Care Plan: Abdominal Pain, Nausea
advertisement

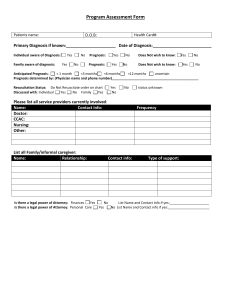
CRITICAL THINKING SUMMARY Student: Kathryn Kaufman Client Dx: Jejunal Stricture, Diverticulitis, Pericarditis, HTN, GERD, Asthma, Gout, DVT with hemorrhagic CVA. Age: 67 Allergies: Celebrex, Lisinopril, Norvasc, Robaxin The MEDICAL DIAGNOSIS that brought the client to the hospital is: Abdominal pain, nausea, and weight loss of 20 lbs. in the last month PATHOPHYSIOLOGY of diagnosed disease: (From text) GOUT: “Hyperuricemia (serum concentration greater than 7 mg/dL) can but does not always cause monosodium urate crystal deposition. However, as uric acid levels increase, the risk becomes greater. Attacks of gout appear to be related to sudden increases or decreases of serum uric acid levels. When the urate crystals precipitate within a joint, an inflammatory response occurs, and an attack of gout begins. With repeated attacks, accumulations of sodium urate crystals…are deposited in peripheral areas of the body, such as the great toe, the hands, and the ear. Renal urate lithiasis (kidney stones), wth chronic renal disearse secondary to urate deposition, may develop.” SYMPTOMS typically seen with this diagnosis include (as identified in your text): Manifestations of the gout syndrome include acute gouty arthritis (recurrent attacks of severe articular and periarticular inflammation), tophi (crystalline deposits accumulating in articular tissue, osseous tissue, soft tissue, and cartilage), gouty nephropathy (renal impairment), and uric acid urinary calculi. CLIENT’S SYMPTOMS of the diagnosed disease include: Patient noted some pain in her joints when she was up and moving, and had some stiffness when walking around with assistance. NUTRITIONAL ASSESSMENT: Height (actual or estimated): 167.6 cm Weight (actual or estimated): 92.0 kg Estimate Ideal Body Weight (Male: 105lb + 6 lb/inch > 5’. Female: 100lb + 5lb/inch > 5’): 130 lbs. Does this client have characteristics of a well-nourished person? Yes/No Explain your answer. The patient appeared to be physically unwell from general appearance. Her skin looked pale and sunken at her eyes; her hair was dull-looking; her energy level was depleted, although she did ambulate in the halls with standby assist, which indicated that her muscle strength was good. She was obese, with her BMI at 33; she mentioned that she had had a weight loss of about 20 lbs. during the last month. Since this patient was admitted to the hospital on 01/29, she had not had much of an appetite. She had little to no appetite due to her abdominal pain, and was nauseated after eating. She was placed on total parenteral nutrition (TPN) at 55 ml/hr, and tolerated it. When an exploratory laparotomy was done to further understand patient’s condition, duodenal and jejunal ulcers were found, as well as jejunal stricture. Patient had a small bowel resection to resolve these issues, but no changes in patient’s appetite occurred, and abdominal pain remained. This resulted in a continued lack of appetite from the patient, and generalized weakness from insufficient caloric intake. PSYCHOSOCIAL STAGE OF DEVELOPMENT What is the client’s developmental stage? Ego integrity vs. Despair Has he/she met the necessary accomplishments? Yes/No Explain. The patient seemed to be anxious about her hospital stay, but when the student asked her about her life and family, she responded in a way that intimated a sense of pride in her family and who she was as a person. She was cooperative, and eager to know what was going on with her health. She seemed frustrated and uncertain because her health was not improving. The student entered the room once to find her crying with her husband. She sounded eager to be home and in a familiar place after being in the hospital for almost three weeks, but also slightly depressed that she was not getting much better. How is this illness affecting the client’s ability to meet these necessary accomplishments? The patient’s frustration with her health kept her focus mainly on what was going on with that, and not as much on her sense of accomplishment in life. She was showing signs of acceptance of her condition, but it was obvious she did not like it. She was showing signs of depression because the cause of her illness was still unknown (or at least the solution) after so much time. NURSING DIAGNOSIS/OBJECTIVES/INTERVENTIONS Indicate below the 2 priority nursing diagnoses that are most relevant for your client. #1 NURSING DIAGNOSIS (problem r/t) Imbalanced nutrition, less than body requirements r/t lack of appetite. DEFINING CHARACTERISTICS (S/S) that support this diagnosis: Patient is not able to keep food down or eat without nausea; patient’s appetite is decreased, and has been on TPN for calorie intake. OBJECTIVE/CLIENT OUTCOME for this diagnosis: Patient will be able to eat at least 50 percent of meals within 1 week, and be free of signs of malnutrition. NURSING INTERVENTIONS that will assist the client to resolve the above identified diagnosis: 1. Weigh the patient daily in acute care, weekly in extended care at the same time (usually before breakfast), and with the same amount of clothing (Ladwig & Ackley, 2011, p. 526). 