Health Psychology Session One: Intro Psych aids: understanding
advertisement

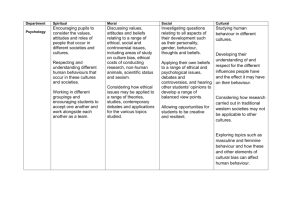
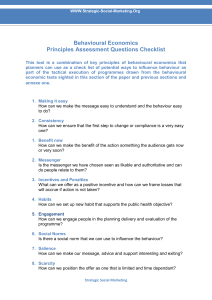
Health Psychology Session One: Intro Psych aids: understanding how beliefs shape help seeking, perceptions, reporting and adherence Studies patients, providers and managers Behaviourism: how does reward and punishment affect behaviour – classical (learn by association – can only pair 2 stimuli therefore change assoc treat phobia) and operant conditioning (positive reinforcement) Social: how thoughts and feelings are affected by social environment e.g. obedience Cognitive: perception, memory etc – social cognition – how people make sense of social world e.g. effects how clinicians behave with patients Dual pathway: psych affects health directly and indirectly Psych clinically applied: awareness, intervention and therapy Session Two: Health Behaviours Good (sleep, healthy eating), protective (screening) and impairing (alcohol, drugs) Biopsychsocial model states all aspect affects health directly or indirectly Factors: background (gender, SES), stable (personality), social (family influence, support) and situational Health Behaviour Model: to understand why people do not attend screening: perceived threat (susceptibility, severity) and perceived efficacy (benefits and barriers) Theory of Planned Behaviour: behaviour attitude (beliefs & outcomes - +ve or –ve), subjective norm (norm beliefs & motivation to comply), perceived behavioural control (control & self efficacy) affect behaviour Transtheorectical model: precontemplation – contemplation – prep – action – maintenance – relapse Stable: emotional disposition (+ve or –ve affect), generalised expectancies (LoC and self efficacy), explanatory styles (internal or external attributions) Session Three: Illness Behaviour Illness behaviour: behaviours engaged in once patients believes they are ill Illness beliefs: beliefs about cause, course and treatment Background, stable (-ve affect notice more symp and ILoC better outcomes but less symp), social (lay referral, if you think your healthy report fewer symp), situational (stress competition for cues) Understanding of illness: identity, cause, times, consequence, control-cure Self regulatory model: understand adaption and coping Session Four: Preventative Medicine Prevention: primary (health promotion), secondary (screening), tertiary (rehab) Screening: population (mammograms etc.), self, opportunistic (depression, hep in preg) Uptake: patient: is screening normal, relevant, high SES women attend more, ILoC increase self screen. Provider: if recommended by HCP more likely uptake. Organisation: official invitation Screening has ethical issues: is the negative stress affects worth only a few benefits true +ve, false +ve, false –ve, true –ve – corrected loss of confidence in HCP Depression screen: felt low in last two weeks? Anhedonia? Questionnaire e.g. HADs, Becks Alcohol misuse: harmful (risk of mental or physical harm), hazardous (causing mental or physical harm), dependence (difficulty controlling, given higher priority, causes harm to self and others, increase tolerance) Cut down Annoyed by others suggesting Guilty Eye opener 5As: Ask, Advise, Assess, Assist, Arrange 5Rs: Relevance, Risks, Rewards, Roadblocks, Review Assess motivation (do you want to quit, will you try soon, do you want help) if motivated the level of dependence will predict success (smoke within 30 mins of waking and +15 a day = highly dependant) Session Five: Councelling Depressive symp: affect (low mood, anhedonia), behaviour (appetite, sleep), cognitive (suicide ideation) Increase prevalence in people with chronic conditions (cause/ effect in diabetes) and elderly Diagnostic interview is the best way to screen. Barriers = language, explanatory models, clinician factors and variation in clinical presentation. Have you felt down, depressed, or hopeless? Anhedonia? Yes? HADS, BDI, PHQ-9 Stepped care plan – brief intervention, medication, psychological help hospitalisation CBT: challenge irrational thoughts to change behaviour Psychodynamic: current difficulties have roots in childhood Humanistic: consider positivism and wholeness Systems: social relationships play an important role – family counselling is useful Session Six: Consultation Purpose of consultation – create interpersonal relationship, exchange information, agree treatment plan Relies on social relationship (manners, polite, laughing), therapeutic relationship (respect and genuniness) and patient-centred communication (allowing patient to express ICE) Shared consultation depends on age (older prefer paternalistic), SES (higher prefer shared) and condition Negative consultation: jollying patients along, jargon, depersonalisation, not paying attention to psych, interrupting, explaining away distress as normal Poor communication: less likely to use services, adhere to treatment and more likely to have –ve health Doctor blocking: time, fear of increasing distress, threat to own emotional wellbeing Patient blocking: burden, doctor blocking, embarrassed, feel not appropriate, fear confirmation of worries Good communication increased satisfaction, better recall and adherence etc. Session Seven: Addiction Addict (no control over behaviour), addiction (chronic relapsing brain disease), dependency (physical or psychological) affect (emotional instability), behaviour (increased use) and cognitive (self-centred) 3+ of increased tolerance, craving, prioritising, difficulty controlling, increase effort to source, neglect etc. Drugs act on mesolimbic reward system via dopamine Stepped care approach: advise – planned counselling – counselling + medication – inpatient Relapse risk factors: age, duration, lack of social support, no follow-ups, no coping etc. Motivation: intrapersonal, interpersonal, contextual and motivational interviewing Treatment: abstinence, harm reduction, medication and psychological. Session Eight: Stress Effects: affect (anxiety, depression, frustration), behaviour (alcohol, smoking), cognition (poor memory, concentration), physiological (immune dysfunction, neuroendocrine effects) Stressed inpatients: increased time in, slow wound healing, more staff time, more analgesia etc. GAS: alarm (fight or flight), resistance, exhaustion Chronic stress ulcers, hypertension, impotence, asthma, acne, psrosis etc. SRRS: 43 life events ranked on chronicity, magnitude and inclusivity Transactional model of stress: stressor primary appraisal (is it a threat?) 2ndry appraisal (can I cope?) coping outcome Factors influencing appraisal: background, stable, situational, social Coping: activities, strategies, dimension (problem focused or emotion focused) Stress management: relaxation – visual, muscle relatxtion, self-hypnosis Session Nine: Somatisation Common symptoms: pain, GI, sexual or pseudonerological Briquets: lots of somatic sympt before 30, 4 areas of pain, 1 GI, 1 sexual and 1 pseudoneurological Conversion: affects motor or sensory nerve control: pseudoneuro – convulsion, paralysis, paraesthesia Hypocondriasis: preoccupation with medical sympt despite reassurance Somatoform pain: serious pain interfering with function – works well with group therapy Body dysmorphia: preoccupation with body defect with increasing distress and suicide ideation Causes: biopsychosocial commonly traumatic event, anxiety depression etc. Assessment: identify beliefs, any stressors, coping and screen for psychiatric morbidity Treat: validate feelings, discuss worries, treatment plan, follow ups, 2 HCP involved, coping strategies etc. Are symptoms extreme and chronic? Coping – do they effect ADL? Belief – resistance to reassurance. Sick role accepted? Excessive use of sevice?