High Risk Conditions and Treatment Primary to Syndrome X A
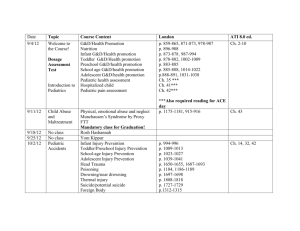
advertisement

High Risk Conditions and Treatment Primary to Syndrome X A Review of the Literature Hope Olson Advanced Nutrition Professor Johnson October 9, 2007 Abstract Since the late 1980's Syndrome X has been of concern among medical experts and dietitians. Several organizations have set standards on the core determinants of the disease, but there are still no set standards on how to classify and treat patients. This literature review inspects the various descriptions of Syndrome X, and how it came to be, how one can prevent it from happening to them, and the latest methodology professionals are utilizing to help their patients greet the road to improved health. Nutritional Support for Metabolic Syndrome X Patients: A Review of the Literature During a lecture in 1988, Gerald Reaven, MD, of the Stanford University School of Medicine, noted that several risk factors for CVD or cardiovascular disease commonly cluster together. These factors include hypertension, hyperglycemia, and dyslipidemia. Reavan referred to this group of factors as Syndrome X. Because insulin resistance underlies Syndrome X, this phenomenon has also been called insulin resistance syndrome, and metabolic syndrome (Meerschaert, 2005). The prevalence of Syndrome X varies slightly depending on the source and criteria used to diagnose this condition, however it is reported that generally 23% of women, and 24% of males have this condition (Davy & Melby, 2003). The astounding impact Syndrome X has on individuals has spiked the interest of medical professionals and dietitians world-wide. The lack of success in slowing the obesity epidemic, and the sparse nutrition and physical activity education in our nation are environmental hazards that add to the genetic hazards some individuals have of contracting the syndrome. This literature review considers the importance of recognizing the features Syndrome X, reducing it's prevalence by habit changes, and treating it with nutritional intervention. This review responds to the following questions: 1. What are the implications of Syndrome X? 2. How can individuals reduce their risks of contracting Syndrome X? 3. What are the current methods being practiced to treat this condition? What are the Implications of Syndrome X? Syndrome X has been categorized under slightly different definitions depending on medical associations, such as the National Cholesterol Education Program's Adult Treatment Panel III, and the World Health Organization, and also varies amongst physicians (Meerschaert, 2005). Table 1.1 offers the specific published criteria from the NCEP ATP III and WHO. Table 1.1 allows for the viability of different criterion, depending on the guidelines the practice treating a patient adheres to. To professionals in the dietetics field however, Syndrome X can be loosely identified in terms of the following signs and symptoms: insulin resistance, hypertension, abdominal obesity, atherogenic dyslipidemia, and a prothrombotic state (Panagiotakos, 2007). Brenda M. Davy, PhD, RD (2003) and her associate identify increased intra-abdominal adipose tissue as a possible initial cause in the development of this syndrome. They also mark that elevated stress-related cortical secretion, abnormal uric acid metabolism, inflammation, and polycystic ovary syndrome contribute to Syndrome X. This abdominal or visceral obesity, commonly referred to as the "apple shape" has been notorious for causing Diabetes Mellitus, and onset of other chronic diseases, such as heart disease. Interestingly enough, "insulin resistance as the primary defect" of Syndrome X has sparred the notion that it is a culprit in the development of cardiovascular disease (Coulston, Peragallo-Dittko, 2004). It is estimated that 20-25% of US adults have metabolic syndrome, "which means an increase in the risk of heart disease for a quarter of the US population" (Knopp, et al., 2003). Table 1.0 Published Criteria for Syndrome X Diagnosis Hypertension Dyslipidemia Obesity Glucose NCEP ATP III Current antihypertensive therapy or BP > 130/85 mm Hg. Plasma triglyceride level > 150mg/dL, HDL-c level < 40mg/dL in men, & < 50mg/dL in women. Waist circumference >/= 40 in. for men, and >/= 35 in. for women. Fasting blood glucose level > 110mg/dL Other Requirements for diagnosis Any three of the above disorders. WHO Current antihypertensive therapy &/or BP > 140/90 mm Hg. Plasma triglyceride level > 150mg/dL, &/or HDL-c level < 35mg/dL in men, & < 40mg/dL in women. BMI > 30kg/m &/or WHR > 0.90 in men, and > 0.85 in women. Type 2 diabetes or impaired glucose tolerance (IGT). Microalbuminuria (overnight urinary