repair may not provide long-term durability and freedom from recurrent mitral regurgitation. A recent randomized controlled trial comparing mitral valve repair to mitral valve replacement in patients with IMR found that the rate of recurrent moderate or severe mitral regurgitation was greater in the patients who had mitral valve repair compared to replacement (36.6% vs. 2.3%, p<0.001). Furthermore, the mortality rate, rate of major cardiac or cerebral vascular events, functional status, and quality of life was not different among the patients who had mitral valve replacement compared to those who had mitral valve repair. Arguments against mitral valve repair include the lack of randomized controlled trials that demonstrate improved survival or functional status in patients undergoing mitral valve repair for IMR, performing mitral valve repair in combination with surgical revascularization adds risk to the operation, the effectiveness of mitral valve repair is not durable and has a high rate of recurrence, and that surgical revascularization alone may correct ischemic mitral regurgitation. Based on this reasoning, an argument can be made to defer mitral valve repair in patients with mild to moderate ischemic mitral 2/9/2016 5 CHEUNG AT regurgitation and viable myocardial segments in whom it is anticipated that surgical revascularization will restore left ventricular geometry and function. Summary Functional or ischemic mitral regurgitation is caused by diseases affecting the left ventricle that causes dysfunction of mitral valve apparatus. The most common pathology is tethering of the mitral valve leaflets as a consequence of dilated cardiomyopathy. While Doppler echocardiography is a standard technique for diagnosis of mitral regurgitation, it may not always accurately grade the severity of functional mitral regurgitation and provide prognostic information because of the dynamic nature of the condition. Echocardiographic evaluation of structural changes such as left ventricular dilation, mitral annular dilation, and mitral leaflet tethering are important for diagnosis and grading the severity of IMR. The benefits of mitral valve repair, mitral valve replacement, or coronary vascularization alone for the treatment of IMR to improve survival, functional status, quality of life, and prevent recurrent IMR remains controversial and is a topic of interest to clinical investigators. REFERENCES 1. Shanewise JS. Cheung AT. Aronson S. Stewart WJ. Weiss RL. Mark JB. Savage RM. Sears-Rogan P. Mathew JP. Quiñones MA. Cahalan MK. Savino J. ASE/SCA guidelines for performing a comprehensive intraoperative multiplane transesophageal echocardiography examination: recommendations of the American Society of Echocardiography Council for Intraoperative Echocardiography and the Society of Cardiovascular Anesthesiologists Task Force for Certification in Perioperative Transesophageal Echocardiography. Journal of the American Society of Echocardiography 1999;12:884-900 2. Zoghbi WA. Chambers JB. Dumesnil JG. Foster E. Gottdiener JS. Grayburn PA. Khandheria BK. Levine RA. Marx GR. Miller FA Jr. Nakatani S. Quiñones MA. Rakowski H. Rodriguez LL. Swaminathan M. Waggoner AD. Weissman NJ. Zabalgoitia M. American Society of Echocardiography's Guidelines and Standards Committee. Task Force on Prosthetic Valves. American College of Cardiology Cardiovascular Imaging Committee. Cardiac Imaging Committee of the American Heart Association. European Association of Echocardiography. European Society of Cardiology. Japanese Society of Echocardiography. Canadian Society of Echocardiography. American College of Cardiology Foundation. American Heart Association. European Association of Echocardiography. European Society of Cardiology. Japanese Society of Echocardiography. Canadian Society of Echocardiography. Recommendations for evaluation of prosthetic valves with echocardiography and doppler ultrasound: a report From the American Society