Poisoning and first aid
advertisement

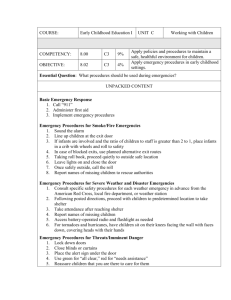
Animal nursing: First aid Objectives List the 3 aims and rules of first aid Classify injuries as life threatening, serious, or minor and describe what that means in terms of owner response List the 8 basic questions that should be asked of an owner over the phone in a first aid emergency to elicit the information required to respond appropriately Describe 5 important points you will cover in your description of the way an owner should approach handle and transport a conscious animal with a painful immobilising injury Describe the preliminary assessment of the first aid patient and the protocol for basic CPR should it be required Discuss the assessment and treatment of a variety of specific first aid conditions References Goodwin, J. (2003) First aid. In B.Cooper & D.L. Lane (Eds.) Veterinary Nursing (3rd ed.) (pp. 101-141). Edinburgh: Butterworth - Heinemann Tasks 1. Make up a role play to demonstrate the appropriate response to an owner ringing up the clinic in a panic because their animal has had a first aid emergency. 2. Describe 5 important points you will cover in your description of the way an owner should approach handle and transport a conscious animal with a painful immobilising injury. 3. Use Humphrey to ventilate your patient at an appropriate rate depth and rhythm for a larger dog and a cat (expiratory pause!) and ensure correct placement of pressure for cardiac massage 4. The vet is busy suturing up the uterine stump in a bitch spey. You are on reception duty and there is another vet nurse in the pharmacy organising some medication. An owner brings Humphrey through the door and he is limp and unresponsive in the owners arms, the owner says he was still breathing as he picked him up out of the car to bring him in but breathing has now ceased and you can’t detect a femoral pulse. Role play your response to this situation and use Humphrey in pairs for 2 person resuscitation in this CPR emergency. Don’t forget the 4 rules of CPR. FIRST AID Definition The immediate treatment of injured animals or those suffering from sudden illness. Three aims of first aid are: a) To preserve life b) To prevent suffering c) To prevent the situation from deteriorating. Legal Limitations Lay Persons - Anyone over the age of 18 is permitted to amputate the dew claws of a puppy before its eyes are open; and anyone is allowed to render first aid in an emergency for the purpose of saving life or relieving pain or suffering. Special provisions for veterinary nurses in New Zealand don’t exist as they do overseas, so only a veterinarian may perform surgery. Veterinary nurses and lay persons are legally unable to do a wide range of even quite minor invasive procedures and treatments. And with the legal “duty of care” and “negligence” laws they have to be accountable to, veterinarians in this country are usually quite conservative about what they will use veterinary nurses to do. However despite those issues, in a first aid situation a veterinary nurse would be expected to be able to act quickly and appropriately especially in the absence of a veterinarian. A qualified veterinary nurse might well be expected to respond using advanced first aid equipment and techniques and manage the patient and its stabilisation for a longer period independently. Veterinarians who are prepared to allow their nurses to routinely and independently use their professional skills and abilities may also use “VOIs” to detail expected actions and limitations of a nurses responsibilities in specific situations. This ensures veterinary nurses are legally covered to do such things as administer Temgesic or Morphine as pain relief for fracture patient being stabilised. In New Zealand we are trying to set up a system similar to many overseas. In Britain any medical treatment or minor surgery (not involving entry into a body cavity) to a companion animal may be done by a veterinary nurse if the following conditions are complied with: 1. the companion animal is, for the time being, under the care of a registered veterinary surgeon or veterinary practitioner and the medical treatment or minor surgery is carried out by the veterinary nurse at their direction; and 2. the registered veterinary surgeon or veterinary practitioner is the employer or is acting on behalf of the employer of the veterinary nurse. 3. Does not apply to veterinary nurses in training. They have the rights of a lay person and may also carry out nursing duties and assist veterinary surgeons in any way which does not involve an act of veterinary surgery. Removal of sutures, replacement of dressings, cutting of nails and beaks, and the sealing of teeth are procedures that are NOT acts if veterinary surgery. Role of a Veterinary Nurse in an Emergency Situation 1. To establish the nature and severity of the emergency by obtaining a good history. 