makerere university faculty of medicine curriculum for the bachelor
advertisement

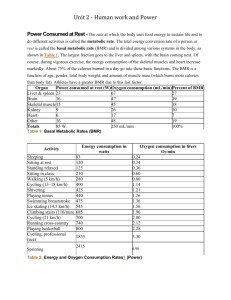
MAKERERE UNIVERSITY FACULTY OF MEDICINE CURRICULUM FOR THE BACHELOR OF SCIENCE IN MEDICAL RADIOGRAPHY (BMR) DEGREE 1.0 GENERAL INTRODUCTION The Department of Radiology, Makerere University offers a degree in Medical Radiography i.e. Bachelor of Science in Medical Radiography. The graduates will attain either Bachelor of Science Medical Radiography Imaging or Bachelor of Science Medical Radiography Therapy. The aim is to produce a broad based professional who can perform multiple tasks and cope with recent advances in diagnostic and therapeutic radiography. In order to address the current Government Health Strategic Investment Plan, there will be a mandatory internship of six months following the successful completion of the programme. The internship will be carried out in the Regional Government hospitals and Non-Governmental hospitals. A radiologist at the centre or a senior radiographer will supervise the interns. A satisfactory report will be provided by the supervisor regarding the entire period of internship. In developing this Programme, the training needs, population health care needs and the diagnostic and therapy equipment available in the country have been considered. Background: Radiography training in Uganda started from a humble beginning at the level of Assistant Radiographer Certificate in 1953. Fourteen years later, the course was upgraded to a Diploma level under the Society of Radiographers of U.K. This was made possible by the commissioning of New Mulago Hospital in 1962 with a modern X-ray Department and a range of X-ray equipment that was used for training. From 1966 to 1982, the awarding body of the diploma was the College of Radiographers, UK. From 1982 to date, the awarding body for the Diploma in Medical Radiography has been Makerere University. The programme is run under the jurisdiction of the Department of Radiology. When the programme transferred to Makerere University, the entry qualifications were upgraded to the minimum university entrance requirements of two principal passes in science subjects and two subsidiaries passes. Justification: Though Radiography training in Uganda has been going on for the last four and a half decades there has not been much change in curriculum content despite the changes in technology and the radiographers’ roles. The following phenomena justify the introduction of a degree programme in the training of radiographers. a) The role of a radiographer in tertiary and district hospitals is rapidly changing from that of a simple technician to that of a team-member in the delivery of high quality health care (2). Radiographers are increasingly being called upon by doctors to discuss results of imaging examinations, for purposes of making a correct diagnosis. b) The wider availability of new imaging modalities in the country and beyond has meant increased time of contact between patients and radiographers. c) Technological advancement in the field of radiology has also resulted in an unprecedented explosion of knowledge in the areas of diagnostic, therapeutic and interventional radiology. d) The Computerization of imaging and radiotherapy equipment requires increased knowledge and skills in computer science. 2 e) Over the last 10 years, many Ugandan students have abandoned radiography to join degree programs at the University. A degree programme in radiography should reduce this trend, and create better opportunities for career development. f) Higher degrees in Radiography are only accessed through prior acquisition of an internationally recognized university undergraduate degree. g) Both radiologists and radiographers must promote the highest standards of training and service delivery in both professions to avoid professional stagnation and decadence since a decline of quality in one adversely affects the other. This can be best achieved through the introduction of a training programme at degree level. h) It is through scholarly teaching and research that the profession of radiography in Uganda will maintain its rank of recognition by international bodies and at the same time, Ugandan communities will receive radiography services of a standard presently available only in the developed countries. i) Makerere has always maintained a pioneer role on the African continent in medical training. Through this programme, Makerere University will earn itself a place as the first University in this region to offer a degree in medical radiography. Moreover, the College of Radiographers (in the U.K) which parented radiography training centers in the Commonwealth recommended the introduction of Radiography degree training programmes, way back in 1990 (1). 2.0 OVERALL GOAL To produce graduate radiographers who are equipped with the necessary knowledge, skills and professional conduct to undertake the appropriate diagnostic imaging examinations or radiation therapy procedures. 4.0 PROGRAM OBJECTIVES The program is designed to produce graduate radiographers who: • Will demonstrate the research skills aimed at improving on the present knowledge and practice, and to develop new scientifically acceptable methods of medical imaging or radiotherapy. • Will demonstrate leadership skills, as they will be called upon to head the already existing centers in the country, and to open up new ones. • Understand the principles, ethics and legal responsibilities of health care practice and activate measures to promote the health and safety for themselves and others. • Are self-directed and lifelong learners who will be able to adapt to changing circumstances in Uganda, and elsewhere keep up with development in their profession and have the necessary motivation and background to acquire relevant specialized qualifications to fulfil the needs of the country and to advance their own careers • Exhibit high levels of administrative insight, skills and integrity and • Are more committed to the person than to the disease and display social responsibility 3 Health Professional Training: There is a worldwide revolution in the training of Health Professionals. This