Peri- implant disease
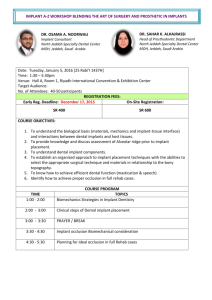
advertisement

Implant Maintenance Morag Powell Dip Dh Dip DT RCS (Edin) Learning objectives Upon completion of reading this article, the dental professional should be able to: Describe the differences between peri-implant mucositis and periimplantitis Describe how to effectively screen dental implants for peri-implant diseases Have a knowledge of oral hygiene aids that are available to use for the prevention of inflammation around implants. Peri- implant disease As dental implants become more commonplace within every day practice, the rise of dental implants with inflammation present around them is very evident. Peri-implant disease is a collective term for inflammatory processes that occur around tissues that surround the implant.1 This inflammation around dental implants can be placed into two categories: peri-implant mucositis and periimplantitis. The term peri-implant mucositis is used to describe reversible inflammation of the soft tissues surrounding implants. Peri-implantitis is the term used to describe an inflammatory condition that involves both the soft tissues and the surrounding bone of the implant.2 Implants can fail very early on after placement as a result of the implant failing to integrate with the bone. These types of failures are known as early implant losses. Implants can also fail during function – this is when an implant has been placed, restored and has been used in function in the patient’s mouth for a length of time. Implants that fail during function can be the result of biologic processes characterized by clinical signs (eg, implant mobility) that emerge only when an advanced and possibly irreversible state of the disease has been reached.2 It is therefore of vital importance that implants are monitored for signs of disease as routine when presenting in the hygienists/dentists surgery. The hygienist’s role with implants Baseline recording When an implant is placed it is good practice for the dentist placing the implant to take a baseline radiograph to record the bone level of the implant on placement. This gives the team involved in caring for the implant a baseline to work from for future assessment. After the fit of the implant restoration, time should be allowed time for any localized inflammation to subside. Once this has occurred, an appointment with the hygienist or dentist should be scheduled to record base line parameters – probing depths, bleeding on probing and plaque score. A modified version of the original Sillness and Loe Plaque index has been produced by Mombelli et al, along with a modified version of the Gingival Index (GI) and a simplified version of the GI by Apse et al to help with the recording of these indices. It is important to remember when recording a GI modified index that soft tissue texture and colour around implants can depend on the normal appearance of the tissue prior to placement, and that non keratinized tissue can appear to be redder in colour than keratinized tissue. There have only been weak correlations between GI scores and changes in peri-implant crestal bone levels, in contrast to studies suggesting that an absence of BOP around implants is a predictor of peri-implant health, and that BOP alone around implants yielded higher diagnostic accuracy for peri-implant diseases at implant sites compared with tooth sites.3 Table 1 Plaque Index – Mombelli et al Score 0 1 No detection of plaque Plaque only recognized by running a probe across the smooth marginal surface of the implant 2 3 Plaque can be seen by the naked eye Abundance of soft matter Table 2 Gingival Index – Mombelli et al Score 0 1 No bleeding when a periodontal probe is passed along the mucosal margin adjacent to the implant Isolated bleeding spots visible 2 3 Blood forms a confluent red line on the mucosal margin Heavy or profuse bleeding Table 3 Gingival Index – Apse et al Score 0 1 2 3 Normal mucosa Minimal inflammation with colour change and minor edema Moderate inflammation with redness, edema and glazing Severe inflammation with redness, edema, ulceration and spontaneous bleeding without probing Which ever index that we choose to use is not the concern, it is the regular recording of clinical observations that is of importance. A suggested guide is to record BOP around the implants at every visit and record ppd annually unless there are signs of inflammation. If inflammation is present then the ppd must be monitored more frequently until either inflammation has resolved or the patient has been referred on. Individual Homecare plans An individual homecare plan should be developed at the initial appointment after restoration fit with the hygienist/dentist. This allows the patient to know exactly how they need to care for the implant. Teaching the patient how to maintain the health of their implant is part of the duty of care that is expected from a dentist placing implants. If the dentist does not wish to do this, this task must be delegated to a member of his/her team as it is of vital importance in the prevention of peri-implant diseases. As clinicians we cannot assume that a patient will know how they must care for their new implant. There is a variety of oral hygiene aids available for use for homecare of the implant. In addition to brushing, the most popular aid for cleaning is the power tip attachment for the braun toothbrush or a manual version of this (interspace brush). This brush allows delicate cleaning and removal of biofilm from the implant sulcus. These brushes can be modified by removing bristles with scissors, making