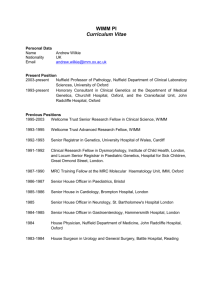
WIMM PI Curriculum Vitae
advertisement

WIMM PI Curriculum Vitae Personal Data Name Nationality Email Andrew Oliver Mungo Wilkie UK andrew.wilkie@imm.ox.ac.uk Present Position 2003-present Nuffield Professor of Pathology, Nuffield Department of Clinical Laboratory Sciences, University of Oxford 1993-present Honorary Consultant in Clinical Genetics at the Department of Medical Genetics, Churchill Hospital, Oxford, and the Craniofacial Unit, John Radcliffe Hospital, Oxford Previous Positions 1995-2003 Wellcome Trust Senior Research Fellow in Clinical Science, WIMM 1993-1995 Wellcome Trust Advanced Research Fellow, WIMM 1992-1993 Senior Registrar in Genetics, University Hospital of Wales, Cardiff 1991-1992 Clinical Research Fellow in Dysmorphology, Institute of Child Health, London, and Locum Senior Registrar in Paediatric Genetics, Hospital for Sick Children, Great Ormond Street, London. 1987-1990 MRC Training Fellow at the MRC Molecular Haematology Unit, IMM, Oxford 1986-1987 Senior House Officer in Paediatrics, Bristol 1985-1986 Senior House in Cardiology, Brompton Hospital, London 1985 Senior House Officer in Neurology, St. Bartholomew's Hospital London 1984-1985 Senior House Officer in Gastroenterology, Hammersmith Hospital, London 1984 House Physician, Nuffield Department of Medicine, John Radcliffe Hospital, Oxford 1983-1984 House Surgeon in Urology and General Surgery, Battle Hospital, Reading Research Achievements As a practicing clinical geneticist I aim to exploit the molecular genetic analysis of individual patients presenting with congenital disorders, both to reveal the cause of their condition and to uncover genetic principles of wider biological and pathological relevance. Since starting as a group leader in Oxford in 1993 I have fostered very close clinical contacts with the craniofacial unit in Oxford, one of five covering the entire UK. As a result of this ongoing 20year collaboration, the Oxford patients probably represent the best characterized cohort of craniofacial patients internationally from a molecular genetic standpoint. During this period my group has discovered many genes that, when mutated, cause serious craniofacial conditions, notably various types of craniosynostosis (premature fusion of the cranial sutures). Many of these discoveries have led to the development of molecular genetic diagnostic tests now in clinical use; the Churchill Hospital provides one of two national diagnostic services for craniofacial disorders and I sign off all lab reports issued by the service. Work on mouse models carrying equivalent mutations has helped to further elucidate the developmental mechanisms of several craniosynostosis syndromes. Starting from the identification of mutations in fibroblast growth factor receptor 2 (FGFR2) in Apert syndrome (a cause of craniosynostosis), and the deduction that these mutations were arising with unexpectedly high frequency in the healthy fathers, my group discovered a novel mechanism whereby pathogenic mutations within the testis can promote the enrichment of mutant spermatogonia. Recent work has identified similar mutations in testicular tumours, linking the processes of somatic and germline mutation to events occurring in the same cell. This work provides fundamental novel insights into mutational processes that may have implications beyond congenital malformations to include common complex diseases such as cancer and neuropsychiatric disorders. What are the Future Aims of Your Current Group? I plan to continue to pursue