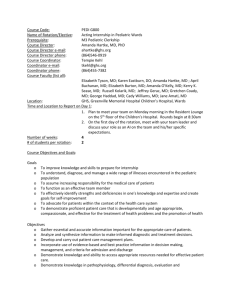
Final Recommendations January 19 2015
advertisement

Criteria Judgeme nts ○ No ○ Probably no Problem Is there a problem priority? ○ Uncertain ● Probably yes ○ Yes ○ Varies Additional considerat ions Research evidence What we knew: The mortality of post cardiac arrest patients is high. Post arrest management has the potential to improve survival and neurologic outcomes. Hyperventilation (leading to hypocapnia) reduces cerebral blood flow and is associated with worse outcomes in children following stroke or traumatic brain injury and hypoxic ischemic injury in neonates. Alternatively, hypercapnia can increase cerebral blood flow which could increase intracranial pressure and worsen metabolic acidosis. Alternatively, mild hypercapnia improves cerebral perfusion and may have neuro-protective effects after brain injury in animal studies. What is added with this review: The prevalence of dyscarbia during the first hours after ROSC is high: up to 55% of the total of patients included in the reviewed studies (36.2% hypercapneic and 25% hypocapneic). The 2 studies selected have been published recently (2012, 2013), are observational and only include non-traumatic patients suffering both in and out-of- hospital cardiac arrest. The Del Castillo study reports a negative association between hypocapnia and outcome and a negative association with hypercapnia and outcome, whereas the Bennett reported no association between ventilation status and outcome. What is added from the adult taskforce on ventilation strategy post cardiac arrest: All studies are observational, recent (2012-2014), and only include non-traumatic cardiac arrest patients. All studies showed a trend or worse outcomes with hypocapnia and hypercapnia. ○ No included studies What is the overall certainty of this evidence? Benefits & harms of the options ● Very Outcome low ○ Low ○ Relative importance ○ High Survival with Favorable neurological/functional outcome at discharge in pediatric patients CRITICAL ○ Survival to hospital discharge in pediatric patients IMPORTANT Moderate Is there important uncertaint y about how much people value the main The relative importance or values of the main outcomes of interest: Certainty of the evidence (GRADE) ⨁◯◯◯ VERY LOW ⨁◯◯◯ VERY LOW Important uncertaint y or Summary of findings: normocapnia variability ○ Possibly important Outcome Without ventilati With ventilati Differe nce Relati ve Criteria outcomes ? Judgeme nts uncertaint y or variability on to on to hypercap hypercap nia nia ○ Probably no important uncertaint y of variability ● No important uncertaint y of variability ○ No known undesirab le Additional considerat ions Research evidence Survival with Favorable neurological/fun ctional outcome at discharge in pediatric patients Survival to hospital discharge in pediatric patients 474 per 1000 669 per 1000 (95% CI) effect (RR) (95% CI) 359 per 1000 (235 to 551) 114 fewer per 1000 (from 77 more to 239 fewer) RR 0.758 7 (0.495 3 to 1.162 2) 320 per 1000 (178 to 575) 349 fewer per 1000 (from 95 fewer to 491 fewer) RR 0.478 (0.266 2 to 0.858 2) With ventilati on to hypocap nia Differe nce (95% CI) Relati ve effect (RR) (95% CI) 140 fewer per 1000 (from 68 more to 268 fewer) RR 0.703 7 (0.433 4 to 1.142 6) ○ No ● Probably no Are the desirable anticipate d effects large? ○ Uncertain ○ Probably yes ○ Yes ○ Varies Are the undesirab le anticipate d effects small? ○ No ○ Probably no ○ Uncertain ● Probably yes Outcome Without ventilati on to hypocap nia Survival with Favorable neurological/func tional outcome at discharge in pediatric patients 474 per (assessed with: 1000 PCPC 1-2 or no change with baseline pre-CA)Bennett, CCM, 2013 333 per 1000 (205 to 541) Criteria Judgeme nts ○ Yes ○ Varies ○ No ○ Are the desirable effects large relative to undesirab le effects? Additional considerat ions Research evidence Survival to hospital discharge in pediatric patients- Del Castillo, Resuscitation, 2012 669 per 1000 556 per 1000 (305 to 1010) 114 fewer per 1000 (from 341 more to 364 fewer) RR 0.829 8 (0.456 3 to 1.508 9) Probably no ● Uncertain ○ N.B. Del Castillo did not study survival with favourable neurological outcome at discharge. Bennett does not present the data on survival to hospital discharge by ventilation category thus is not included in this RR calculation. Probably yes ○ Yes ○ Varies ○ No ○ Probably no Are the resources required small? ○ Uncertain ○ Probably yes ● Yes ○ Varies Resource use Is the increment al cost small relative to the net benefits? ○ No ○ Probably no ● Uncertain ○ Probably yes The additional resources required would be possibly more frequent blood gases (depending on institution baseline) and adjustments on the ventilator. Pre-hospital monitoring of ventilation after ROSC is desirable, especially if the pre-hospital time is long. The equipment necessary to monitor ventilation is not frequently available for pre-hospital providers. In the in-hospital setting this monitoring is a standard of care. Criteria Judgeme nts Research evidence ○ Yes ○ Varies ○ Increased Depending on the ability to do blood gas monitoring and make ventilator changes. ○ Equity What would be the impact on health inequities ? Probably increased ● Uncertain ○ Probably reduced ○ Reduced ○ Varies ○ No ○ Acceptab ility Is the option acceptabl e to key stakehold ers? Probably no ○ Uncertain ● Probably yes ○ Yes ○ Varies ○ No ○ Feasibilit y Is the Probably option feasible to no implemen t? Uncertain ○ ● Probably It would likely be acceptable to stakeholders to monitor pCO2, as this is currently the standard of care in the hospital setting. Monitoring EtCO2 is becoming the standard in pre-hospital settings as a surrogate marker for quality of CPR and detection of ROSC and thus it may be acceptable to continue to monitor EtCO2 until arrival to a hospital, even though the evidence is of low quality. Additional considerat ions Criteria Judgeme nts Additional considerat ions Research evidence yes ○ Yes ○ Varies