them thinner and more easily adapted to the implant sulcus. Superfloss and Implant floss are both very good at removing the biofilm by cleaning the neck of the implant due to the thickness and absorbing nature of the floss. Interdental brushes and regular floss can also be used, but in my experience interdental brushes alone will not control the biofilm, especially around the buccal and lingual aspects of the implant so they need to be used in conjunction with superfloss/floss. The air flosser by Phillips Sonicare and the water irrigators available are also very good and most importantly, very easy for patients to comply with. Instruments to remove Biofilm around implants There are many different types of instruments available on the market for cleaning around dental implants. When considering your selection of instrument to use around a dental implant you must take into consideration the effect that the instrument will have on the surface of the implant. Due to this, standard dental instruments are not recommended for this procedure. Plastic instruments have been available for many years now but have the disadvantage that they cannot be sharpened and are very bulky in nature. Carbon instruments are also available, which are thinner than the plastic instruments but again are not easy to maintain. The hand instrument of choice to remove the biofilm from the implant is a titanium instrument. These are widely available from the main manufacturers of dental instruments including Deppeler, PDT and LM. The titanium instrument has been shown to cause very little damage to the implant surface and can be sharpened with a sharpening stone. It is however, important that the sharpening stone that is used for this is kept solely for sharpening titanium instruments. Ultrasonic tips are available with plastic inserts to use around the implant and there are also ceramic tips now available for use with some of the piezo machines. Iatrogenic factors in Peri-implant disease When a patient presents with peri-implant diseases we must look to see if there are any other factors that may be influencing the condition. These include: Excess cement around the implant Abutments not fitting correctly Design of restorations Site of implant placement Excess cement can be checked for by using some floss around the implant or by using an explorer probe. If there is excess cement, it can be removed easily with a hand instrument and the health of the gingivae should improve. Abutments not fitting correctly can be checked on radiographs by the dentist placing them and altered if necessary. The dentist placing the implants should also take into account the design of the restoration in relation to allowing the patient enough access to the implant so it can be cleaned on a daily basis with all of the above mentioned oral hygiene aids. Adjunctive treatments When peri-implant diseases are detected, adjunctive aids can be considered for use along side instrumentation. These include: Amino acid glycine powder Atridox Dentomycin Perio-chip The amino acid glycine powder used in place of the sodium bicarbonate in the air polishing systems has been shown not to change surface characteristics of titanium implants4 with favourable treatment outcomes similar to that of subgingival root surface debridement with hand instruments.5 The EMS perio flow system comes with a disposable plastic nozzle, which can be bent to give better access to pockets around difficult to reach implants. Antibiotics also can be administered locally to areas of inflammation, Dentomycin is the most popular that is used in practice. The antibiotics are most effective when they are administered in conjunction with biofilm disruption in the implant pocket. Chlorehexidine has been shown to significantly reduce the bacterial load on the surface of implants, and the placement of a perio-chip is relative easy around the implant. It is always important to remember to inform patients that there may be an initial localised swelling that lasts for 48 hours when a perio chip is placed and that they need to avoid flossing for 10 days after placement as per manufacturers instructions. Before using any of the above in the treatment of peri-implant diseases the hygienist should discuss each case with the referring dentist to determine a treatment plan and gain a prescription (if required). Summary Peri-implant diseases are increasing in prevalence within daily practice and need to be screened for when treating patients who have dental implants. Instruction in how to care for dental implants needs to be given to patients immediately after the implant has been restored and becomes functional. By delivering this instruction when the implant becomes functional, disease processes can be prevented. References: 1. Mombelli A, Lang NP. The diagnosis and treatment of peri-implantitis. Periodontal 2000 1998:17:63-76 2. Salvi, Lang. Diagnostic parameters for monitoring peri-implant conditions. Int J Oral Maxiofac Implants 2004; 19 (suppl) 116-127 3. Jepsen S et al. Progressive peri-implantitis. Incidence and prediction of periimplant attachment loss. Clin Oral Imp Res 1996; 7: 133-134 4. Schwarz, F., Ferrari, D., Popovski, K., Hartig, B. & Becker, J. J. (2009) Influence of different air-abrasive powders on cell viability at biologically contaminated titanium dental implants surfaces. Journal of Biomedical Materials Research. Part B, Applied Biomaterials 88, 83–91. 5. Moëne, R., Décaillet, F., Andersen, E. & Mombelli, A. (2010) Subgingival plaque removal using a new air-polishing device. Journal of Periodontology 81, 79–88.