the dual themes of the molecular basis of craniofacial malformation and consequences of selfish spermatogonial mutation. The investigation of both themes is substantially assisted by recent developments in DNA sequencing, making this a “golden era” to be undertaking such work. In the case of craniofacial malformation, exome and whole genome sequencing are allowing the discovery of disease-causing genes at an unprecedented rate; our group has identified four novel, validated genes over the past 2 years indicating that our current understanding of molecular pathogenesis is far from complete. With our excellent clinical links we are strongly placed to continue to mine our sample resource for novel pathogenic mutations, with the aim of achieving a more complete picture of the diversity of genetic lesions giving rise to craniofacial disorders. Alongside this we are investigating the pathophysiological mechanisms of craniosynostosis, particularly using carefully chosen mouse models. An emerging theme is that many of the genes mutated in these developmental malformations are also mutated in cancer, raising the question whether abnormal development could be targeted using anticancer drugs – although many logistical challenges would have to be overcome to make this a reality. In our further work on spermatogonial mutation, we would like to identify the mutational events directly in testes by using a combination of immunohistochemistry, microdissection and high throughput sequencing. Ultimately, our long-term aim is to document the frequency spectrum of every mutation in the human genome, but in the short-term we want to identify which genes are most strongly governed by this mechanism. How do These Aims Contribute to the Understanding and/or Management of Human Disease The work on the molecular basis of craniofacial malformations has led to the introduction of many new diagnostic genetic tests and the development of Oxford as a leading international centre in this work. Such molecular genetic diagnosis provides the cornerstone for giving families accurate diagnostic information and informed genetic counseling. In addition it is increasingly recognised that accurate diagnosis informs surgical prognosis and is therefore important in the long-term clinical management of patients. This work also contributes to understanding the different pathophysiological mechanisms that underlie craniosynostosis. Whilst the work on selfish spermatogonial selection is aimed at providing fundamental insights into disease rather than novel tests, it can nevertheless yield valuable data for genetic counselling – for example, it has demonstrated that certain de novo mutations are very unlikely to be associated with germinal mosaicism, thus potentially avoiding invasive prenatal diagnostic tests that are potentially harmful to the fetus. Lay Summary of Research About 1 in 2,000 children is born with a serious malformation of the skull: the most frequent type is termed “craniosynostosis”, the premature fusion of the cranial sutures. Parents want to know why this has happened, whether it could happen again, and whether any tests are available to determine the answers to these questions. Working closely with surgeons in Oxford who treat these children, our laboratory aims to identify new genetic causes of these malformations. Over the past 20 years we have identified over ten new causative genes, which have been introduced into laboratory testing in the NHS and around the world. Using modern technologies that combine the ability to sequence an