2. Give immediate and relevant instructions and advise to the owner/caretaker. 3. Make the necessary preparations for arrival of the patient. 4. Administer first aid treatment to an animal by whatever means are available, but only as an interim measure, designed to preserve life and alleviate suffering until the veterinarian is available to attend the animal. The Four Rules of First Aid Are: 1. 2. 3. 4. 5. 6. Stay calm Be prepared Do not put yourself, owners or other staff at risk Ensure the animal is at no further risk Assess the severity of the illness/injury (triage the situation) Contact the veterinarian as soon at possible Telephone Calls Often the nurse on reception is the first point of contact for a client. It is the nurse’s job to elicit information from the client to ascertain the severity of the problem, and offer appropriate advice without making a diagnosis or offering a prognosis Classification of emergencies: EXAMPLE OF TYPES OF EMERGENCIES Life Threatening requires immediate action Unconsciousness Collapse Dyspnoea or cyanosis Anuria Severe haemorrhage Severe burns Prolapsed eye Poisoning Dystocia Open fractures Minor Insect stings Minor wounds (where the haemorrhage is easily controlled by bandaging) Minor burns (where there is only slight discomfort) Abscesses Slight lameness (where animal is able to bear some weight on the leg) Haematuria Aural haematomata 1. Life-threatening emergencies: involve significant disturbance of major body systems and have the potential for rapid deterioration and death, requiring urgent life-saving help. 2. Minor emergencies: Emergencies where life is not immediately threatened, where full evaluation and treatment can be delayed until after the needs of life-threatening emergencies have been dealt with. Restraint and Transport of the Injured Animal With all injured animals, before help can be provided it is necessary for them to be adequately restrained. The approach to and restraint of the injured animal is a vital preliminary, although animals that have suffered the most damage are usually the least likely to offer any resistance. Your approach to an injured animal should be calm, quiet and yet purposeful. It is often valuable to have the assistance of two or three sensible people. By talking to the animal in a quiet, reassuring voice you may be able to get close enough to restrain it, at least temporarily. If all attempts at catching the animal fail, it may be necessary to get professional assistance, e.g. the vet clinic may do house calls. Restraint may require drugs or specialist equipment. Cats Be careful scruffing dyspnoeic animals, or those showing signs of spinal injury. Boxes or cages can be placed on top of collapsed or fractious animals, and a cardboard sheet slid underneath so the cat comes to lie on it. Dogs Muzzles may be indicated, but should not be used in dyspnoeic or vomiting animals. Allow the animal to assume the most comfortable position for transport. Stretchers may be indicated for animals with spinal injuries. These are simply supporting surfaces: wood sheets, coats supported by poles, or even a blanket. Birds Handle very gently Do not compress the thorax or abdomen Gloves may be required for psittacines Horses Use of halters, twitches, lifting leg etc. Arrival at the Surgery: (Preliminary Assessment of Degree of Injury) Preliminary assessment and triage 1. Safety On arrival the animal should be examined (with due care for the safety of the professional staff the client and the animal), a provisional assessment made and treatment given. If more than one animal arrives at once, the most life threatening emergencies should be dealt with first. 2. Response The next step is to assess the level of consciousness of the animal. If a problem exists it is vital to determine whether an animal is unconscious or dead. COMPARISON BETWEEN RECENT DEATH AND UNCONSCIOUSNESS Sign Death Unconscious collapse Heart beat Absent for more than 3 minutes Regular, though slowed Respiratory pattern Absent, although occasionally Cheyne Stokes respiration is observed Varies according to the depth of CNS depression (mimics anaesthesia) Eyeball position Central Turned down or central, according to the depth of CNS depression Cornea Glazed Normally moist Corneal reflex Absent Present (unless eyelids paralysed) Pupil size Fully dilated May vary in size, but are rarely fully dilated Pupillary light reflex Absent Usually present unless iris paralysed Movement Absent, except