Initial Consultation Form
advertisement
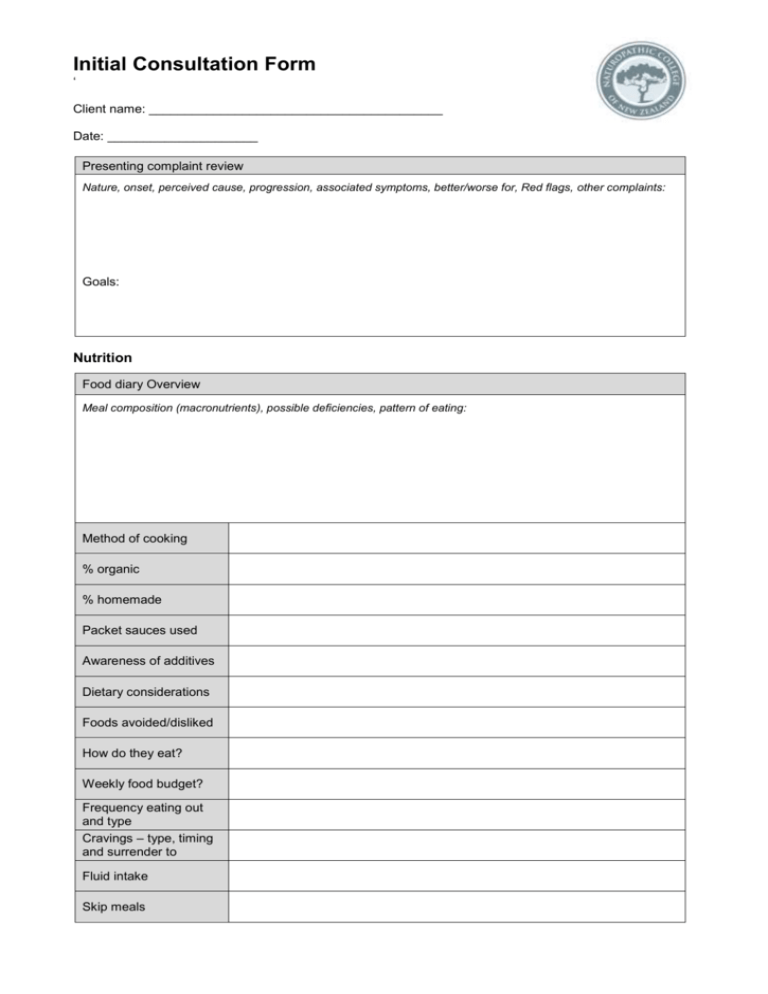
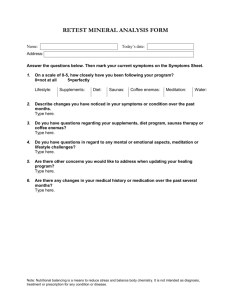
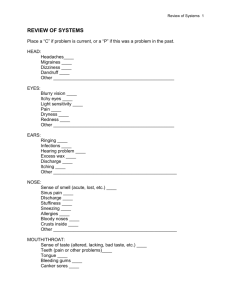
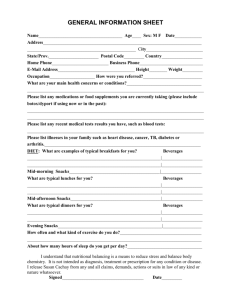
Initial Consultation Form ‘ Client name: _________________________________________ Date: _____________________ Presenting complaint review Nature, onset, perceived cause, progression, associated symptoms, better/worse for, Red flags, other complaints: Goals: Nutrition Food diary Overview Meal composition (macronutrients), possible deficiencies, pattern of eating: Method of cooking % organic % homemade Packet sauces used Awareness of additives Dietary considerations Foods avoided/disliked How do they eat? Weekly food budget? Frequency eating out and type Cravings – type, timing and surrender to Fluid intake Skip meals Body Systems Digestive – appetite, reflux/burning/gnawing after meals, discomfort after eating, bloating, urgency, cramping, wind, sleepy after meals, blood with stool – bright/dark, pain (location/type) , nausea Integumentary - eczema ( hot, dry, red, inflamed, location, raw, itchy), psoriasis (scaly, red, inflamed, location) , acne (location, white pustules, red/deep, cyclic) scars, boils, flushing, sweats, cracks, itching, bleeding gums, cracked lips, sunburn, dry/oily Respiratory – difficulty breathing/asthma/constriction, chest pain, sputum (colour), shortness of breath, wheezing, cough Urinary – Bladder infections (burning/ blood with urination), flow of urine, complete urination, pain, kidney infections (lower back pain/blood in urine), fluid retention (location), incontinence Cardiovascular – anaemia (easy bruising, pale, breathless, fatigue, frequent infections), varicose veins (pain), high or low blood pressure, palpitations, chest pain, cholesterol, cold extremities, bleeding/ hemorrhages (nose bleeds), broken capillaries, burst blood vessels Musculoskeletal – cramps, restless legs, growing pain, areas of tension, repetitive strains, arthritis, injuries, pain, stiffness, tendonitis, bursitis, twitches, dental health/history Lymphatic / Immune – previous illnesses, glandular fever (severity), flu vaccine, freq of colds / flu per year, heal quickly, hay fever / sinus (blocked nose, itchy eyes, tickly throat, pain in sinus, runny), cold sores, swollen glands (location, hard/soft, moveable, pain) , frequent infections Reproductive – Women – Sexual function, STDs, # of pregnancies, difficulty getting pregnant, last menstrual cycle, length of cycle, frequency of cycle, colour, flow, duration, clots, cramping/pain, PMS (irritability, sore breasts, sore back, cravings), noted changes in cycle with age, noted discharge, itching, odour, thrush Men – sexual function, STDs, impotence, discharge, pain, blood, low testosterone (loss of muscle, low energy, low