entire human genome in a single experiment with computational methods to analyse the data, we now aim to compile a comprehensive compendium of the possible gene mutations, and their relative frequency over the next few years, so that more families can get answers to their questions. Additional benefits of this work are that we can learn more both about how the skull develops, and why the causative genetic changes (mutations) arise. To answer the first question, we need to use mice that recapitulate several features of the human disorder, since it would be unethical to investigate the origins of developmental malformation in the human fetus. Working on the mechanisms of mutation, we have stumbled on an unexpected process whereby changes to genes arising in the healthy father’s testis that are harmful in the offspring, are paradoxically beneficial to cells within the testis itself. We term this process “selfish selection”. Again exploiting new technologies, the other major thrust of our laboratory is to explore the wider consequences of this new mechanism for causing disease. All Publications Over the Past 5 Years (*corresponding author) Wilkie AOM*, Byren JC, Hurst JA, Jayamohan J, Johnson D, Knight SJL, Lester T, Richards PG, Twigg SRF & Wall SA (2010). Prevalence and complications of single gene and chromosomal disorders in craniosynostosis. Pediatrics 126:e391-e400. Bochukova EG, Soneji S, Wall SA & Wilkie AOM* (2010). Scalp fibroblasts have a shared expression profile in monogenic craniosynostosis. J Med Genet 47:803-808. Jenkins D, Baynam G, De Catte L, Elcioglu N, Gabbett MT, Hudgins L, Hurst JA, Jehee FS, Oley C & Wilkie AOM* (2011). Carpenter syndrome: extended RAB23 mutation spectrum and analysis of nonsense-mediated mRNA decay. Hum Mutat 32:E2069-78. Hurst JA, Jenkins D, Vasudevan PC, Kirchhoff M, Skovby F, Rieubland C, Gallati S, Rittinger O, Kroisel PM, Johnson D, Biesecker LG & Wilkie AOM* (2011). Metopic and sagittal synostosis in Greig cephalopolysyndactyly syndrome: five cases with intragenic mutations or complete deletions of GLI3. Eur J Hum Genet 19:757-762 Nieminen P, Morgan NV, Fenwick AL, Parmanen S, Veistinen L, Mikkola ML, van der Spek PJ, Giraud A, Judd L, Arte S, Brueton LA, Wall SA, Mathijssen IMJ, Maher ER, Wilkie AOM, Kreiborg S & Thesleff I (2011). Inactivation of IL11 signaling causes craniosynostosis, delayed tooth eruption and supernumerary teeth. Am J Hum Genet 89:67-81. Lim J, Goriely A, Turner GDH, Ewen KA, Jacobsen GK, Graem N, Wilkie AOM & Rajpert-De Meyts E (2011). OCT2, SSX and SAGE1 reveal the phenotypic heterogeneity of spermatocytic seminoma reflecting distinct subpopulations of spermatogonia. J Pathol 224:473-483. Babbs C, Stewart HS, Williams LJ, Connell L, Goriely A, Twigg SRF, Smith K, Lester T & Wilkie AOM* (2011). Duplication of the EFNB1 gene in familial hypertelorism: imbalance in ephrin-B1 expression and abnormal phenotypes in humans and mice. Hum Mutat 32:930-938. Fenwick AL, Bowdin SC, Klatt REM & Wilkie AOM (2011). A deletion of FGFR2 creating a chimeric IIIb/IIIc exon in a child with Apert syndrome. BMC Med Genet 12:122. Barroso E, Pérez-Carrizosa V, García-Recuero I, Glucksman MJ, Wilkie AO, García-Minaur S & Heath KE (2011). Mild isolated craniosynostosis due to a novel FGFR3 mutation, p.Ala334Thr. Am J Med Genet A 155:3050-3053. Sharma VP, Wall SA, Lord H, Lester T & Wilkie AOM* (2012). Atypical Crouzon syndrome with a novel Cys62Arg mutation in FGFR2 presenting with sagittal synostosis. Cleft Palate Craniofac J 49:373-377. Lim J, Maher GJ, Turner