Cheyne Strokes respiration May be roused in stupor Body temperature Rigour mortis in a few hours Cools within 15 minutes Remains constant Depth of Unconsciousness. This is assessed by the various eye reflexes. The pedal reflexes are also a useful indication as to the depth of unconsciousness, since they are the first reflexes to be lost as brain activity becomes depressed and the last to return as the condition improves. There are two terms used to describe the depth of unconsciousness: Stupor, the animal can be roused with difficulty and the pedal withdrawal reflex is still present, though the toes may need to be pinched quite hard. Pupillary and palpebral reflexes are also still present. Coma, the animal cannot be roused, the pedal reflexes are absent and the eye reflexes indicate a plane of surgical anaesthesia or deeper. The pupils become dilated as the condition deteriorates and death approaches. Other clinical signs may be seen in animals with an altered state of consciousness Convulsions. Convulsions are violent, irregular, involuntary movements of the body. The time of onset and duration should be noted. Incontinence. Urine or faeces may be passed by the unconscious animal either passively (a gradual seepage because the sphincter muscles relax) or actively (e.g. a pool of urine passed during an epileptiform fit). Collapse Collapse is said to have occurred when a conscious animal is unable or unwilling to stand up. ‘Collapse’ is the most common emergency reported by owners and covers a multitude of situations from an arthritic dog which is reluctant to get up and go for a walk to a deceased pet. The cause and severity of the ‘collapse’ must therefore first be discovered so that the correct first aid procedures may be carried out. Unconscious animals should always take priority and must be examined and treated immediately. 3. ABCs The current protocol for unresponsive animals is: Check ABC then apply CAB Airway Control Ensuring a clear airway: Lay the animal in right lateral recumbency. Position against a hard surface to improve stability and head in a slightly head-down position. Barrel chested dogs or those weighing greater than 20 Kg should be positioned in dorsal recumbency and stabilised to prevent rolling (e.g. with sand bags). Open the jaws, pull the tongue forward and examine the airway with a light. Where possible remove any foreign bodies, e.g. balls, bones, broken teeth with your fingers or device (e.g. allis tissue forceps). Wipe away any vomit, mucous or blood from the back of the throat. Position the head lower than the chest to facilitate drainage of fluid from the respiratory tract and reduce the risk of aspiration of regurgitated or vomited gastric contents. Breathing If breathing appears to have stopped completely and yet the animal is not yet in cardiac arrest, as determined by checking for its heartbeat, etc., artificial respiration is essential. Intubate the animal with a cuffed endotrachael tube. If under anaesthetic, turn OFF the anaesthetic. Flush the bag with 100% oxygen. Begin intermitant positive pressure ventilation (IPPV)with 100% oxygen. If this is not possible, then IPPV can also be provided by breathing expired air into the animal’s lungs via the endotracheal tube or by the use of a self inflating resuscitation bag (e.g. ambu resuscitator) connected to the endotracheal tube. Until equipment is available first responders should apply mouth to nose ventilation. Circulation If breathing has stopped, then check for a palpable heart beat pulse and by feeling between the 4th -6th ribs for a heart beat and feeling the medial side of the thigh for a femoral pulse. If a palpable femoral pulse is absent then the cardiac function is insufficient for vital cell function and CPR should start. For an unresponsive patient that is not breathing and has no heartbeat the checks should take no more than 15 seconds. Compressions are the most vital action for effective preservation of life so if breathing and circulation have ceased CPR must start with compressions. In cats and small dogs the cardiac pump mechanism which directly compresses the heart, should be used. For medium and large size dogs the thoracic pump mechanism compresses the thoracic cavity and thus increased intra- thoracic pressure squeezes the heart. Compressions are applied at the same rate for all animals ie approximately 100 beats per minute. If there are 2 people available, giving 1 breath per 6 seconds gives an appropriate respiration rate of 10 breaths per minute. Alternatively for single handed resuscitation attempts, deliver 2 lung inflations for every 30 chest wall compressions. The effectiveness of chest compressions can be