Recommendation Should ventilation to hypercapnia vs. normocapnia be used for infants and children with ROSC after cardiac arrest in any setting? Balance of consequences Undesirable consequences clearly outweighdesirable consequences in most settings Undesirable consequences probably outweigh desirable consequences in most settings The balance between desirable and undesirable consequences is closely balanced or uncertain Desirable consequences probably outweigh undesirable consequences in most settings Desirable consequences clearly outweigh undesirable consequences in most settings ○ ○ ● ○ ○ Type of recommendation Recommendation We recommend against offering this option We suggest not offering this option We suggest offering this option We recommend offering this option ○ ● ○ ○ We suggest maintaining pCO2 with normal physiological range (30-50mmHg) as part of a post ROSC bundle of care (weak recommendation, very low quality of evidence). Part A. Hypercapnia vs. Normocapnia Justification For the critical outcome of survival to hospital discharge with favorable/functional neurological outcome in pediatric patients (assessed with PCPC 1-2 or no change with baseline pre-CA), we have identified very low quality evidence from one observational study [Bennett, 2013, 1534] of 195 pediatric in and out-of-hospital cardiac arrest survivors to at least 6 hours post-arrest (down-graded for indirectness, imprecision and serious risk of bias) showing no benefit of hypercapnia (> 50 mmHg) (Relative Risk of survival to hospital discharge with favorable/functional neurological outcome is 0.7587, CI 0.4953 to 1.1622). For the important outcome of survival to hospital discharge in pediatric patients we have identified very low quality evidence from one observational study [Del Castillo, 2012, 1456] of 223 pediatric patients suffering an in-hospital cardiac arrest (down-graded for inconsistency, indirectness, imprecision and serious risk of bias). This study showed worse outcome with hypercapnia (≥ 50 mmHg) (Relative Risk of survival to hospital discharge is 0.478, CI 0.2662 to 0.8582). Part B. Hypocapnia vs. Normocapnia For the critical outcome of survival to hospital discharge with favorable/functional neurological outcome in pediatric patients (assessed with PCPC 1-2 or no change with baseline pre-CA), we have identified very low quality evidence from one observational study [Bennett, 2013, 1534] of 195 pediatric in and out-of-hospital cardiac arrest survivors to at least 6 hours post-arrest (down-graded for indirectness, imprecision and serious risk of bias) showing no benefit of hypocapnia (< 30 mmHg) (Relative Risk of survival to hospital discharge with favorable/functional neurological outcome 0.7037, CI 0.4334 to 1.1426). For the important outcome of survival to hospital discharge in pediatric patients we have identified very low quality evidence from one observational study [Del Castillo, 2012, 1456] of 223 pediatric suffering an in-hospital cardiac arrest (down-graded for inconsistency, indirectness, imprecision and serious risk of bias) showing no benefit of hypocapnia (< 30 mmHg) (Relative Risk of survival to hospital discharge is 0.8298, CI 0.4563 to 1.5089). There were no subgroups analyzed in the two pediatric studies. Subgroup considerations Patients being treated with therapeutic hypothermia would require temperature corrected interpretation of blood gases to avoid excessive hypocapnia. Patients with lung injury may benefit from less aggressive respiratory ventilation targets and a strategy of "permissive hypercapnia" to minimize risk of ventilator-induced lung injury. Acceptability: current recommendations are to consider performing blood gas analysis every 10 to 15 minutes after establishing initial mechanical ventilator settings and make appropriate adjustments. If we were to institute pCO2 targets, this would align with this 2010 ILCOR recommendation. Targets may be acceptable in the pre-hospital setting where EtCO2 detectors are in use. The evidence may not be strong enough to institute EtCO2 detectors for the sole purpose of targeting normocapnia in the pre-hospital setting. Implementation considerations Feasibility: Achieving pCO2 targets may be difficult (as evidenced in Roberts's CCM 2014 study) but in all patients who are intubated and can have blood gas analyses, it is feasible to target pCO2. Aiming to avoid hypocapnia could result in hypercapnia. The long term consequences of hypercapnia are more unclear than they are for hypocapnia. Time frame: No study went beyond 24h. Duration of targeted pCO2 would depend on patient's condition and their ability to control their own CO2 (pressure supported ventilation vs mandatory ventilatory strategies) Accountability: In most cases, the most responsible physician will be accountable to the targets in the in-hospital setting. Monitoring and evaluation Research possibilities Studies need to look at both mean PCO2 (temperature corrected where appropriate), and variability of PCO2. The more values the better and all must have temporal correlation. No analysis should be performed without adjusting for age, Utstein criteria, prescribed ventilation, comorbidities (e.g. lung disease), oxygenation, cooling. Degree of dyscarbia should be reported and analyzed. Currently, a multicenter RCT in adult population has been started to evaluate a strategy of normocapnia versus mild hypercapnia during the first 24h. Similar studies would be desirable in the pediatric population. The available studies are observational and very heterogeneous regarding patients, methodology and outcomes. Additional research evaluating the balance between lung protection parameters and permissive hypercapnia versus standard ventilatory parameters and normocapnia may be interesting, as respiratory etiology is common among the pediatric population. It would also be interesting to determine which is the most desirable method of evaluating PaCO2 during hypothermia in pediatric patients (ph-stat or alpha-stat).