presenting confidentiality
advertisement

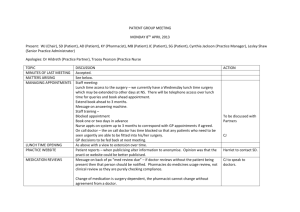
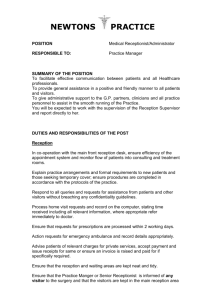
PRESENTING CONFIDENTIALITY This document sets out notes for a presentation on confidentiality for use with a group of GP Practice Staff DO YOU WANT TO KNOW A SECRET? As an introduction play or read the opening lines of the famous Beatles song. "Listen do you want to know a secret; do you promise not to tell" This session is designed to talk about and discuss various aspect of confidentiality as it rel ates to working in a doctors surgery. At the outset let’s do two things demonstrate firstly how easy it is for a message to chang e on its passage from you to a third party and secondly how sensitive is information about you to you. CHINESE WHISPERS Two hooded men one dressed in a Mickey Mouse mask and the other dressed as Fozzie B ear were seen holding what look like long barreled guns rushing into the NatWest Bank i n Pudsey on Monday morning at 10 past 10. 'Hand this message on a piece of paper to the first person in a group say 8 people and ask the first person to pass the message quietly to the next person and so. Once the message has been given to the last person in the group ask the last person to repeat the message o ut loud. Wait for the laughter and the expressions of surprise as to how the message has c hanged Tell the group. This is how easy it is to get things wrong. You are taking confidential mess ages all day every day. Make sure you have taken an accurate message and repeat it back to ensure accuracy. Record the message immediately in a note book or computer log. SENSITIVE INFORMATION This section walks through the type of questions you might be asked at an interview for a job and asks what would you answer and asks whether legally can be asked the question. That aside would you answer the questions differently if you were being asked them by y our doctor, a member of your family, your religious mentor, your solicitor or your best fri end? The questions could be presented on a handout and 10 minutes should be allowed to co mplete the form and discuss it in groups. TWENTY SENSITIVE QUESTIONS Here are 20 'sensitive' questions to test out; 1. What is your name and have you used any other names? 2. How old are you? 3. Where were you born? 4. Are you married, single or divorced? 5. What is your sexual orientation? 6. Which religion do you practise? 7. Do you require time off for religious or other purposes? 8. Do you have any disabilities that might affect your work? 9. Do you take any regular medication? 10. Have you taken any sick leave or maternity leave in the last 5 years? 11. Do you wear glasses? 12. Do you have any difficulty hearing or wear a hearing aid? 13. Do you have any points on your driving licence? 14. Do you have any children aged under 6 years old? 15. Are you intending to have any children? 16. Have you ever been arrested? 17. What languages can you speak and what is your first language? 18. Do you have a passport and what is your nationality? 19. What is your ethnic origin? 20. Do any of your relatives work for this employer? As a general rule any questions that might show a bias against or lack of equality toward t he applicant and show no real relevance to the job or organisation would be inappropriat e. You should not ask for a date of birth or the makeup of your family or its origins at inter view. Once an appointment has been made it will be necessary to confirm age and obtain evidence as to the right to work. These days there may well be raised eyebrows and a reluctance to answer many of the qu estions but equally so candidates often quite willingly reveal answers which might affect t heir chances off being offered the job. There are so many sensitivities that you need to be careful simply about saying boo to a goose! Doctors whether they are general practitioners, consultants or GP Registrars all need to b e aware of their own obligations under the Hippocratic Oath and the Geneva Convention which enshrine their duty to care about their patients, not to do harm and to respect the secrets that patients confide in them even after the patient has died HOW TO BE KEEP IT CONFIDENTIAL A secret is no longer a secret once it is seen or heard by someone else! Looking around a surgery there are many areas where care needs to be taken to maintain confidentiality. Consulting Rooms Example - During a consultation with an AIDs sufferer a nurse entered the room and start ed to talk about another patient. The AIDs patient left the surgery complaining that he h ad no trust that his condition would be kept confidential. The door should be kept closed. Interruptions should be discouraged in person or by telephone. The computer screen should show only the patients notes. The Tannoy system should be switched off. Example - A doctor left open his Tannoy handset and made derogatory remarks about a p atient to someone in the room There is a tendency for doors to remain open between consultations and nursing areas to be shared with other patients as well as doors left open. Reception There should be no telephones at the reception. Computer screens should not be visible Conversations should be private - no queues chomping at the bit! Reception staff should not repeat or reveal the names of any person attending th e surgery to a third party Example - A husband asks the receptionist if his wife has been to see the doctor. The rece ptionist checks and tells him his wife is seeing the doctor. The man rushes down to the co nsulting room and a serious incident occurs. He had assaulted his wife the previous day There is a tendency for conversations to take place in loud voices. Secretarial Office Example - A medical secretary developed a habit of reading intensely every clinical letter that she saw for no apparent reason. She was dismissed. Patients records should be returned to storage not kept on desks Clinical letters waiting to be scanned or filed should be kept in folders and not lef t visible. Records and Office area Doctors and Staff should not discuss patients in the earshot of reception Records should be kept in a secure area Call Systems Should a doctor call a patient in for a consultation by name? Is there any other way a pati ent can be called without breaching a confidence? Example - A practice installed an intriguing system of coloured and numbered tokens tha t were handed