increased if a second operator inflates the chest simultaneously with a compression. If the cause of the cardiopulmonary arrest is known to be a choking incident, after each round of compressions and before ventilating the patient the operator should check the airway to see whether the blockage has been dislodged by the CPR. If it hasn’t attempt ventilations anyway since they may help move the blockage down into one lung which allows the patient to breath sufficiently for life with the other unobstructed lung until further action can be taken. Detection of a femoral pulse or monitoring retinal blood flow with a Doppler probe by a second operator can assess the efficiency of the compressions. Research shows the first few compressions are only sufficient to raise blood pressure and more are required to actually move blood through the vessels. This is the key reason for recent changes in the protocols and the reason a single person operator should continue with compressions and breaths uninterrupted for 2 minutes before checking for signs of life. Signs of effective CPR: Early: Palpation of pulse during compression Constriction of pupil Ventromedial location of the eye Improvement of mucous membrane colour ECG changes Late: Lacrimation Cranial nerve reflexes return (e.g. blinking, gagging, coughing) Return of spontaneous respiratory activity. If early signs are not seen within two minutes, two alternative options remain: Drugs and External defibrillation: Emergency thoracotomy and internal cardiac compression Nurses can prepare for either eventuality by ensuring that the crash cart with resuscitation drugs is fully stocked and that resuscitation drugs have not expired. You must know the drugs and equipment required during CPR and be able to reconstitute them. The secondary survey and stabilisation If animal is conscious, perform a quick physical examination noting: any obvious abnormalities in body conformation evidence of external haemorrhage skin colour and mucous membranes rate and quality of pulse and respiration temperature unusual odours Shock- Treatment and recognition Definition: Shock is a multisystemic response to a disease process that results in inadequate tissue perfusion. This results in insufficient oxygen delivery to meet the tissues needs. The inadequacy of perfusion can be secondary to a number of circulatory problems that are classified into 4 different forms of shock Types of shock Hypovolaemic: due to decreased circulating blood volume eg haemorrhage or secondary to dehydration Distributive (anaphalactic, toxic): due to vasodilation of blood vessels and abnormal distribution of body fluid eg sepsis and allergic reaction Cardiogenic: due to failure of the heart to pump eg dilated cardiomyopathy or severe arrhythmia Obstructive: due to blockage of blood flow in the vessel eg pericardial effusion or pulmonary thromboembolism Clinical Signs Tachycardia, weak and thready pulse quality, vasoconstriction (pale colour, prolonged CRT, cold appendages, oliguria), low blood pressure. Treatment for shock Since treatment of the different types of shock may be quite different diagnosis of the cause is quite essential. But in general oxygen supplementation, and a warm stress free environment are helpful. Fluid therapy is a key therapy for hypovolaemic shock and may be helpful for distributive shock but usually contraindicated for cardiogenic shock Specific first aid conditions and their treatment 1. Haemorrhage Classification of haemorrhage: (a) By Type of Blood Vessel Damaged Arterial haemorrhage Most serious type of haemorrhage and most difficult to stop. Arterial bleeding is bright read and spurts in pulses from a wound. A definite bleeding point can be detected. Venous Haemorrhage slightly less serious than arterial haemorrhage but rapid blood loss will occur if a large vein is damaged. Easier to control than arterial haemorrhage because of low pressure Venous blood is darker red and streams steadily from a wound. A definite bleeding point is visible. Capillary Haemorrhage Occurs in all wounds Blood escapes from multiple, pinpoint sources in the tissues and oozes from the wound with very little force. No definite bleeding points are visible. (b).Destination of blood loss External Haemorrhage bleeding that is clearly visible at the body surface. Internal Haemorrhage bleeding into tissues or body cavities. Hidden. In most cases the only way to detect severe internal bleeding is by recognising the general signs of shock which the haemorrhage produces. First Aid Treatment of Haemorrhage direct digital pressure, wear gloves and apply for at least 5 minutes use of artery forceps and ligation of vessel pad and pressure