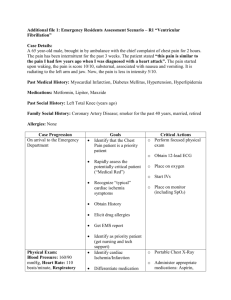
ADULT RESUS final 10-1-14
advertisement

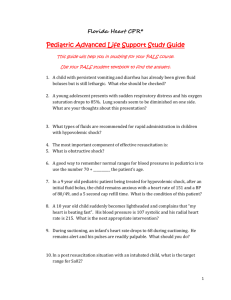
Oct 1, 2014 Revision ADULT CARDIAC ARREST Specific information needed A. History of arrest – onset, preceding symptoms, bystander CPR, or other treatment; duration of arrest. B. Past history – disease, medications. C. Surroundings – evidence of drug ingestion, trauma, environmental exposure, and other unusual presentations. Specific objective findings A. Absence of consciousness. B. Terminal or no respirations. C. Absence of pulse. D. Signs of trauma, blood loss. E. Air temperature, skin temperature. Treatment – per American Heart Association Guidelines unless otherwise noted A. Check surroundings for safety to rescuers. B. Transfer to a firm surface. C. Initiate CPR. General Guidelines: Chest Compressions 1. 1 cycle of CPR = 30:2 chest compressions: breaths 2. 5 cycles CPR = 2 minutes chest compressions 3. Push hard and push fast (at least 100/minute) 4. Ensure full chest recoil 5. Rotate compressors every 2 minutes with rhythm checks 6. During CPR, any interruption in chest compressions deprives heart and brain of necessary blood flow and lessens chance of successful defibrillation 7. In general, patients with cardiac arrest initially have adequately oxygenated blood, but are in circulatory arrest. Therefore, chest compressions are initially more important than ventilation to provide perfusion to coronary arteries. 8. Continue CPR while defibrillator is charging, and resume CPR immediately after all shocks. Do not check pulses except at the end of CPR cycle and if rhythm is organized at rhythm check. 9. In the establishment of an advanced airway do not interrupt compressions. Consider alternate oxygenation strategy first. Replace with endotracheal tube only if needed. General Guidelines: Ventilations during CPR 1. If cardiac arrest is suspected to be secondary to VT/VF, passive oxygenation with an OPA and NPA with a NRB facemask is preferred over positive pressure ventilation with a BVM or advanced airway during the initial resuscitation efforts. 2. If cardiopulmonary arrest is suspected to be secondary to a respiratory arrest first leading to secondary cardiac arrest (e.g. severe COPD exacerbation, status asthmaticus, etc.), adequate ventilation and oxygenation are the priority. Good clinical judgment is required while attempting to understand the cause of the cardiopulmonary arrest. 3. In general, in the acute phase of cardiac arrest, patients will have adequately oxygenated blood but are in circulatory arrest. As such, chest compressions are more important than ventilation to perfuse vital organs. D. Call for back-up if needed. E. In unwitnessed cardiac arrest, give first 2 minutes of CPR without interruptions for ventilation. During this time period, passive high flow oxygenation is preferred with OPA/NPA (consider both) and NRB facemask. F. If arrest is witnessed by EMS, immediate defibrillation is first priority General Guidelines: Defibrillation 1. All shocks should be given as single maximum energy shocks 2. Manual biphasic: follow device-specific recommendations for defibrillation. If uncertain, give maximum energy (e.g. 200J) 3. Manual monophasic: 360J 4. AED: device specific 5. Do not interrupt chest compressions and do not hyperventilate. Hyperventilation decreases effectiveness of CPR and worsens outcome G. Treat with medications, pacing, etc. according to rhythm – Using current AHA Guidelines. H. Airway management General Guidelines: Ventilation 1. PASSIVE ventilation is the recommended method for ventilating a patient during resuscitation. “Passive ventilation” is defined by high flow 02 via NRB mask with at least one airway adjunct (NPA/OPA). 2. For purposes of ventilation, adult age is defined as patients 13 years of age and greater. (This age cutoff is based on the Colorado State Adult RSI guidelines.) However, provider discretion can be exercised based on patient habitus. General Guidelines: Timing of Placement of Advanced Airway 1. Advanced airway (e.g. ETT) is not required during resuscitation. There is a strong preference to NOT place an advanced airway until ROSC. However, advanced airway may be placed at any time after initial 2 rounds of chest compressions and rhythm analysis, provided placement does not interrupt chest compressions. a. If there is a failure to secure the airway using the ETT, or there are concerns about interrupting CPR to secure the airway, a rescue airway may be considered. 2. If there is active airway compromise (e.g. vomiting), an advanced airway can be placed at any time during resuscitation, with attention to not interrupting chest compressions. 3. Advanced airway should be obtained upon ROSC 4. Once an advanced airway is in place, compressions are given continuously and breaths given asynchronously at 8-10 per minute. a. It is vital that patients are NOT over-ventilated with advanced airway, as this can cause decrease in cardiac preload. 5. Always confirm advanced airway placement with ETCO2 6. Use continuous waveform capnography. In low flow states such as cardiac arrest, colorimetric CO2 detector may be inaccurate and not sense very low CO2 level. Specific precautions A. Cardiac arrest in a trauma situation is not treated according to this protocol. In a trauma situation, transport should be rapid, with IV, and CPR en-route. B. Survival from cardiac arrest is related to the time to BOTH BLS and ALS treatment. Don't forget CPR in the rush for advanced equipment. A call for back-up should be initiated promptly by any BLS unit. Likewise, standing order administration of the first steps in treatment is recommended to minimize time delays to ALS. C. See Neonatal and Infant/Child Resuscitation Protocols for special pediatric details. D. Large peripheral veins (antecubital or external jugular) are preferred IV sites in an arrest or an IO. E. Quick-look pads or paddles are preferred for initial rhythm check. Change to leads for more secure reading. Be sure machine is set to record from whichever mode is in use. F. Patients who have called with chest pain and decompensate rapidly may benefit from rapid attempts at pacing. General Guidelines: Pacing 1. Pacing is not indicated for prolonged asystole and PEA. Instead start chest compressions according to Universal Pulseless Arrest Algorithm. 2. Pacing should not be undertaken if it follows unsuccessful defibrillation of VT/VF as it will only interfere with CPR and is not effective General Guidelines: ICD/Pacemaker patients 1. If cardiac arrest patient has an implantable cardioverter defibrillator (ICD) or pacemaker: place pacer/defib pads at least 1 inch from device. Biaxillary or anterior posterior pad placement may be used G. Contact base for termination if no Return of Spontaneous Circulation (ROSC)