GDH, Dudka-Ruszkowska W, Taylor S, Rajpert-De Meyts E, Goriely A & Wilkie AOM* (2012). Selfish spermatogonial selection: evidence from an immunohistochemical screen in testes of elderly men. PLoS ONE 7:e42382. Twigg SRF, Lloyd D, Jenkins D, Elcioglu N, Cooper CDO, Al-Sannaa N, Annagür A, Gillessen-Kaesback G, Stefanova I, Knight SJL, Goodship JA, Keavney B, Beales PL, Gileadi O, McGowan SJ & Wilkie AOM* Mutations in the multidomain protein MEGF8 identify a new subtype of Carpenter syndrome associated with defective lateralization. Am J Hum Genet 91:897-905. Eley KA, Johnson D, Wilkie AOM, Jayamohan J, Richards P & Wall SA (2012). Raised intracranial pressure is frequent in untreated non-syndromic unicoronal synostosis and does not correlate with severity of phenotypic features. Plast Reconstr Surg 130:690e697e. Bendon CL, Fenwick AL, Hurst JA, Nürnberg G, Nürnberg P, Wall SA, Wilkie AOM & Johnson D (2012). Frank-ter Haar syndrome associated with sagittal craniosynostosis and raised intracranial pressure. BMC Med Genet 13:104. Justice CM, Yagnik G, Kim Y, Peter I, Jabs EW, Erazo M, Ye X, Ainehsazan E, Shi L, Cunningham ML, Kimonis V, Roscioli T, Wall SA, Wilkie AOM, Stoler J, Richtsmeier JT, Heuzé Y, Sanchez-Lara PA, Buckley MF, Druschel CM, Mills JL, Caggana M, Romitti PA, Kay DM, Senders C, Taub PJ, Klein OD, Boggan J, Zwienenberg-Lee M, Naydenov C, Kim J, Wilson AF & Boyadjiev SA (2012). A genome-wide association study identifies susceptibility loci for non-syndromic sagittal craniosynostosis near BMP2 and within BBS9. Nature Genet 44:1360-1364. Varvagiannis K, Stefanidou A, Gyftodimou Y, Lord H, Williams L, Sarri C, Pandelia E, Bazopoulou-Kyrkanidou E, Noakes C, Lester T, Wilkie AOM & Petersen MB (2013). Pure de novo partial trisomy 6p in a girl with craniosynostosis. Am J Med Genet A 161A:343351. Shanks ME, Downes SM, Copley RR, Lise S, Broxholme J, Hudspith KAZ, Kwasniewska A, Davies WIL, Hankins MW, Packham E, Clouston P, Seller A, Wilkie AOM, Taylor JC, Ragoussis J & Németh (2013). Next Generation Sequencing (NGS) as a diagnostic tool for retinal degeneration reveals a much higher detection rate in early onset disease. Eur J Hum Genet 21:274-280. Vodopiutz J, Zoller H, Fenwick AL, Arnhold R, Schmid M, Prayer D, Müller T, Repa A, Pollak A, Aufricht C, Wilkie AOM & Janecke AR (2013). Homozygous SALL1 mutation causes a novel multiple congenital anomaly - mental retardation syndrome. J Pediatr 162:612-617. Sharma VP, Fenwick AL, Brockop MS, McGowan SJ, Goos JAC, Hoogeboom AJM, Brady AF, Jeelani NuO, Lynch SA, Mulliken JB, Murray DJ, Phipps JM, Sweeney E, Tomkins SE, Wilson LC, Bennett S, Cornall RJ, Broxholme J, Kanapin A, WGS500, Johnson D, Wall SA, van der Spek PJ, Mathijssen IMJ, Maxson RE, Twigg SRF & Wilkie AOM* (2013). Mutations of TCF12, encoding a basic-helix-loop-helix partner of TWIST1, are a frequent cause of coronal craniosynostosis. Nature Genet 45:304-307. Twigg SRF, Vorgia E, McGowan SJ, Peraki I, Fenwick AL, Sharma VP, Allegra M, Zaragkoulias A, Akha ES, Knight SJL, Lord H, Lester T, Izatt L, Lampe AK, Mohammed SN, Stewart FJ, Verloes A, Wilson LC, Healy C, Sharpe PT, Hammond P, Hughes J, Taylor S, Johnson D, Wall SA, Mavrothalassitis G & Wilkie AOM* (2013). Reduced dosage of ERF causes complex craniosynostosis in humans and mice, and links ERK1/2 signalling to regulation of osteogenesis. Nature Genet 45:308-313. Twigg SRF, Babbs C, van den Elzen MEP, Goriely A, Taylor S, McGowan SJ, Giannoulatou E, Lonie L, Ragoussis I, Akha ES, Knight SJL, Ceide RZ, Hoogeboom AJM, PassosBueno MR, Pober BR, Toriello