bandage, if blood seeps through do not remove , apply another bandage over the first. Monitor the circulation distal to the bandage eg nail bed, should remain pink and toes should not swell. Pressure bandaging of the abdomen for internal bleeding should only be left in place for a maximum of 12 hours 2. Wounds Definition: A wound is an injury in which there is a forcible break in the continuity of the soft tissues. CLASSIFICATION OF WOUNDS Open Closed Incised Contusion Lacerated Haematoma Puncture Haemorrhage into body cavity Abrasion Open wounds Involve an injury that breaks the body surface (skin or mucous membrane). These wounds are externally visible and blood loss can be evaluated. There are four types of open wounds: Incised Caused by sharp, cutting instruments e.g. scalpel, knives, glass, cat claws. Edges are. clean cut and clearly defined, usually gape, especially with movement. Avulsed, incised wounds are often V-shaped. Usually bleed freely. Often penetrate deeply to damage underlying structures, e.g. tendons, nerves. Laceration Wounds are irregular in shape, with jagged and uneven edges. Areas of skin may be literally be worn away. Edges of the wound always gape because the skin has been torn apart. Severity depends on the depth of the wound. Often little haemorrhage. Wounds are contaminated and dirty thus increasing the risk of infection. Healing is slow. Puncture Wounds Wounds produced by penetration of sharp pointed objects e.g. teeth, claws, stakes, nails, thorns, bullets. The actual skin would may be quite small but this will often lead to a long narrow track which penetrates deeply into the underlying tissues. Little haemorrhage, close quickly, but are often contaminated. Rapid healing if adequate drainage is provided and infection is controlled. Abrasions Are the same as a graze wound. Such wounds do not penetrate the entire skin thickness. Are superficial, often contaminated and rarely serious. First Aid of Open Wounds and Abrasions: Treat for shock. Cover the wound with a sterile dressing while stabilization is carried out Control any severe haemorrhaging. Consider analgesia Once the patient is stable Clip the hair around the wound. Before you do this, fill the wound with KY jelly or if the wound is large, fill the periphery of the wound with KY jelly and pack the rest of the wound with sterile saline soaked swabs. This will help to prevent hair from falling into the wound. Moisten the hair with saline to facilitate removal in clumps and inhibit contamination of the wound with multiple fine hairs. Remove contamination, eg grit dirt hair with dressing forceps. DO NOT REMOVE DEEPLY PENERATING FORIEGN BODIES. Large penetrating foreign bodies which protrude from the body should be cut off so that they only protrude above the skin surface. A ring pad dressing can then be applied over the whole wound. Flush the wound mechanically, use copious amounts of non-toxic solution. eg Isotonic sterile saline, syringed into the wound. Take care not to disturb blood clots and not to further contaminate the wound from surrounding skin. Dress the wound. Apply wound dressing appropriate to the type and stage of the wound. Oily ointments should be avoided as they are difficult to remove at subsequent surgery. Likewise, cotton wool should never be applied directly to the wound as it will stick to the wound. If antibiotics are indicated generally parenteral administration is more effective than topical treatments and less cytotoxic on damaged devitalised tissue Closed wounds A Closed Wound is one where the injured does not cause a break in the body covering. There are three types of closed wounds: Contusions (Bruise) A contusion is produced by a blow with a blunt instrument which causes rupture of blood vessels in the skin and in the soft tissues beneath. Signs of a contusion are heat, pain, and swelling. White-skinned animals show discolouration of the skin, which is first red (immediately after the blow), then purple (within a few hours) and finally yellow/green (after several days). Treatment of Contusions Cold compresses. Apply immediately to cause vasoconstriction and thereby reduce the volume of blood entering the damaged area. This reduces swelling and also pain. Application of a pressure bandage will also help to control haemorrhage and reduce swelling. Haematoma Haematomas are soft and usually painless and cool to the touch. They result from rupture of a blood vessel, most often a vein under the skin with bleeding into the connective tissues. Examples include aural haematomas on the ear flaps of dogs and those produced at venipuncture sites if pressure is not applied with the needle is withdrawn. First aid of Haematomas: Bandage the affected area firmly, as soon as possible, or apply firm pressure with a cold compress if bandaging is impractical. 