Presentation on Neurological Health Services
advertisement

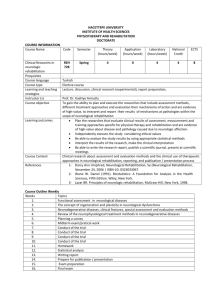
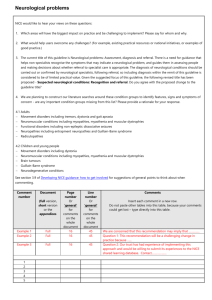
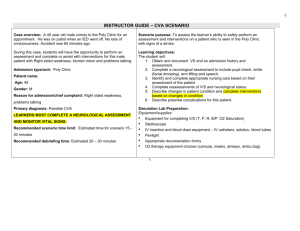
Presentation on Neurological Health Services Joint Oireachtas Committee on Health and Children 11th February 2014 The Neurological Alliance of Ireland The Neurological Alliance of Ireland is the national umbrella for over 30 organisations representing people with neurological conditions and their families. It the only national umbrella dedicated to representing issues affecting this population, estimated to be over 700,000 people. The Neurological Alliance of Ireland has played a significant role in developing the policy agenda for neurological health services in this country, including through their framework document Neurological Conditions in Ireland: A challenge for healthcare; an opportunity for change. The Neurological Alliance represents the interests of patients and patient organisations on a range of fora, including the programme teams for the national clinical programmes in neurology and rehabilitation medicine. Neurological Health Services in Ireland There are a number of characteristics of neurological care in Ireland. -Long waiting lists for access to neurospecialists, including for diagnosis -Multidisciplinary care is hampered by extremely stretched and underresourced teams, where they exist, in some neurology centers, there is little access to multidisciplinary support -Community aftercare and rehabilitation is extremely underresourced and underdeveloped. There is only one specialised neurorehabilitation community team established in Ireland, working in the Mid West region. All of these combine to result in access to neurological care which falls far below what would be expected in a developed country. There is a largely disjointed and uncoordinated approach in this country for those who require neurological care and neuro-rehabilitation. Individuals and families require services on a continuum basis due to the nature and often complexity of the neurological conditions they are living with. The current service delivery model is a largely episodic model, almost exclusively medical in nature and does not reflect nor meet the real needs. This is costly and ineffective, not good practice and incredibly frustrating for patients and families. Our presentation concentrates on Community Aftercare and Neurorehabilitation Access to rehabilitation services was highlighted in a case reported on just two weeks ago in the Irish Times Health Supplement where a victim of traumatic brain injury was informed that there was a 4 month waiting list for one of three high dependency beds in the National Rehabilitation Hospital. The then clinical lead of the national rehabilitation medicine programme made the following statement in an interview with the Irish Medical Times in 2011: “There are insufficient numbers of rehabilitation medicine consultants, insufficient access to specialist rehabilitation at a local level, lack of support for primary care teams in managing very challenging cases and lack of support for the patient and their families. Even if a patient has been through the services of the NRH, once they get discharged they’re very often left in a kind of limbo.” The Neurological Alliance of Ireland carried out a national survey in 2013 asking patients and family members about their access to neurorehabilitation services. The results highlighted the critical issue of access to therapies in the community: 40% could not access neuropsychology services 25% could not access physiotherapy or OT services to meet their needs The ongoing pressure on therapy services, due to the recruitment embargo and lack of investment, is impacting significantly on people with neurological conditions. Earlier this year for example, it was highlighted that there was no adult speech and language therapy service in Waterford city, resulting in a devastating impact on adults with neurological conditions such as acquired brain injury and Parkinson’s disease. The NAI is currently carrying out a national survey of people with neurological conditions and their families with over 550 responses to date. The survey questions people about their experiences over the past 3 years to assess the impact of the most significant cuts in health services in recent years. Preliminary findings from the survey confirm what has been communicated by patient organisations working day to day with these individuals: 57% impacted by increasing costs of medication 25% reporting having to purchase physiotherapy services on a private basis 17% have had a medical card refused, 10% have had their card withdrawn 84% reporting anxiety about future health cutbacks It is difficult to propose comprehensive solutions to the complex and wide ranging challenges affecting neurological care in Ireland in the scope of this brief presentation. However it is clear that steps need to be taken to address the critical lack of aftercare services for people after diagnosis or onset of a neurological condition There are salient points which can be made 1. Ireland could address a critical issue in relation to neurorehabilitation by putting in place the community neurorehabilitation teams recommended in the national neurorehabilitation strategy published in 2011. To date there is only one such team in the Mid West. The steady erosion of community based therapy provision and the lack of new investment will significantly hamper the establishment of these teams. Case management is essential for those with complex needs such as people with acquired brain injury to avoid the type of disjointed care experienced by these individuals. 2. Cuts in community health services are critically impacting on people with neurological conditions who are among the most dependent on such supports. Cuts to home care packages are forcing people to stay in acute units or be discharged home with inadequate care. Either way it leads to long term pressure on the acute system. 3. The medical card is a vital portal to services for those with chronic illness. Not having a medical card excludes people with neurological conditions from many of these supports. 4. Ireland is uniquely reliant on not for profit organisations to provide neurological health services that are normally provided by the State in other jurisdictions. The reality is that the infrastructure of community based neurological care is hugely reliant on the services provided by patient organisations. Disability organisations have seen a 15% drop in their funding in recent years and many have had to close or curtail services to people with neurological conditions. The message which we want members of the committee to take from our presentation is that: 1. Community aftercare for people with a neurological condition in Ireland has historically been underdeveloped and underresourced and well below what is routinely available in other countries 2. The services that are in place are being decimated by cuts to community health services which are significantly affecting the quality of care available for people with neurological conditions in this country.