of Echocardiography's Guidelines and Standards Committee and the Task Force on Prosthetic Valves, developed in conjunction with the American College of Cardiology Cardiovascular Imaging Committee, Cardiac Imaging Committee of the American Heart Association, the 2/9/2016 6 CHEUNG AT European Association of Echocardiography, a registered branch of the European Society of Cardiology, the Japanese Society of Echocardiography and the Canadian Society of Echocardiography, endorsed by the American College of Cardiology Foundation, American Heart Association, European Association of Echocardiography, a registered branch of the European Society of Cardiology, the Japanese Society of Echocardiography, and Canadian Society of Echocardiography. Journal of the American Society of Echocardiography 2009; 22:975-1014 3. Zoghbi WA, et al. Recommendation for the evaluation of the severity of native regurgitation with two-dimensional and Doppler Echocardiography. J Am Soc Echocardiogr 2003;16:777-802 4. Shernan, SK. Perioperative Transesophageal echocardiographic evaluation of the native mitral valve. Crit Care Med 2007;35[Suppl.]S372-S383 5. Carpentier A. Cardiac valve surgery: The “French Correction”. J Thorac Cardiovasc Surg 1983; 86:323-37 6. Rao V, et al. Surgical Management of Ischemic Mitral Regurgitation Circulation 2009;120:1287-1293 7. Magne J, Pibarot P, Dagenais F, Hachicha Z, Dumesnil J, Sénéchal M. Preoperative posterior leaflet angle accurately predicts outcome after restrictive mitral valve annuloplasty for ischemic mitral regurgitation. Circulation 2007;115:782-791. 8. Watanabe N, Ogasawara Y, Yamaura Y, Kawamoto T, Akasaka T, Yoshida K. Quantitation of mitral valve tenting in ischemic mitral regurgitation by transthoracic real-time three-dimensional echocardiography. J Am Coll Cardio. 2005;45:763-769. 9. Otsuji Y, Kumanohoso T, Yoshifuku S, Matsukida K, Koriyama C, Kisanuki A, Minagoe S, Levine R, Tei C. Isolated annular dilation does not usually cause important functional mitral regurgitation. J Am Coll Cardiol 2002;39:1651-1656. 10. Kuwahara E, Otsuji Y, Iguro Y, Ueno T, Zhu F, Mizukami N, Kubota K, Nakashiki K, Yuasa T, Yu B, Uemura T, Takasaki K, Miyata M, Hamasaki S, Kisanuki A, Levine R, Sakata Y, Tei C. Mechanism of recurrent/persistent ischemic/functional mitral regurgitation in the chronic phase after surgical annuloplasty. Circulation 2006;114[suppl I]:I-529—I-534. 11. De Varennes B, Chaturvedi R, Sidhu S, Côté A, Li Pi Shan W, Goyer C, Hatzakorizan R, Buithieu J, Sniderman A. Initial results of posterior leaflet extension for severe type IIIb ischemic mitral regurgitation. Circulation 2009;119:2837-2843. 2/9/2016 7 CHEUNG AT 12. Kaplan S, Bashein G, Sheehan F, Legget M, Mut B, Li X-N, Sivarajan M, Bolson E, Zeppa M, Arch M, Martin R. Three-dimensional echocardiographic assessment of annular shape changes in the normal and regurgitant mitral valve. Am Heart J 2000;139:378-387. 13. Kwan J, Shiota T, Agler D, Popvić Z, Xin Qin J, Gillinov M, Stewart W, Cosgrove D, McCarthy P, Thomas J. Geometric difference of the mitral apparatus between ischemic and dilated cardiomyopathy with significant mitral regurgitation: real-time three-dimensional echocardiography study. Circulation 2003:107:1135-1140. 14. Boltwood C, Tei C, Wong M, Shah P. Quantitative echocardiography of the mitral complex in dilated cardiography: the mechanism of functional mitral regurgitation. Circulation 68 No 3;1983:498-508. 15. Yiu S, Enriquez-Sarano M, Tribouilloy C, Seward J, Tajik J. Determinants of the degree of functional mitral regurgitation in patients with systolic left ventricular dysfunction. Circulation 2000;102:1400-1406. 16. Lee A, Acker M, Kubo S, Bolling S, Park S, Bruce C, Oh J. Mechanisms of recurrent functional mitral regurgitation after mitral valve repair in nonischemic dilated cardiomyopathy. Circulation 2009;119:2606-2614. 