Ketamine - Angelique I Davis The University of Kansas
advertisement
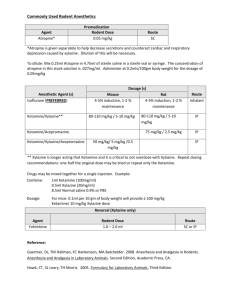
Running head: KETAMINE 1 Ketamine Angelique Davis Kansas University Medical Center KETAMINE 2 Ketamine What is special K? No, not the special K Kellogg’s cereal challenge, but moreover the commonly known street drug “Special K” or clinically known as Ketamine or Ketalar. Although ketamine has been known to be an addictive drug, there is a substantial clinical use for ketamine in anesthesia. Ketamine is a fairly new drug compared to other anesthetics and narcotics, as it was discovered in the 1970s. The extensive background of ketamine has had researchers searching for answers on how ketamine affects our bodies, what our bodies do with the drug, and the proper anesthetic uses of ketamine. Phencyclidine derived drugs were first discovered in the 1950s by Parke-Davis industries in an attempt to develop a drug that had both analgesic and anesthetic properties. Parke-Davis industries first looked at PCP, but it was discontinued in 1978 due to its abusive nature and severe psychodysleptic effects. Thus after additional research ketamine, a cyclohexamine, was developed in the 1970s having little to no effect on respiratory and cardiovascular systems, although it still has some psychodysleptic effects (Georges & Thierry, 2013). Ketamine is classified as a noncompetitive N-methyl-D-aspartate (NMDA) antagonist, inhibiting glutamate. NMDA receptors are ligand-gated ion channels that allow influx of calicum and sodium anions which deploraize the cell and cause an action potential (Nagelhout & Plaus, 2013). Ketamine is primarly an anesthetic, but has an analgesic effect as well due to its mechanism of action. According to (Nagelhout & Plaus, 2013), the mechanism of action for ketamine is “coined as dissociative anesthesia” by working on several different areas of the central nervous system (p. 113). Ketamine’s mechanism of action is very extensive as defined by (Butterworth IV, Mackey, & Wasnick, 2013): KETAMINE 3 Ketamine inhibits polysynaptic reflexes in the spinal cord as well as excitatory neurotransmitter effects in selected areas of the brain. In contrast to the depression of the recticular activating system induced by the barbiturates, ketamine functionally “dissociates” the thalamus (which relays sensory impulses from the reticular activating system to the cerebral cortex) from the limbic cortex (which is involved with the awareness of sensation) (p. 182). Ketmine then allows a patient to look aware, but not respond to stimuli normally. Patient’s receiving ketamine seem “awake” by having their eyes open, being able to maintain swallowing function, pupillary reaction, and an intact respiratory drive, depending on the dose given (Butterworth IV et al., 2013). There are multiple routes that ketamine can be administered and or absorbed, making it very adaptable to clinical situations. Ketamine can be delivered intravenously (IV), intraosseous, intramuscular, orally, nasally, and rectally. Doses of ketamine may vary depending on various factors concerning the patient and whether induction or sedation is needed. A typical dose and route for an adult is intravenously 1-2 mg/kg for induction and 2.5-15 mcg/kg/min IV for sedation (Butterworth IV et al., 2013). The distribution of ketamine can be further explained by delving into pharmacokinetics. Ketamine and pharmacokinetics is best defined by a two compartment model pertaining to distribution. Ketamine is a potent anesthetic by reasoning of being protein bound by only 12% and being highly lipid soluable (Nagelhout & Plaus, 2013). Ketamine baring these two chacteristics allow quick upake to the brain, causing an increase in cerebral blood flow and cardiac output (Butterworth IV et al., 2013). IV Ketamine is directly absorbed into the central compartment, crossing the blood brain barrier, then redistributed to the peripheral compartment. KETAMINE 4 After ketamine reaches the periphery, it is then metabolized by the hepatic system and excreted in the urine. Metabloism in the liver produces several metabolites, but the most discussed active metabolite is norketamine, by the P-450 system. The active metabolite norketamine has a reduced potency of about 20-30% that of ketamine. Norketamine is then metabolized into inactive water soluble metabolites that are excreted in the urine (Nagelhout & Plaus, 2013). The above stated pharmacokinetics lead into ketamine’s pharmacodynamics. Since ketamine acts on the central nervous system (CNS), primarly in the thalmic and limbic system, it induces a “dissociative anesthesia”. Ketamine is effective in different ways at different plasma concentrations. According to (Nagelhout & Plaus, 2013), “Anesthetic levels are present with plasma levels of 640 to 1000 mcg/ml, and analgesic levels are present with plasama ketamine concentrations of 100 to 150 mcg/ml” (p. 114). Ketamine acts on different parts of the body, in different ways. Ketamine’s effects on the cardiovascular system are increased blood pressure, increased heart rate, and increased systmetic vascular resistance, thus resulting in increased cardiac output. The response on the respiratory system is similar to that of the sympathetic nervous system as well, by brochdilating and only slightly reducing the repiratory rate upon first dose administration. Since ketamine increases cardiac output it will then increase cerebral blood flow causing an