has been brought about by demands for a health worker with a whole new set of competencies to complement the existing clinical proficiency. Some of these are: • Life long self-directed learning skills • Critical and innovative thinking • Communication skills • Managerial/Administrative skills • Social responsibility The traditional curriculum currently in use in the Faculty of Medicine Makerere University provides learning experiences, which are mainly modeled on the Tertiary Teaching Hospital patient ward mix. While this produces clinically competent health workers, it does not adequately equip the graduates to effectively implement Primary Health Care (PHC). Furthermore it does not impart the new competencies demanded in the market place. The need to change the curriculum at the Faculty of Medicine, Makerere University has therefore been born out of the following factors: 1. The need to produce a Health worker with expanded competencies 2. The decentralization of services and in particular health services to the Health sub-district calling for a new health care provider. 3. The demands by the community for a health worker who is a good communicator and possesses of good public relations skills 4. The adoption of Primary Health Care as central to the strategic plan of the Ministry of Health. 5. The aspirations of the students, staff and employers as expressed in a study that investigated client satisfaction with the Makerere graduate and need for curriculum change. 6. International visits to selected universities in Africa, Europe, Asia, Australia and Canada also highlighted and emphasized the need for change of the curriculum to one that is student centered and promotes social responsibility to communities. Health sector strategic plan has decentralised service delivery to the health sub-districts. The capacity of the district workers to handle these expanded responsibilities was found wanting by a human resource audit conducted by the Makerere Institute of Social Research. (MISR) The Faculty of Medicine took stock of its training through a feasibility study and decided to review the curriculum in order to produce health workers who match the new demands of the districts and also keeping in mind changes talking place in medical education elsewhere in the world. The feasibility study established, expressed support for curriculum review by the public, students, employers, as well as members of the faculty. It also established: • The need to address relevance of course content • The needs to provide horizontal integration across disciplines and vertical integration of pre-clinical and clinical and community aspects of learning 4 • The need to provide community teaching sites • Provision of a student-centered learning through Problem Based Learning (PBL) During the pilot stage for curriculum review it became clear to the Education Committee that the task of curriculum review is a major one, lengthy and costly. The committee therefore decided on a phased approach to ensure feasibility and adopted a grassroots participatory approach to ensure ownership and continuity and accountability. 5.0 VISION OF THE FACULTY OF MEDICINE “To be a center for academic and health service excellence” 6.0 MISSION OF THE FACULTY OF MEDICINE “We are dedicated to improving the health of the people of Uganda and beyond, promoting health equity by providing quality education, research and health services. We achieve this by enhancing capacity and participation of stakeholders; strengthening systems and partnerships; and harnessing the power of new sciences and technology so as to build and sustain excellence and relevance” 7.0 STUDENT CAPACITY AND FUNDING Mainly the programme shall be privately sponsored, Government will avail funds for at least five government-sponsored students per intake. Total intake will be 30 students per year i.e. 25 private students and 5 Government sponsored students. 8.0 DESIGNS AND STRUCTURE OF THE CURRICULUM This curriculum provides for student centered learning, encourages critical thinking and problem solving through PBL. It advocates for integration of learning experiences and is community oriented. It also includes non traditional subjects like management and communication. 8.1 Curriculum Design: a) Integration Since the human being functions as an integrated whole, the learning experiences must be as contextual and holistic as possible in order to enable the health worker to deal with an individual rather than a body part or a disease process. This is ensured in the curriculum design through two levels of integration. i) The horizontal integration: This breaks down boundaries between disciplines like: Anatomy, Physiology, Biochemistry and provides a package of learning experiences of the Biomedical Sciences. This does away with the compartmentalization and eliminates repetition of subject content. The Horizontal integration goes hand in hand with the vertical integration. ii) The Vertical integration: The vertical integration ensures that all levels of the learning spiral, thus students are exposed to Basic Sciences, Clinical experiences and community health activities right from first year. 5 Biomedical Sciences are covered in the first 2 years and continue into the clinical clerkships. Conversely the clinical experience starts small and broadens out into the clerkships (Figure 1). The community exposure is constantly applied in appropriate doses through out the programme. Figure 1 demonstrates Biomedical Sciences and Clinical Biomedical Sciences Clinical Sciences 1st Year 3rd Year b) Active Student Learning through PBL There are several methods of student learning each with its advantages and disadvantages. Problem Based Learning has been identified as that which best encourages, active student learning, critical and analytical thinking/learning in context, problem solving and self-directed learning. For this reason the proposed curriculum is student centered which encourages active student learning through PBL. c) Early Clinical Exposure Early clinical exposure is important in helping the students integrate and apply Biomedical Sciences to patient management. It is proven