albumin) excretion rate > 20ug/min [30mg/g Cr]. Confirmed T2 DM, or IGT & any two of the above criteria. If normal glucose tolerance, must have three of the above. Note: Information obtained from Coulston & Peragallo-Dittko, 2004. This table identifies several traits that lead to the burdens and final contraction of the fullon condition and the reader has a chance to note some attention grabbing facts. Besides the fact the NCEP ATP III differs slightly from that of the WHO, one can easily establish high blood pressure, low levels of high density lipoproteins (HDL-c), obesity --specifically visceral, diabetes, and protein excretion are problems that the disease thrives on. According to Joyce Pastors, RD, MS, CDE, obesity and a sedentary lifestyle are the driving forces behind Syndrome X. The complications of being overweight are increasing: not only is type 2 diabetes affecting even younger populations; it's making them susceptible to a chronic illness that is multifaceted in terms of risks. One body of evidence points to insulin resistance as the essential cause of metabolic syndrome, and insulin resistance predispose people to the development of type 2 diabetes mellitus (Pastors, 2006). Outcomes of the predispositions include one hypothesis that has postulated a link between colorectal cancer, insulin resistance, and hyperinsulinemia (Lukaczer, 2001). Even more recently, speculation has centered on the link between hyperinsulemia and breast cancer (Lukaczer, 2001). Although these are frightening outcomes of this condition, the good new is most of the sub-conditions of Syndrome X can be prevented before they develop through lifestyle changes, behavioral changes, and education! How Can Individuals Reduce Their Risks of Contracting Syndrome X? Previous research has clearly shown that the individual components of Syndrome X are all modifiable by exercise. There has been established an inverse relationship between the prevalence of metabolic syndrome and cardio respiratory fitness, while adjusting for the potential influence and confounding factor of macronutrient intake (Sullivan, 2006). This means that Sullivan concurs exercise is a large factor in reducing one's risk of contracting Syndrome X, but that diet could confound some of the data since those who work out choose healthier food, on average. Of course, diet and exercise have complementary roles, and in the long run, they work better together than either component alone. "Generally speaking, diet has been shown to be more effective for overall weight loss, but exercise has more of an effect on weight maintenance and changes in body composition over time," including controlling diabetes, and changing body composition such as the HDL-C level (Sullivan, 2006). If a person consistently exercises and maintains an accelerated cardiorespiratory function, they are less likely to become obese, and contract this bundle of complications know as Syndrome X. Diet plays a large role in deflecting the risks associated with Metabolic Syndrome. The ATTICA study completed by Demosthenes Panagiotakos and his associates concluded "a dietary pattern that includes cereals, fish, legumes, vegetables, and fruits was independently associated with reduced levels of clinical and biological markers linked to the metabolic syndrome, whereas meat and alcohol intake showed the opposite results." This diet was inversely related to the likelihood of Syndrome X. Another evidence based study recommended by both the American Heart Association (AHA) and the NCEP ATP III, is to limit the intake of foods with a high content of cholesterol-raising fatty acids -- saturated fatty acids, and transfatty acids (Coleman, 2002). Both organizations encourage individuals to replace those foods with unsaturated fatty acids from fish, vegetables, legumes, and nuts, and with carbohydrates from grains and fruits (Coleman, 2002). What are the Current Methods Used to Treat this Condition? The diet can be used as a tool to promote a healthy lifestyle and combat the components of Syndrome X. It is commonplace for people with high contents of LDL, or total cholesterol to use a statin, which is drug that fixes part of the problem. One may temporarily fix insulinsensitivity or resistance with insulin shots. Individually or congressionally, these characteristics, among others, that are clustered together forming Syndrome X can be treated through a diet high in monounsaturated fats, and low in carbohydrate. "High carbohydrate diets can increase triglycerides, lower high-density lipoprotein (HDL) cholesterol, and worsen glucose tolerance in individuals with the metabolic syndrome" (Coleman, 2002). In one study recorded by Coleman from Grundy and colleagues, discovered that a