HV, Wall SA, Brunner HG, Mathijssen IMJ & Wilkie AOM* (2013). Cellular interference in craniofrontonasal syndrome: males mosaic for mutations in the X-linked EFNB1 gene are more severely affected than true hemizygotes. Hum Mol Genet 22:1654-1662. Jay S, Wiberg A, Swan M, Lester T, Williams LJ, Taylor IB, Johnson D & Wilkie AOM* (2013). The fibroblast growth factor receptor 2 p.Ala172Phe mutation in Pfeiffer syndrome – history repeating itself. Am J Med Genet 161A:1158-1163. Giannoulatou E, McVean G, Taylor IB, McGowan SJ, Maher GJ, Iqbal Z, Pfeifer SP, Turner I, Burkitt-Wright EMM, Shorto J, Itani A, Turner K, Gregory L, Buck D, Rajpert-De Meyts E, Looijenga LHJ, Kerr B, Wilkie AOM* & Goriely A* (2013). Contributions of intrinsic mutation rate and selfish selection to levels of de novo HRAS mutations in the paternal germline. Proc Natl Acad Sci USA 110:20152-20157. Favaro FP, Alvizi L, Zechi-Ceide RM, Bertola D, Felix TM, de Souza J, Raskin S, Twigg SRF, Weiner AMJ, Armas P, Margarit E, Calcaterra NB, Andersen GR, McGowan S, Wilkie AOM, Richieri-Costa A, de Almeida MLG & Passos-Bueno MR (2014). A noncoding expansion in EIF4A3 causes Richieri-Costa-Pereira syndrome, a craniofacial disorder associated with limb defects. Am J Hum Genet 94:120-128. Williamson KA, Rainger J, Floyd JA, Ansari M, Meynert A, Aldridge KV, Rainger JK, Anderson CA, Moore AT, Hurles ME, Clarke A, van Heyningen V, Verloes A, Taylor MS, Wilkie AOM, UK10K Consortium & Fitzpatrick DR (2014). Heterozygous loss-of-function mutations in YAP1 cause both isolated and syndromic optic fissure closure defects. Am J Hum Genet 94:295-302. van den Elzen MEP, Twigg SRF, Goos JAC, Hoogeboom AJM, van den Ouweland AMW, Wilkie AOM & Mathijssen IMJ (2014). Phenotypes of craniofrontonasal syndrome in patients with a pathogenic mutation in EFNB1. Eur J Hum Genet 22:995-1001. Rimmer A, Phan H, Mathieson I, Iqbal Z, Twigg SRF, 500 Whole-Genome Sequences (WGS500) Consortium, Wilkie AOM, McVean G & Lunter G (2014). Integrating mapping-, assembly- and haplotype-based approaches for calling variants in clinical sequencing applications. Nature Genet 46:912-918. Fenwick AL, Goos JAC, Rankin J, Lord H, Lester T, Hoogeboom AJM, van den Ouweland AMW, Wall SA, Mathijssen IMJ & Wilkie AOM (2014). Apparently synonymous substitutions in FGFR2 affect splicing and result in mild Crouzon syndrome. BMC Med Genet 15:95. Babbs C, Lloyd D, Pagnamenta AT, Twigg SRF, Green J, McGowan SJ, Mirza G, Naples R, Sharma VP, Volpi EV, Buckle VJ, Wall SA, Knight SJ, International Molecular Genetic Study of Autism Consortium (IMGSAC), Parr JR &51 Wilkie AOM (2014). De novo and rare inherited mutations implicate the transcriptional coregulator TCF20/SPBP in autism spectrum disorder. J Med Genet. 51:737-747. Taylor JC, Martin HC, Lise S, Broxholme J, Cazier J-B, Rimmer A, Kanapin A, Lunter G, Fiddy S, Allan C, Aricescu AR, Attar M, Babbs C, Becq J, Beeson D, Bento C, Bignell P, Blair E, Buckle VJ, Bull K, Cais O, Cario H, Chapel H, Copley RR, Cornall R, Craft J, Dahan K, Davenport EE, Dendrou C, Devuyst O, Fenwick AL, Flint J, Fugger L, Gilbert RD, Goriely A, Green A, Greger IH, Grocock R, Gruszczyk AV, Hastings R, Hatton E, Higgs D, Hill A, Holmes C, Howard M, Hughes L, Humburg P, Johnson D, Karpe F, Kingsbury Z, Kini U, Knight J, Krohn J, Lamble S, Langman C, Lonie L, Luck J, McCarthy D, McGowan SJ, McMullin MF, Miller KA, Murray L, Németh AH, Nesbit MA, Nutt D, Ormondroyd E, Oturai AB, Pagnamenta A, Patel SY, Percy M, Petousi N, Piazza P, Piret SE, Polanco G, Popitsch N, Powrie F, Pugh C, Quek