to patients after they had booked in at reception. The circular tokens had a hole in the middle just like a polo mint. A display board listed the doctors and their roo ms and each had a red light. On the wall below the display board was what can only be de scribed as a peg board with a series of pegs and above each pin a room number. On the p egs patients had hung their polo mints and the number on the last token was visible. When a doctor wished to call the next patient he pressed a button to ring a bell and flash a light against his name on the display board. Patients were then expected to look at thei r tokens and the peg board and if their number was the next one they were to place their toekn on the appropriate peg and take their turn to see the doctor. Asked why the practice had chosen this system, the answer was that the practice had a lar ge ethnic population and there were many patients with exactly the same name who coul d be in the waiting room at the same time! DISCUSSION POINT Calling patients by their name does not maintain confidentiality - Discuss? New Technology Great care needs to be taken when using new technology just as it would have done whe n using the old style paper records. Lloyd George records could be marked with a note th at there was a patient with a similar name. There is nothing so visible with a computer rec ord but it is still possible to scan a clinical letter and attach it to the wrong patient. Letter s attached to the wrong patient are extremely difficult to find. The process of receiving, r eading and scanning clinical letters needs to be watertight. All in all patients records must be kept safely, and securely. Conversations about or with p atients should be in a controlled environment. Conversations should not be able to be ov erhead. Clinical and personal information about patients should not be repeated to a thir d party without consent. WHO CAN BE KEPT IN THE LOOP Strictly speaking a patient’s health records should be kept and maintained by the health professional providing treatment and care. In a medical practice treatment and care can be provided by a doctor, your registered doctor, by a GP Registrar, by a Practice Nurse or a Nurse Practitioner. You may also see a Health Care Assistant or a Phlebotomist. So it is ' safe' to assume that all these persons can see your records. In a GP surgery some other staff may need as part of their job to look at and extract infor mation from your records. This might include a medical secretary who is making a Choos e and Book referral or typing a referral letter on behalf of a GP. Should the GP, however, be expected to provide a full draft of a referral letter? Other staff might have been given tasks to do looking for health data to enter from clinical letters or reports to claim Qualit y points. For reception staff and secretarial staff when asked a question about their records by a p atient it is always wise to pose the question do you mind me looking at your notes to chec k for you? Example – A temporary member of staff who was attending a medical school acted as a fi ling clerk for the summer months. One day her neighbour attended the surgery for an ap pointment. The medical student looked up the patients notes and discussed what she had found with her mother than night. Her mother repeated the information to her neighbou r. The medical student was dismissed. What about the patient you may well ask. Yes, legally the patient has a right to view their own medical records unless it would adversely affect their health to do so. If such a decisi on was made by a doctor it might be challenge in a court of law. ACCESS TO RECORDS Written applications from patients are few and far between and the law requires a respo nse within 40 days. Patients may ask for a copy of their records both manually held and co mputer held records. The practice has a right to charge for copying up to £50 and there is also legally a charge of £10 for access. Some clinical letters will bear a notation to the eff ect that the permission of the author must be sought to release such records. Sharing Records The issue of allowing access to records is now complicated by the fact that patients can a gree to share their records with other NHS sites and NHS services and vice versa. Recentl y too there has been a decision to share records and the information contained in them a nonymously. These arrangements for sharing records allow such services as the out of ho urs providers to view and edit patient records. But again consider who has access to these records. Back at the surgery the Practice and its staff need to be clear about who can access patie nt’s records. The midwife who is not employed by the practice might ask to see an expect ant mothers notes. Example - A member of staff mentioned to a midwife that one of her relatives was having problems with her pregnancy and described in detail her symptoms and attempted to dis cuss a resolution. The Midwife complained that a member of staff had been discussing wi th her confidential information about a patient. The member of staff was reprimanded. Other health care providers such as district nurses and health visitors also work at GP surg eries and might ask for access to records, which might be appropriate if specifically deali ng with a patient at a doctor’s request. However, other health care providers such as outp atient consultants, counsellors or physiotherapists would not have access to patient’s rec ords. PRIVATE REQUESTS FOR ACCESS The other area for discussion is access by third parties such as solicitors, insurance compa nies and health care professionals preparing medical reports. GPs have the right to charg e fees for access to records and for copying records. They also have the right to charge fe es for preparing medical reports themselves. This aspect of practice management was at one time quite a lucrative area of private income, but with the reduction in the mortgage market it is now less so. In any event a patient must give written consent to access to their own medical records by a third party. SUMMARY 1. There should be no access to records without a patient’s written consent. 2. Patient information should not be revealed visually to a third party. 3. Conversations about patients and with patients should not be overheard Robert Campbell www.kingfisherpm.com Email to robert.campbell@orange.net