3. Burns Definition: A burn is an injury to the body caused by dry heat, and a scald is caused by wet heat (steam, oil etc.). Burns can also be caused by electrical current, chemicals, radiation etc. Burns are classified /evaluated according to: Depth - superficial in the skin or deep involving underlying tissues. Area involved and % of the body surface affected Cause – dry, scald, electrical radiation etc. All burns cause tissue damage and inflammation with fluid loss from damaged capillaries. Pain can be severe especially when large areas are involved. Superficial burns are more painful than deep burns because the nerves have been damaged in deeper burns. Treatment: If burns are severe and involve more than 50% of the body, euthanasia should be considered. Less severe burns or those involving smaller areas of the body surface can be treated. Initially, immersion of the affected part in cold water, running water, or packing the area with cold packs for 10 minutes, will help to reduce the pain and lessen tissue oedema. Treatment of shock is often required. Aims of Treatment of burns: Remove the source Cool the damaged area as quickly as possible9clip fur to ensure the affected area is identified). Keep patient warm once the initial cooling treatment is complete. Dress wound. Analgesia Splint to limit movement if necessary and or E-collar to prevent self mutilation. Prepare an IV drip. 4. Electric shock Electric shock is most commonly seen in puppies and kittens usually as a result of chewing on electric cords. The severity of problems will vary with the voltage and with the pathway of the current through the body. As the electricity traverses the bodies tissues it is converted to heat. There is coagulation necrosis (tissue death) at the site of entry and exit, and within the striated muscle it passes through. Wounds of the palate, lips, and tongue are frequently seen. Focal necrosis may occur in nerves, spinal cord and brain. Stupor, coma, cardiac arrest or arrhythmias, cardiogenic shock, convulsions, and death are all possible complications. Lung oedema is a more common sequel in small animals and causes laboured breathing and cyanosis (blue mucous membranes from lack of oxygen). It is essential to remember to switch off the power supply before touching the animal, as it may be electrically ‘live’ even though it is clinically dead. If this is not possible then use an electrically non-conducting implement to push the animal away from the electrical source (e.g. dry wood or plastic pole). If the animal is alive on presentation, treatment will depend on the severity of it’s condition. Early treatment often requires oxygen therapy, intravenous fluids, diuretics, bronchodilators, and corticosteroids. These materials and therapeutics should be made ready. 5. Heat stroke Most often seen when animals, frequently dogs, are confined for prolonged periods in hot, poorly ventilated surroundings, especially if they do not have access to water. The animal becomes unable to regulate its body temperature, which gradually rises. Initially the animal is distressed, panting and drooling excessively and restless. The animal becomes weak and its tongue and lips initially appear bright red. Eventually the animal will collapse, go into a coma and subsequently die. On presentation the animal feels burning hot and it’s temperature is off the scale. Treatment: Cool the animal by hosing it with cold water. Administer cooled intravenous fluids. Confine the animal to a cool, airy kennel, preferably with a concrete floor. Lay a wet blanket over the animal to keep the coat wet and reduce it’s insulative properties. If unconscious, swab away saliva. Position the head so that saliva will drain from the mouth instead of into the back of the throat. Give oxygen if the animal is cyanotic (mucous membranes blue) Monitor the temperature every 15 minutes to avoid overcooling the body. When the body temperature reaches 40.5 degrees or less aggressive cooling should be discontinued. Once it is in the normal range, it should be dried off, kept in a cool kennel with access to cold drinking water. Monitor the temperature every 30 minutes to ensure it doesn’t rise again. 