2. For the client who is malnourished and can eat, offer small quantities of energy-dense and protein-enriched food, served in an appetizing fashion, at frequent intervals (Ladwig & Ackley, 2011, p. 527). 3. Provide companionship at mealtime to encourage nutritional intake (Ladwig & Ackley, 2011, p. 527). #2 NURSING DIAGNOSIS (problem r/t) Readiness for enhanced coping r/t patient crying from frustration about hospital stay. DEFINING CHARACTERISTICS (S/S) that support this diagnosis: Patient was found crying with spouse because of frustration over having no appetite and being in the hospital for almost three weeks. Patient is frustrated because the she has not been seeing any positive outcomes of her hospital stay in regards to her perceived health. OBJECTIVE/CLIENT OUTCOME for this diagnosis: Patient will state awareness of at least three possible environmental changes that may contribute to decreased coping, and seek at least one new coping strategy within two weeks from now. NURSING INTERVENTIONS that will assist the client to resolve the above identified diagnosis: 1. Encourage the patient to use spiritual coping mechanisms (if applicable) such as faith and prayer (Ladwig & Ackley, 2011, p. 306). 2. Empower the patient to set realistic goals and to engage in problem solving (Ladwig & Ackley, 2011, p. 306). 3. Use empathetic communication and encourage the patient to verbalize fears, express emotions, and set goals (Ladwig & Ackley, 2011, p. 306). COMPLICATIONS: If this client’s condition were to worsen, what would be the most likely reason and why? Most likely, this patient’s condition would worsen because of further malnutrition due to abdominal pain, lack of appetite, and nausea after eating. Her condition could also worsen because of the amount of anxiety she feels about not knowing what is wrong with her, and that she is not seeing any positive results. This could take away some of her appetite, however it will make it harder for her to keep eating. How would you know this is happening? This could most easily be noted as happening when the patient’s food intake is decreasing and her level of anxiety is increasing. She would become weaker, and probably would not be able to keep down very much of the food she actually is consuming. What will you do if this happens? This patient has an order (though it has not yet been filled) for a nasogastric tube to be placed. If she continued to have the same issues with eating and appetite, it is likely that the doctor would want the NG tube to be placed, and have her begin enteral feedings as she tolerates them. The student/nurse would provide as much encouragement to the patient as possible to reassure her, and would try to reduce her anxiety levels as much as possible, while still making sure she knows the seriousness of the situation PHYSICIAN PRESCRIBED MEDICATIONS AND INTERVENTIONS MEDS/IVs/TX/DIET (Include dose, route, frequency) REASON PRESCRIBED (Drug Classification, What is it treating?) NURSING IMPLICATIONS FROM TEXT (Checking for adverse reactions, preparation & administration concerns) TPN 2,000 infusing @ 55ml/hr in Dextrose 5% in Water Allopurinol 300mg/1 tab, by mouth, daily Potential injury during central line placement, sepsis, and metabolic complications. Limits amount of caloric intake via TPN to about 2300cal/day. Not recommended for full nutritional needs. I&O should be monitored (Davis’ Drug Guide, 2014). Xanthine oxidase inhibitors: prescribed for treatment of gout. Rash, hypersensitivity, hypo-/hypertension, drowsiness, nausea, diarrhea, vomiting, bone marrow depression. Monitor I&O; may affect kidney function. Monitor for joint pain and swelling in patients with gout. Watch for skin rash (Davis’ Drug Guide, 2014). Anticoalgulants: prescribed for post-surgery measures. Alopecia, bleeding, anemia, heparininduced thrombocytopenia, pain at injection site, fever. Assess for signs of bleeding and hemorrhage, bruising, etc. Monitor for hypersensitivity reactions (Davis’ Drug Guide, 2014). Vasodilators: prescribed for high blood pressure. Dizziness, drowsiness, headache, tachycardia, sodium retention. Make sure to check blood pressure and heart rate immediately before giving (should be above 60 bpm). Monitor throughout therapy (Davis’ Drug Guide, 2014). Hormones: given for hormone replacement of thyroid hormones. Headache, irritability, abdominal cramps, diarrhea, vomiting, hyperthyroidism, weight loss. Assess apical pulse and BP before giving, assess for tachyarrhythmias and chest pain (Davis’ Drug Guide, 2014). Antiulcer agents: prescribed for duodenal and jejunal ulcers. Abdominal pain, diarrhea, nausea, vomiting, constipation, flatulence. Assess patient routinely for epigastric and abdominal pain and for frank and occult blood in stool, emesis, or Hydralazine 50mg/2 tabs, by mouth, twice daily Misoprostol 100 mcg/1 tab, by mouth, 3 times (What data is important to