L, Robbins PA, Robson K, Russo A, Sahgal N, van Schouwenburg PA, Schuh A, Silverman E, Simmons A, Sørensen PS, Sweeney E, Thakker RV, Tomlinson I, Trebes A, Twigg SRF, Uhlig H, Vyas P, Vyse T, Wall SA, Watkins H, Whyte MP, Witty L, Wright B, Yau C, Buck D, Humphray S, Ratcliffe PJ, Bell JI, Wilkie AOM, Bentley D, Donnelly P & McVean G. Factors influencing success of clinical genome sequencing across a broad spectrum of disorders. Nature Genet 47:717-726. Twigg SRF, Forecki J, Goos JAC, Richardson ICA, Hoogeboom AJM, Van den Ouweland AMW, Swagemakers SMA, Lequin MH, Van Antwerp D, McGowan SJ, Westbury I, Miller KA, Wall SA, WGS500 Consortium, van der Spek PJ, Mathijssen IMJ, Pauws E, Merzdorf CS & Wilkie AOM (2015). Gain-of-function mutations in ZIC1 are associated with coronal craniosynostosis and learning disability. Am J Hum Genet 97:378-88. Fennell N, Foulds N, Johnson DS, Wilson LC, Wyatt M, Robertson SP, Johnson D, Wall SA &Wilkie AOM. Association of mutations in FLNA with craniosynostosis. Eur J Hum Genet, in press, PMID 25873011. Piard J, Rozé V, Czorny A, Lenoir M, Valduga M, Fenwick AL, Wilkie AOM & Van Maldergem L. TCF12 microdeletion in a 72 year-old woman with intellectual disability. Am J Med Genet A, in press, PMID 25871887. Reviews Johnson D & Wilkie AOM* (2011). Craniosynostosis. Eur J Hum Genet 19:369-376. Goriely A* & Wilkie AOM* (2012). Paternal age effect mutations and selfish spermatogonial selection: causes and consequences for human disease. Am J Hum Genet 90:175-200. Clarke AJ, Cooper DN, Krawczak M, Tyler-Smith C, Wallace HM, Wilkie AOM, Raymond FL, Chadwick R,Craddock N, John R, Gallacher J & Chiano M (2012). ‘Sifting the significance from the data’ - the impact of high-throughput genomic technologies on human genetics and health care. Hum Genomics 6:11. Goriely A, McGrath JJ, Hultman CM, Wilkie AOM & Malaspina D (2013). "Selfish spermatogonial selection": a novel mechanism for the association between advanced paternal age and neurodevelopmental disorders. Am J Psych 170:599-608. Köhler S, Doelken SC, Mungall CJ, Bauer S, Firth HV, Bailleul-Forestier I, Black GCM, Brown DL, Brudno M, Campbell J, Fitzpatrick DR, Eppig JT, Jackson AP, Freson K, Girdea M, Helbig I, Hurst JA, Jähn J, Jackson LG, Kelly AM, Ledbetter DH, Mansour S, Martin CL, Moss C, Mumford A, Ouwehand WH, Park SM, Riggs ER, Scott RH, Sisodiya S, Vooren SV, Wapner RJ, Wilkie AOM, Wright CF, Vulto-van Silfhout AT, Leeuw ND, de Vries BBA, Washingthon NL, Smith CL, Westerfield M, Schofield P, Ruef BJ, Gkoutos GV, Haendel M, Smedley D, Lewis SE & Robinson PN (2014). The Human Phenotype Ontology project: linking molecular biology and disease through phenotype data. Nucleic Acids Res 42:D966-974. Maher GJ, Goriely A & Wilkie AOM (2014). Cellular evidence for selfish spermatogonial selection in aged human testes. Andrology 2:304-314. Twigg, SRF & Wilkie AOM (2015). A genetic-pathophysiological framework for craniosynostosis. Am J Hum Genet 97:359-77. Twigg, SRF & Wilkie AOM (2015). New insights into craniofacial malformations. Hum Mol Genet, in press, PMID 26085576. Book chapters Wilkie AOM (2013). Genetics of craniosynostosis. In: Maloy S & Hughes K (eds). Brenner’s Encyclopedia of Genetics 2nd edition, Academic Press, San Diego, Vol 2 pp. 208–211. Ten Key Publications Throughout your Career (* Corresponding author) Wilkie AOM, Lamb J, Harris PC, Finney RD & Higgs DR (1990). A truncated human chromosome 16 associated with α thalassaemia is stabilized by addition of telomeric repeat (TTAGGG)n. Nature 346:868-871. Wilkie AOM*, Slaney