6. Convulsions and seizures A convulsion/fit/seizure is usually sudden in onset. The animal having a fit collapses on to its side and goes into violent convulsions. The legs are extended and often paddling in motion, its head pulled back and neck extended; there is involuntary champing of jaws, which results in the foaming saliva from around the lips. Eyes are open and fixed in a stare. Respiration rate is increased and defecation and urination are common during severe fits. Most convulsions subside after a few minutes but occasionally the animal will be experiencing continuous fits. These attacks represent gross overactivity of the central nervous system ‘circuits’ and any extra stimulus usually only worsens the situation and prolongs the fit. Seizures may be primary (epileptiform, more common in dogs than cats, usually seen in young animals, 1 to 3 years of age) or secondary. Secondary fits often occur in older animals following brain damage by diseases (such as distemper), trauma (such as a blow to the head), or toxaemia (as seen in uraemia or poisoning cases, e.g. organophosphates, slug bait). Treatment for seizures: Owners should be advised to get the animal to the surgery as soon as possible. Owners should be advised to keep visual and auditory stimuli to a minimum. If it is possible the animal should be kept in a dark and quiet area. Owners should remain with the animal but be advised not to touch it (minimise tactile stimulus). Owners need to remain calm. Once at the surgery, the animal should be placed in a dark, quiet cage until the vet arrives. Valium and Barbiturates should be prepared as it may be necessary to sedate or anaesthetise the animal to control the seizures. Under no circumstances should the owner or vet nurse attempt to put a hand into the animal’s mouth until the convulsions subside. Such attempts are fruitless and may result in severe bites. 8. Fractures Definition: A fracture is a forcible break in the continuity of bony tissue, i.e. the bone is broken. Classification of Fractures(can be by anatomical description, type of displacement, direction of the fracture line, number or types of fractures, by joint affected etc). Some of the more commonly used terminologies are the following: Simple fracture is one where there is one fracture line, e.g. the bone is broken cleanly into two pieces. Comminuted fracture is a complex fracture creating three or more fragments. Greenstick fracture is an incomplete fracture. The bone has a fissure in one cortex but there is not a complete separation of bone at the fracture line. These occur most frequently in immature animals. Open fracture is one where there is a wound communicating between the skin or mucous membranes and the fracture site. This allows contamination of the fracture site with bacteria. Closed fracture is one where there is no overlying wound. Pathological fracture results from normal use of a bone weakened by a disease process. The disease process may be generalised (for example, a nutritional deficiency of calcium and phosphate causing weak bones), or localised (for example, a tumour affecting the bone). Avulsion fracture occurs when a bone prominence is torn away from the rest of the bone, usually by the pull of a muscle. For further information and examples see your text book Clinical signs of fractures Most fractures are caused by trauma. In the initial phases a fracture is an inflammatory lesion and many of the clinical signs can be attributed to acute inflammation. The major clinical signs seen are: Loss of function and unnatural gait if a limb is involved Visible or palpable deformity of the affected bone Abnormal mobility at the fracture site Crepitus when the injured part is moved. Pain localised to the affected bone Local swelling, bruising and heat due to haemorrhage from the surrounding tissues First Aid of Fractures: Animals with broken bones are in pain. They may bite and must be safely restrained prior to administering first aid. A muzzle is often needed. Attend to life threatening problems first. Always ensure that there is an adequate airway, breathing and circulation. Many times these animals also have soft tissue injuries that are more life threatening than the broken bone. Shock is often a problem and fluid therapy is often needed early in treatment. Cover any open wounds with a clean (preferably sterile) dressing Immobilise the fracture prior to moving the animal and cage rest to minimize movement till surgery If a spinal fracture is suspected, the entire spine should be immobilised by strapping the animal to any straight and rigid structure of suitable length. Arrest haemorrhage. Support Dressings applied must include a joint above and below the fracture site eg Robert Jones and other Bandaging, Splinting. These may not be possible to apply with the animal conscious. If both arterial and venous flows are obstructed, the toes may become swollen and cold. If any swelling should occur, the dressings must be removed immediately and replaced by looser bandaging. See your text book for further details