high carbohydrate, very low-fat diet lowers HDL. That is not what most people would think since fat is "bad." It is the ratio of LDL to HDL that is unhealthy, if the LDL is too high. The study went on to say that instituting a low-fat diet supplemented with monounsaturated fat resulted in less HDL lowering than a very low-fat diet (Coleman, 2002). The "Dietary Effects on Lipoproteins and Thrombogenic Activity" (DELTA) study found that high monounsaturated fat diets reduced HDL cholesterol by only 4% compared to the 7% for the low fat diet. In addition, the high-monounsaturated fat diet did not increase the triglycerides compared to the 7% increase on the low-fat diet (Coleman, 2002). Another benefit from a higher monounsaturated fat diet (providing the patient still looses weight) is the ability for MUFA to be less susceptible to oxidation than polyunsaturated fatty acids. Since MUFA's are not easily oxidized, they contribute much less to atherosclerosis, which is great news for treating CHD. The NCEP ATP III recommends a therapeutic lifestyle change as the first priority of treatment for individuals with risk factors that can be related to lifestyle, such as obesity, sedentary lifestyle, elevated plasma glucose levels, high triglyceride values, or low HDL-C levels (Sullivan, 2006). The ways in which people would receive this treatment include but are not limited to weight loss counseling, regular exercise, and therapeutic diet, similar to that of the MUFA incorporated diet described above. This approach, though idealistic, would have benefits such as improved "plasma triglyceride and HDL cholesterol values while offering promise for reducing the burden of medication required to improve the risk factor profile" (Sullivan 2006). The approach is idealistic in terms of the patients’ readiness for this kind of commitment, and psychological strength. It will require persistence and careful planning of exercise, diet, and behavioral change. Almost all of the signs and symptoms of Syndrome X are acquired over a long period of time, and can result in serious medical treatment. Treating hypertention, dyslpidemia, visceral obesity, and insulin resistance is difficult, costly, and time consuming with the use of drug therapy, and in the case of obesity, is not an answer. There are numerous evidence based studies concluding that therapeutic lifestyle changes and a diet high in monounsaturated fatty acids and low in carbohydrate offer great hope to patients with Syndrome X. Prevention of the syndrome is directly correlated with a moderate diet consisting of fruits, vegetables, legumes, cereals, fish, and MUFAs. This ultimately leads to educating the public on the benefits of these foods and how easy it is to obtain these nutritional resources. Exercise will aid in weight loss and maintenance, a key to preventing the onset of visceral obesity, the precursor to Syndrome X. While the conditions of Syndrome X are unique in that they are, for the majority, preventable by behavior changes and healthy food attitudes, they still need to be further analyzed in depth in light of dietary treatment. References Coleman, Ellen. (February, 2002). Monounsaturated Fat, Metabolic Syndrome, and CHD. Today's Dietitian, 15-17. Exert obtained from Betty Larson, RD, FADA. Coulston, Ann M., Peragallo-Ditkko, Virginia (2004). Insulin Resistance Syndrome: A Potent Culprit in Cardiovascular Disease. Journal of the American Dietetic Association, 104, 176-178. Davy, Brenda M., Melby, Christopher L. (2003). The Effect of Fiber-Rich Carbohydrates on Features of Syndrome X. Journal of the American Dietetic Association, 103, 86-93. Knopp, R. H., Retzlaff, B., Fish, B. et. al. (2003). Obesity, Insulin Resistance, and Heart Disease. Nutrition Close Up, 20, 1-3. Lukaczer, Dan. (2001). Nutritional Support for Insulin Resistance. Applied Nutritional Science Reports. 1-5. Pages 1-5 are those of an exert from ANSR, obtained from Betty Larson, RD. Meerschaert, Carol M. (December, 2005). Metabolic Syndrome: What's in a Diagnosis? Today's Dietitian, 40-43. Exert obtained from Betty Larson, RD, FADA. Panagiotakos, D. B., Pitsavos, C., Skoumas, Y., Christodoulos, S. (2007). The Association Between Food Patterns and the Metabolic Syndrome Using Principal Components Analysis: The ATTICA Study [Electronic version]. Journal of the American Dietetic Association, 107, 979-986. Pastors, Joyce Green. (March, 2006). Metabolic Syndrome: Is Obesity the Culprit? Today's Dietitian, 12- 16. Exert obtained from Betty Larson, RD. Sullivan, Vicki K. (2006). Prevention and Treatment of the Metabolic Syndrome with Lifestyle Intervention: Where Do We Start? [Electronic version]. Journal of the American Dietetic Association, 106, 668-670.