Reorganization of Questions in eValu8 2014 RFI
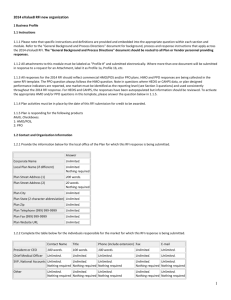
advertisement

Reorganization of Questions in eValu8 2014 RFI-Input and Output Background Plan Sponsors provided feedback over the past few years that the organization of the summary of plan responses to the eValue8 RFI could be improved to more closely align with how they thought about plan activities. A reorganized format proposed by a Plan Sponsor was discussed with Coalition leaders who supported this change. Sample reports were produced and provided to gather feedback from Plan Sponsors and a subset of Plan respondents. The change in organization of the questions was discussed at the September 25th eValue8 annual meeting with the Plan and Coalition attendees (in person and on the phone) to gather feedback on the new organization and timing of implementation of the output (Summary report) and input (RFI) All attendees voted to implement the change in both the RFI and the Summary Report for eValue8 2014. Plan respondents told NBCH that this reorganized format more closely aligned with how they produce reports. What does this mean When respondents receive the email invitation to participate in eValue8 2014, they will access Proposal Tech to begin the response process. One key difference is the RFI will now consist of 8 Modules instead of 7 modules. Many of the Module and section titles will be different; however the questions are not different, although they may be relocated. Please review the module and section information below as well as the summary of changes. Resources to support this change As in previous releases of eValue8, a mapping document will be provided that will map the question number in eValue8 2014 to eValue8 2013 and eValue8 2012. The “default source” feature in ProposalTech will also be available so respondent can see scored response to the question from prior year and either change their response or confirm the prior response. Current (eValue8 2013 and prior) and New (eValue8 2014) Components Current Organization of Modules/Sections/Questions Plan Profile Contact & Organization Information Enrollment & Scope of RFI Response Services & Compliance Review Provider Management Purchaser Support Health Information Technology Racial, Cultural & Language Competency Innovations Consumer Engagement Alignment of Plan Design Practitioner Information & Connectivity Hospital Choice Support Shared Decision Making & Treatment Option Support Electronic Personal Health Record Claims Management & Price Transparency Performance Measurement New Organization of Modules/Sections/Questions Business Profile Contact & Organization Information Market Position Accreditation & CAHPS Performance Business Practices & Results Collaborative Practices Innovations Other Information Physician & Hospital Management & Measurement Management & Contracting Physician Support & HIT Information to Physicians to Help Steer Members Physician Management and Support to Help Members Stay Healthy Physician Management and Support to Help Members Manage Chronic Conditions Scope of Physician Measurement for Transparency and Rewards Physician Payment Programs for Value Achievement (Quality and/or Efficiency) Plan Policies on Healthcare Acquired Conditions and Never Events Hospital Payment Programs for Value Achievement Plan Steerage of Members to Centers of Excellence and Higher Value Physicians and Hospitals Hospital Management Performance Provider Measurement Community Collaboration for Provider Measurement Physician Support & HIT Physician Performance Measurement & Reporting Physician/Practice Site and Medical Group/IPA Value Differentiation and Payment Rewards Hospital Services Performance Measurement and Reporting Efficiency and Overuse Hospital Value Differentiation and Payment Rewards Centers of Excellence or High Performance Hospital Network Pharmaceutical Management Program Organization Efficiency & Appropriateness: Generic & Appropriate Drug Use Specialty Pharmaceuticals Quality and Safety: Outpatient Prescribing Prevention & Health Promotion Health Promotion Programs and Worksite Wellness Health Assessments (HA) Cancer Screening Programs & Results Immunization Programs Prevention & Treatment of Tobacco Use Obesity Obstetrics and Maternity and Child Chronic Disease Management Program Scope & Coordination Member Identification & Support Practitioner