17. Izumo M, Lancellotti P, Suzuki K, Kou S, Shimozato T, Hayashi A, Akashi Y, Osada N, Omiya K, Nobuoka S, Ohtaki E, Miyake F. Three-dimensional echocardiographic assessments of exercise-induced changes in left ventricular shape and dyssynchrony in patients with dynamic functional mitral regurgitation. Eur J Echocardiogr 2009;10:961-967. 18. Yamano T, Nakatani S, Kanzaki H, Toh N, Amaki M, Tanaka J, Abe H, Hasegawa T, Sawada T, Matsubara H, Kitakaze M. Exercise-induces changes of functional mitral regurgitation in asymptomatic or mildly symptomatic patients with idiopathic dilated cardiomyopathy. Am J Cardiol 2008;102:481-485. 19. Peteiro J, Freire E, Montserrat L, Castro-Beiras A. The effect of exercise on ischemic mitral regurgitation. CHEST 1998;114:1075-1082. 20. Takano H, Adachi H, Ohshima S, Taniguchi K, Kurabayashi M. Functional mitral regurgitation during exercise in patients with heart failure. Circ J 2006;70:15631567. 21. Lebrun F, Lancellotti P, Piérard L. Quantitation of functional mitral regurgitation during bicycle exercise in patients with heart failure. J Am Coll Cardiol 2001;38:1685-1692. 2/9/2016 8 CHEUNG AT 22. Badiwala M, Verma S, Rao V. Surgical management of ischemic mitral regurgitation. Circulation 2009;120:1287-1293. 23. Levine R, Schwammenthal E. Ischemic mitral regurgitation on the threshold of a solution: from paradoxes to unifying concepts. Circulation 2005;112:745-758. 24. Gorman III J, Ryan L, Gorman R. Pathophysiology of ischemic mitral insufficiency: does repair make a difference? Heart Fail Rev 2006;11:219-229. 25. Gillam L. Is it time to update the definition of functional mitral regurgitation? Structural changes in the mitral leaflets with left ventricular dysfunction. Circulation 2008;118:797-799. 26. Enriquez-Sarano M, Loulmet D, Burkhoff D. The conundrum of functional mitral regurgitation in chronic heart failure. J Am Coll Cardiol 2008;51 No 4:487-489. 27. Penicka M, Linkova H, Lang O, Fojt R, Kocka V, Vanderheyden M, Bartunek J. Predictors of improvement of unrepaired moderate ischemic mitral regurgitation in patients undergoing elective isolated coronary artery bypass graft surgery. Circulation 2009;120:1474-1481. 28. Salgo IS. Gorman JH 3rd. Gorman RC. Jackson BM. Bowen FW. Plappert T. St John Sutton MG. Edmunds LH Jr. Effect of annular shape on leaflet curvature in reducing mitral leaflet stress. Circulation 2002;106:711-7. 29. Bonow RO. Carabello BA. Chatterjee K. de Leon AC Jr. Faxon DP. Freed MD. Gaasch WH. Lytle BW. Nishimura RA. O'Gara PT. O'Rourke RA. Otto CM. Shah PM. Shanewise JS. 2006 Writing Committee Members. American College of Cardiology/American Heart Association Task Force. 2008 Focused update incorporated into the ACC/AHA 2006 guidelines for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 1998 Guidelines for the Management of Patients With Valvular Heart Disease): endorsed by the Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. Circulation 2008;118:e523-661. 30. Vahanian A. Baumgartner H. Bax J. Butchart E. Dion R. Filippatos G. Flachskampf F. Hall R. Iung B. Kasprzak J. Nataf P. Tornos P. Torracca L. Wenink A. Task Force on the Management of Valvular Hearth Disease of the European Society of Cardiology. ESC Committee for Practice Guidelines. Guidelines on the management of valvular heart disease: The Task Force on the Management of Valvular Heart Disease of the European Society of Cardiology. Eur Heart J 2007;28:230-68. 2/9/2016 9 CHEUNG AT 31. Chan KMJ, Punjabi PP, Flather M, et al. Coronary artery bypass surgery with or without mitral valve annuloplasty in moderate functional ischemic mitral regurgitation. Final results of the Randomized Ischemic Mitral Evaluation (RIME) Trial. Circulation 2012;126:2502-10. 32. O’Gara P. Randomized trials in moderate ischemic mitral regurgitation. Many questions, limited answers. Circulation 2012;126:2452-5. 33. Acker MA, Parides MK, Perrault LP, et al. Mitral-valve repair versus replacement for severe ischemic mitral regurgitation. New Engl J Med 2014; 370:23-32.