SF, Oldridge M, Poole MD, Ashworth GJ, Hockley AD, Hayward RD, David DJ, Pulleyn LJ, Rutland P, Malcolm S, Winter RM & Reardon W (1995). Apert syndrome results from localized mutations of FGFR2 and is allelic with Crouzon syndrome. Nature Genet 9:165-172. Moloney DM, Slaney SF, Oldridge M, Wall SA, Sahlin P, Stenman G & Wilkie AOM* (1996). Exclusive paternal origin of new mutations in Apert syndrome. Nature Genet 13: 48-53. Wilkie AOM*, Tang Z, Elanko N, Walsh S, Twigg SRF, Hurst JA, Wall SA, Chrzanowska KH & Maxson RE Jr (2000). Functional haploinsufficiency of the human homeobox gene MSX2 causes defects in skull ossification. Nature Genet 24: 387-390. Goriely A, McVean GAT, Röjmyr M, Ingemarsson B & Wilkie AOM* (2003). Evidence for selective advantage of pathogenic FGFR2 mutations in the male germline. Science 301:643-646. Twigg SRF, Kan R, Babbs C, Bochukova EG, Robertson SP, Wall SA, Morriss-Kay GM & Wilkie AOM* (2004). Mutations of ephrin-B1 (EFNB1), a marker of tissue boundary formation, cause craniofrontonasal syndrome. Proc Natl Acad Sci USA 101:8652-8657. Goriely A, McVean GAT, van Pelt AMM, O’Rourke AW, Wall SA, de Rooij DG & Wilkie AOM* (2005). Gain-of-function amino acid substitutions drive positive selection of FGFR2 mutations in human spermatogonia. Proc Natl Acad Sci USA 102:6051-6056. Goriely A, Hansen RMS, Taylor IB, Olesen IA, Jacobsen GK, McGowan SJ, Pfeifer SP, McVean GAT, Rajpert-De Meyts E & Wilkie AOM* (2009). Activating mutations in FGFR3 and HRAS reveal a shared genetic origin for congenital disorders and testicular tumors. Nature Genet 41:1247-1252. Sharma VP, Fenwick AL, Brockop MS, McGowan SJ, Goos JAC, Hoogeboom AJM, Brady AF, Jeelani NuO, Lynch SA, Mulliken JB, Murray DJ, Phipps JM, Sweeney E, Tomkins SE, Wilson LC, Bennett S, Cornall RJ, Broxholme J, Kanapin A, WGS500, Johnson D, Wall SA, van der Spek PJ, Mathijssen IMJ, Maxson RE, Twigg SRF & Wilkie AOM* (2013). Mutations of TCF12, encoding a basic-helix-loop-helix partner of TWIST1, are a frequent cause of coronal craniosynostosis. Nature Genet 45:304-307. Twigg SRF, Vorgia E, McGowan SJ, Peraki I, Fenwick AL, Sharma VP, Allegra M, Zaragkoulias A, Akha ES, Knight SJL, Lord H, Lester T, Izatt L, Lampe AK, Mohammed SN, Stewart FJ, Verloes A, Wilson LC, Healy C, Sharpe PT, Hammond P, Hughes J, Taylor S, Johnson D, Wall SA, Mavrothalassitis G & Wilkie AOM* (2013). Reduced dosage of ERF causes complex craniosynostosis in humans and mice, and links ERK1/2 signalling to regulation of osteogenesis. Nature Genet 45:308-313. Markers of Esteem 2000 Professor of Genetics in the recognition of distinction exercise, University of Oxford 2002 Oon International Prize in Preventive Medicine, Downing College, Cambridge and Cambridge University Medical School 2002 Fellow of the Academy of Medical Sciences 2006 Member of European Molecular Biology Organisation 2013 Fellow of the Royal Society Current Grant Support 1.11.10-31.10.15 Wellcome Trust Programme Grant: Selfish mutations in the testis: impact on evolution and disease. £1,135,718 ref 091182/Z/10/Z 1.2.14-31.1.19 Wellcome Trust Senior Investigator Award: Mutations in malformation and disease. £1,687,339 ref. 102731/Z/13/Z 1.01.15-31.12.16 National Institutes of Health: Nonsyndromic Craniosynostosis: Phenotype/Genotype Study (Co-investigator; PIs Simeon Boyd and Paul Romitti) $211,608 ref. 2R01DE016886-06A1 1.04.15-31.03.16 NIHR Oxford Biomedical Research Centre Genomic Medicine Theme: Genetics of craniosynostosis. £97,708 (PI; £25k consumables plus salaries for predoc RA and postdoc RA)