Support Performance Measurement: CAD Performance Measurement: Diabetes Performance Measurement: Other Conditions Behavioral Health Management Plan Organization Member Screening & Support Practitioner Support Performance Measurement Helping Members Stay Healthy Alignment of Plan Design Health Assessments (HA) Cancer Screening Programs & Results Immunization Programs Health Promotion Programs and Worksite Wellness Prevention & Treatment of Tobacco Use Obesity CAHPS Performance Helping Members Become Good Consumers Addressing language and health literacy needs Alignment of Benefit Design and Incentives Electronic Personal Health Record Help Finding the Right Doctor Hospital Choice Support Shared Decision Making & Treatment Option Support Price Transparency - Helping Members Pay the Right Cost HEDIS & CAHPS Performance Helping Members Manage Acute/Episodic Conditions Alignment of Plan Design Obstetrics and Maternity and Child Bariatric Surgery End of Life and Hospice Care Helping Members Manage Chronic Conditions Program Availability (Standard or Buy-Up, Stand) and Co-ordination Member Identification & Support for CAD & Diabetes Performance Measurement: CAD & Diabetes Plan Organization for Behavioral Health Management Member Screening & Support in Behavioral Health Performance Measurement: Behavioral Health Performance Measurement: Other Conditions Pharmaceutical Management Value-Based Formulary Efficiency & Appropriateness: Generic & Appropriate Drug Use Specialty Pharmaceuticals Quality and Safety: Outpatient Prescribing Client Support, Data Analyses and Reporting Beneficiary Communication and Benefit Design Data Analyses and Reporting New Purchaser Report and Plan RFI – “Summary of Changes” What Moved In Module What Moved out CAHPS Rating of Health Plan & Health Care from Consumer Community Collaboration from Provider Prometheus PACs from Provider Business Profile Hospital Accreditation & Treatment of Claims if no contract with Specialist Meaningful Use and eRxing All but 2 questions in Cultural Disparities to “Good Consumer” Beneficiary communication and outreach support and Purchaser Reports to Client Support Hospital Accreditation & Treatment of Claims if no contract with Specialist from Profile Meaningful Use and eRxing from Profile Support and services-treatment decision support, Choosing Wisely from Consumer Monitor screening for tobacco use from Prevention Practitioner Education Support (tobacco, obesity, PCMH, diabetes, CAD, depression and alcohol) including reimbursement for SBIRT Monitoring use of screening tools for alcohol and depression and appropriate prescribing of anti-depressants Engaging ERs and trauma centers on alcohol screening and interventions Benefit Design for Wellness & Prevention from Consumer CAHPS rating for member communication from Consumer All but 2 questions in Cultural Disparities from Profile Public reports of physician and hospital quality from Provider HEDIS Overuse Procedures from Provider Physician & Hospital Management & Measurement Community Collaboration to Business Profile Prometheus PACs from Provider to Business Profile Helping Members Stay Healthy Bariatric surgery to “Episodic care” Maternity & Obstetrics to “Episodic care” Alignment of Incentives through plan design to Client Support Benefit Design for Wellness & Prevention to “Stay Healthy Benefit design for acute care to” Episodic care” and for Chronic Disease to “Chronic Conditions” End of Life Care Program and Hospice Services to “Episodic care” Benefit Design for Acute Care from Consumer End of Life Care Program from Consumer Hospice Services from Consumer Bariatric surgery from Prevention & Wellness Maternity & Obstetrics from Prevention & Wellness (includes payment reform t o reduce elective deliveries) Benefit design for Chronic Disease from Consumer Entire BH module except to Provider Support Helping Members Manage Acute/Episodic Conditions None Helping Members Manage Chronic Conditions None Beneficiary communication and outreach support from Profile Purchaser Reports from Profile Alignment of Incentives through plan design from Consumer Pharmaceutical Management Client Support, Data Analyses & Reporting Provider Support for CAD and Diabetes to Physician & Hospital Non-HEDIS measures for CAD, Diabetes and Depression DM programs (ROI, Absenteeism) to Client Support None None Helping Members Become Good Consumers