increase in intracranial pressure. Ketamine also increases salvation and lacrimation, which can be mediated with an anticholinergic if necessary. Once ketamine is administerd the desired effects are unclear to providers due to dissociative anesthesia, but according to (Nagelhout & Plaus, 2013) “clinical anesthesia can be obtained 3 to 5 minutes” (p. 113) after administration. After an initial dose of ketamine a patient will start to re-orient at appoximately 15 minutes. If a paient recieves repeated doses, reawakening can certainly take longer. Elimination half-life of ketmine is 2-3 hours and again can be longer if KETAMINE 5 repeated doses are given (Nagelhout & Plaus, 2013). Ketamine has a wide therapuetic index. Overdose of ketamine is unlikely in the clinical setting, but some signs and symptoms are reduced ability to maintain airway, seizures, hypertension, vomiting, anxiety and chest pain (Lakey, 2011). In this day and age anesthesia providers are aware of a patients status due to vigilant monitoring of the patient. Ketamine has a use in multiple clinical situations, but also some contraindications as well. Ketamine is particularly useful over other IV anesthetic agents due to its stability of the sympathetic nervous system. Ketamine is useful in hemodynamically unstable patients (i.e. trauma, burns, hypovolemia, and shock), asthmatics, and outpatient or bedside procedures. Since ketamine has sympathomimetic properties, ketamine increases heart rate, cardiac output, cerebral blood flow, mean arterial pressure, and intracranial pressure (ICP). These properties will successfully provide analgesia and sedation to patient with a reduced reserve. Controversially, ketamine can have the reverse effects on a patient that has depleted their sympathetic reserve in accordance with their primary injury. The adverse effects of ketamine are increased salvation, lacrimation, increased ocular pressure, and in some patients the increased cerebral blood flow can cause increased ICP levels. The literature involving elevated cerebral blood flow is vague on whether there is truly a negative affect associated with the increased ICP. The increased ICP may be of benefit to the surrounding tissues of the initial injury in due part by increasing cerebral perfusion pressures. Ketamine would not be used on patients with glaucoma or patients undergoing eye surgery due to increased intraocular pressure and nystagmus. Ketamine also can cause emergence phenomena. Emergence phenomena cause vivid dreams, floating sensations, and delirium, which deter providers from using ketamine (Nagelhout & Plaus, 2013). A literature review performed a study on patients and adverse effects, but focused more on KETAMINE 6 emergence phenomena with administration of ketamine only and administration of ketamine and midazolam. A literature review pertaining to the administration of ketamine alone and ketamine with midazolam set out to discover if emergence phenomena would improve with co-administration of both ketamine and midazolam. The study “was a prospective, cross sectional, comparative, observational study, conducted at a tertiary hospital, by the department of pharmacology in collaboration with the department of anesthesia.” (Lohit, Srinivas, & Chanda, 2011, p. 321). The article performed a study on a group of 60 patients, 30 patients received just ketamine and the other 30 patients received ketamine and midazolam. The patients were carefully screened for four hours post procedure for subjective signs and symptoms of emergence phenomena. The study showed patients receiving both medications had a “smooth and complete post-surgical recovery” (Lohit et al., 2011, p. 322), as compared to the patients that only received ketamine. The study on ketamine-induced emergence phenomena is only the tip of the iceberg and needs additional research, but this article is a step in the right direction. Ketamine is not only an IV anesthetic, but also an analgesic. Ketamine is unlike any other IV anesthetic in this way. Ketamine has a unique characteristic by keeping patients both hemodynamically stable and providing worthy sedation and analgesia. Since ketamine used alone increases chances of patients having emergence phenomena, exploring options to reduce this adverse effect is imperative. I see ketamine still being used in the next 10-20 years due to the positive benefits it has for multiple settings, i.e. pre-hospital, procedural, disaster, emergency, and general anesthesia. KETAMINE 7 References Butterworth IV, J. F., Mackey, D. C., & Wasnick, J. D. (2013). Intravenous anesthetics. In B. Belval, & H. Lebowitz (Eds.), Morgan & Mikhail’s clinical anesthesiology (5th ed. (pp. 182-184). New York, NY: McGraw-Hill. Georges, M., & Thierry, V. (2013, February 23). Ketamine pharmacology: An update (Pharmacodynamics and molecular aspects, recent findings). CNS Neuroscience & Therapeutics, 19, 370-380. Lakey, S. (2011). Ketamine overdose. Retrieved from http://pain.emedtv.com/ketamine/ketamine-overdose.html Lohit, K., Srinivas, V., & Chanda, K. S. (2011). A clinical evaluation of the effects of administration of midazolam on ketamine-induced emergence phenomenon. Journal of Clinical and Diagnostic Research, 5, 320-323. http://dx.doi.org/JCDR/2011/1244 Nagelhout, J. J., & Plaus, K. L. (2013). Intravenous induction agents. In J. J. Nagelhout, & K. L. Plaus (Eds.), Nurse anesthesia (5th ed., pp. 113-117). St. Louis, MO: Elsevier Saunders.