Neurosciences Emergency Admissions and Bed Management
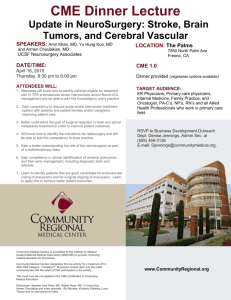
advertisement

Neurosciences Emergency Admissions and Bed Management Neurosciences The Atkinson Morley Neuroscience Centre provides tertiary neuroscience care to a regional population of 3.5 million in South West London, Surrey and Sussex and some district neurology and neurosurgery services to the local population. The Neurology service includes a Regional Head Injury Service and Hyper Acute Stroke Unit providing specialist stroke services to the population of South West London. There are approximately 7000 admissions to Neurosurgery and Neurology annually with Neurosurgery carrying out between and 2400 – 2500 operations of which 60% are emergencies. Neurosurgery also runs one of the busiest neuro-oncology services in the country and manages approximately 1300 patients a year with brain and other central nervous system tumours. These patients form a large part of our elective admissions. Stroke at St Georges is one of the leading stroke services in the UK. There is a twenty bedded HASU to provide service to patients from South West London, and also a sixteen bedded Stroke Unit providing services for local patients. This service has approximately 2000 admissions per year. St George’s also acts as a regional and national referral for specialised stroke cases. We have a well developed carotid intervention service offering endarterectomy and stenting in collaboration with the regional vascular surgery unit also housed at St George’s and receive referrals from throughout the district for this. Neurosciences bed configuration; Ward Location Kent Number of beds Third Floor 8 Head Injury William Drummond Third Floor 22 Neurology (incl 4 dedictate Video Telemetry beds with IT/camera wiring) 20 Hyper Acute Stroke Unit Brodie Neurosurgery Second Floor 14 Neurosurgery (Female) Brodie Stroke Second Floor 16 Stroke Unit McKissock Second Floor 24 Neurosurgery (Male) The bed configurations are based on Service Specifications set by commissioners and the demands experienced by each service. The Neurosciences staff will flex the non-stroke beds after discussion with the clinicians and a review of the tertiary emergency and elective demands. The following emergency conditions have to be admitted to St George’s as a tertiary Neurosciences centre; Neurosurgery/TBI; Cranial extradural haematoma regardless of whether a craniotomy is required Cranial acute subdural haematoma requiring craniotomy Clinically suspected blocked VP shunt Acute hydrocephalus with clinical neurological deterioration of GCS (eg Subarachnoid haemorrhage, colloid cyst, tumours) or with radiological evidence of likely imminent deterioration or coning Acute deterioration in GCS of chronic, or acute onset chronic subdural haematoma, intracerebral haematoma or where there is radiological evidence of likely/ imminent coning Clinically suspected cerebral abscess with consistent contrasted CT or MRI imaging Cerebral tumour with mass effect and acutely deteriorating GCS despite 16 mg iv dexamethasone Painful 3rd nerve palsy with proven posterior communicating /superior cerebellar artery aneurysm on CT /MRI Stroke patients being considered for craniectomy. Acutely deteriorating cord compression from trauma, tumour, infection, haemorrhage, acute disc herniation. Not from central cord syndrome or degenerative changes alone. Patient must have been on strict bed rest and in the case of tumour, acute disc or haemorrhage, also on dexamethasone 16 mg IV loss Proven central lumbar disc herniation with established perineal sensory + incontinence / urinary retention Acute traumatic brain injury on CT brain scans All of these patients can be managed and placed as directed by the Neurosurgical SpR and consultant on call and do not normally require site management intervention unless they are admitted via St George’s A&E This will only happen if Neurosurgery have no beds to admit directly to. Stroke; these must be brought into A&E and placed via the Neurology/Stroke SpR on call All ?Stroke patients who are ambulanced into A&E (from home/community or another Hospital) All patient found to have a medical condition should be referred back to their local DGH and either transported back or placed under the team that would normally care for a patient with that condition The Neurosciences bed manager will ensure elective admissions are reviewed daily and prioritised along with the emergencies awaiting transport to a neurosciences bed. The Neuroscience Management team, in liaison with the DDNG for Neuro/Surgery/Theatres will make a decision on the opening and staffing of the Neuro Day Unit (NDU) – this will also take into consideration the patients due to come into the NDU at 7.30am. Key criteria for placing patient in the NDU; All patients must be of the same sex and fulfil the criteria below: The patient should be mobile and require minimal nursing assistance The patient should be able to be fully dressed in the day time The patient is a neurosciences patient The patient is pre – operative and is due to have surgery the following day The patient is due to be discharged the next day from a neurosurgical or neurology ward Stroke patients should not be accommodated within the escalation area. The Neurosciences bed manager will ensure that there are; 1-2 HASU beds empty at 7.30pm, failing that they will identify 2 patients who can be moved to alternative beds to provide acute stroke beds 1-2 Neurosurgical beds empty at 7.30pm, failing which they will identify 2 patients who can be moved to alternative beds This will be based on the proviso that there are no patients in a neurosciences bed that does not have both a neuro condition and is not under neuro consultant (ie outliers) and following discussion with the Neurosciences on call SpR’s Any further placement of patients should be discussed with the Neurology/Stroke (bleep 7277) and Neurosurgery (bleep 7242) SpR on call who will be able to advise on the tertiary nature of their demand. If the rare event that the clinical priority cannot be agreed by the two Neurosciences SpR’s the two consultants on call will need to be contacted.