libido, decreased strength) Nervous – insomnia, restlessness, irritability, depression, anxiety, teeth grinding, ability to tolerate stress, mouth ulcers, vision, hearing, smell, taste Endocrine – hypothyroid (cold hands/feet, dry/itchy skin, dry/thin hair, constipation, brittle nails, poor concentration, fatique) hyperthyroid (fast beating heart, bulging eyes, loose bowel motions, fatigue, anxiety), blood sugar dysfunction (intense hunger, nervousness/confusion, trembling, palpitations, anxiety/irritability, poor concentration, dry mouth, thirst, frequent urination, irritable without food, blurry vision, dry/itchy skin, poor eyesight, yeast infections, numb tingling feet) hypoadrenia – (tired upon waking, insomnia, excessive fatigue, craving salt, overwhelmed, poor concentration, low immunity, depression) Emotional tendencies – cope well on a daily basis, thriving/growing, satisfied with life, happy, supported, feel able to change things if not Client Consent I, __________________________________, give consent for my health information to be documented and appropriate physical examinations and assessments to be performed. I understand that following the consultation a treatment plan will be created for me after agreement between myself and the student practitioner. I will give the practitioner all personal information needed to perform a safe and successful treatment. I am aware that both practitioner and I have the right to stop the consultation procedure and / or treatment at any time. Client Signature: ________________________________________________________________ Student Practitioner Signature: ____________________________________________________ Clinical Assessments Blood Pressure - Sitting - Standing Respiratory Rate Zinc Taste 1 2 3 4 Height Pulse Weight Temperature BMI Blood Type Key Note Endocrine body type Body Language Facial Signs Nail Signs Colours, lines, marking, scars, sunken, age spots Pitting, ridging, white spots, lines, marks, colour, capillary refill, cuticles, growth, strength Tongue Colour Size/Shape Coating Tremor Markings Iridology/Sclerology Other Physical Assessments Lymph, Thyroid, Abdominal, Melanoma, Phalens, skin scratch, PPRT Evaluation Summary Possible causes for complaint Treatment Focus Overall approach of treatment Treatment Plan Specific and individualized treatment Hb/ Flower essence/ Supplements recommended: Nutrition advice: Lifestyle Advice: Handouts Given: Referral to: Self Reflection Client take-home shopping list Shopping list: Nutritional aspects to integrate: Lifestyle techniques to look into: Prescriptive remedy instructions: Please feel free to call me and discuss anything that may occur to do with your presenting complaint. I will have your thorough treatment plan ready in a day or two and will call you to discuss.