know before & after giving) To provide caloric and nutritional supplication to the diet for a patient who needs additional support. Heparin 5,000 units/1mL, subQ, every 8 hours Levothyroxine (Synthroid) 100 mcg/1 tab, by mouth, daily CLIENT DATA FROM YOUR ASSESSMENT gastric aspirate (Davis’ Drug Guide, 2014). daily with meals Pantoprazole 40mg/1 tab, by mouth, twice daily Propranolol 160 mg/1 cap, by mouth, daily Sodium chloride 0.9% 10 ml IVPush, every 8 hours at end of shift. (Norco/Vicoden) Acetaminophen hydrocodone, 2 tab, as needed every 4 hours (Zofran) Proton pump inhibitors: prescribed for treatment of GERD and duodenal ulcers. Headache, pseudomembranous colitis, abdominal pain, hyperglycemia, bone fracture. Assess patient routinely for epigastric and abdominal pain and for frank and occult blood in stool, emesis, or gastric aspirate (Davis’ Drug Guide, 2014). Beta-blockers: prescribed for prevention MI and management of HTN. Fatigue, weakness, dizziness, arrhythmias, bradycardia, pulmonary edema, mental depression. Assess BP and HR frequently during therapy, assess for orthostatic HTN; monitor I&O, take daily weight. Assess for rash frequently (Davis’ Drug Guide, 2014). Mineral/electrolyte replacements/supplements: prescribed for replacement of electrolytes; patient has low sodium. Heart failure, pulmonary edema, edema. Assess fluid balance (I&O, weight, edema, lungs); assess for signs of hyponatremia/hypernatremia (Davis’ Drug Guide, 2014). Opioid analgesics: prescribed as needed for abdominal pain. Confusion, dizziness, sedation, hypotension, constipation, dyspepsia, nausea. Assess BP, pulse, and respirations throughout therapy. If resp. are <10/min, may need to decrease dose to avoid hypoventilation. Assess bowel function (Davis’ Drug Guide, 2014). Antiemetics: prescribed as needed for patient nausea. Headache, dizziness, drowsiness, constipation, diarrhea. Assess patient for nausea, vomiting, abdominal distention, and bowel sounds prior to and after giving. Assess for extrapyramidal effects (Davis’ Drug Guide, 2014). Antiemetics: prescribed as needed for patient nausea. Neuroleptic malignant syndrome, confusion, disorientation, sedation, bradycardia. Monitor BP, pulse, and respirations frequently during therapy. Assess level of sedation (may cause resp. depression) (Davis’ Drug Guide, 2014). Ondansetron 4mg/2ml IVPush, as needed every 6 hours (Phenergen) Promethazine 6.25 mg /0.25mL, IVPush, as needed every 6 hours Analgesics: prescribed as needed for patient pain. Tramadol 50 mg/1 tab, by mouth, as needed every 4 hours Seizures, dizziness, headache, constipation, nausea, abdominal pain, anorexia, diarrhea. Assess pain before giving; assess BP, pulse, and respirations before/during therapy; not recommended for patients dependent on opioids; monitor patient for seizures (Davis’ Drug Guide, 2014). Analysis of Diagnostic Tests DIRECTIONS: 1. List all diagnostic and laboratory tests pertinent to the patient's medical diagnosis or medical treatments (i.e. medications) and provide the patient values for each test. Explain why they are pertinent for this patient. 2. List any screening diagnostic and laboratory tests that are not within normal limits. Explain why these tests are increased or decreased in relation to your patient's medical condition. Diagnostic/Lab Test Sodium Urea Nitrogen Glucose Patient Values Analysis of Values 133 (L) The patient’s Na+ levels could be low because she has been vomiting some after eating. Hydralazine can also cause fluctuation in electrolytes. 27 (H) A high BUN can be caused by her allopurinol; these higher levels will be seen to decrease after 2-3 days. May also be increased from propranolol. 104 (H) Could be elevated because the patient is receiving a TPN in D5W drip. Propranolol can also increase glucose levels. Patient has not been Calcium 8.0 (L) Total protein Albumin 4.7 (L) 1.8 (L) Surgery: Exploratory laparotomy Surgery: Small bowel resection consuming a large amount of calcium in her diet – has not really been consuming much of anything. This could contribute to it being low. The patient’s level of protein could be decreased because she has not been consuming very much protein (and keeping it down). Pantoprazole can cause some abnormality in liver function tests. Found: a duodenal and jejunal ulcer. Patient is receiving pharmacological treatment for ulcers. Patient has had a small bowel resection, and has been healing nicely, though she has not been improving in appetite or much with pain levels. References: Davis’ Drug Guide. (2014). Nursing Central. Unbound Medicine. Retrieved from www.nursing.unboundmedicine.com. Ladwig, G. B. & Ackley, B.J. (2011). Guide to nursing diagnosis (3rd ed.). Maryland Heights, MO: Mosby. Smeltzer, S., Bare, B., Hinkle, J., & Cheever, K. (2010). Brunner & Suddarth’s textbook of medical-surgical nursing (12th ed.). Philadelphia, PA: Lippincott.
![[Physician Letterhead] [Select Today`s Date] . [Name of Health](http://s3.studylib.net/store/data/006995683_1-fc7d457c4956a00b3a5595efa89b67b0-300x300.png)