to be a strong stimulus to learning. Early clinical exposure is gained through paper cases, mutated clinical cases, skills lab and actual cases. d) Community Based Education and Service (COBES) COBES is vital for contextual learning and management of community health problems. It also acquaints and familiarizes the students with the environment in which they are required to operate upon qualification. COBES is provided for in the proposed curriculum through district community teaching sites. c) The Spiral Curriculum Four main themes are represented in the various phases of the learning experiences. These are: • The Normal structure and Functions (phase 1) • The Abnormal structure and Functions (phase 2) • Clinical practice (phase 2) • Community medicine (phases 1 and 2) All 4 themes are introduced at level 1 in various degrees of depth. New information in the next level is introduced in such a way that there is a link with the information obtained from the previous level. Previous learning, therefore acts as building blocks, as students “walk” their way through from phase 1 to Phase 2. 6 8.3 Curriculum Structure: The curriculum is organised into Courses and Blocks. a) The Courses These represent the subjects to be learned. Each has Course Objectives, course content, mode of delivery and contact hours. The course content is integrated and is developed by interdisciplinary teams of subject experts. The course content is influenced by the following factors: • Course objectives which are based on the health needs of the population. • Level of learning in the spiral of the curriculum • Time available in the academic calendar • Approval by Content experts The instruction and learning of the agreed course content is guided by problems developed by the interdisciplinary teams. b) The Learning Blocks Related courses are organized into an examinable set called the Learning Block. Courses are the building units of a block. The “Blocks” are the building units of the curriculum. The objectives of the Blocks are similar to the program objectives, which are usually expressed as competencies. These competencies are in turn based on the population health needs and other priorities addressed by the program. The proposed blocks contain two to three courses and therefore last from 5-15 weeks. The semesters are made up of 1-2 blocks. (See Curriculum map) c) Phases The learning experiences are organized into 2 Phases which spiral into each other. Phase 1 Predominantly covers principles of learning or teaching methodologies and foundations of medical education, the normal structures and functions. It extends over the 1st and 2nd years of study Phase 2 Predominantly exposes the students to Pathophysiology and Clinical experience Community practice is cross cutting. It is scheduled for in every year except the final year. 9.0 POLICIES GOVERNING THE CURRICULUM REGULATIONS The title of this program shall be Bachelor of Bachelor of Science in Medical Radiography degree (BMR) This is a three-year programme. Every academic year consists of two 17-week semesters and one 10-week recess term except the final year, which has no recess term. The course shall be governed by the general regulations and statutes of the University and in addition by regulations of the faculty. 10.0 ADMISSION REQUIREMENTS Direct Entry Scheme: A candidate shall be eligible for admission into the programme on meeting the following minimum requirements. The Uganda Certificate of Education (Ordinary level) or its equivalent AND 7 Two principal passes in approved science subjects at the same sitting of the Uganda Advanced certificate of Education Examination (Advanced level) or its equivalent. The essential subject shall be Biology. The relevant subjects shall be two best done of Physics, Chemistry and Mathematics. Diploma Entry Scheme: A Diploma in Medical Radiography of Makerere University or the equivalent. Mature Age Entry Scheme: Applicants must pass a Makerere University Mature Age Examination. Degree Holders Entry Scheme: Degree holders in Biological Sciences shall be considered for admission. 11. 0 COURSE STRUCTURE AND DURATION The Bachelor of Science in Medical Radiography Program shall normally extend over a period of 3 years. Each year shall consist of 2 semesters and a recess term except the 3rd year, which shall consist of two semesters only. Length of a semester A semester shall be 17 weeks, 15 weeks for teaching and 2 weeks for examinations. Type of Courses The Courses in the Programme shall be classified as Core Courses. Therefore, the students shall be required to register for and pass all the Courses in the First and Second years. In the Third year students shall register for Courses either in Medical Imaging or Radiation Therapy. Programme structure The lay out of the programme is shown below. Appropriate codes have been used. BMR: Is the code for Bachelor of Science in Medical Radiography. Cl.H = Clinical hours LH = Lecture hours PH = Practical hours TH = Tutorial hours SH = Self directed learning hours CH = Contact hours CU = Credit units The Course Pass Grade is 2.0. No grade shall be awarded for any Course in which the student fails. 12.0 GRADING OF COURSES Each course shall be graded out a maximum of 100 marks and assigned appropriate letter grades and grade point as follows: Marks Letter Grade Grade Point 80 – 100 A 5.0 75 – 79.9 70 – 74.9 B+ B 4.5 4.0 65 – 69.9 B- 3.5 8 60 – 64.9 C+ 3.0 55 – 59.9 C 2.5 50 – 54.9 C- 2.0 45 – 49.9 D+ 1.5 40 – 44.9 D 1.0 35 – 39.9 Below 35 DE 0.5 0 c) Retaking a course or courses i) A student shall retake a Course or Courses when next offered in order to obtain at least the Pass mark of 50. ii) A student who fails to obtain at least the Pass Mark (50%) during the Second Assessment in the same course or Courses he/she has retaken shall receive a written warning. iii) A student may retake a Course when next offered again in order to improve his/her Pass Grade(s) if the Pass Grade got at the first Assessment in the Course or Courses was low. iv) While retaking a Course or Courses, a student shall: a) Attend all the prescribed lectures/tutorials/ Clinicial/ Practicals/Fieldwork in the Course or Courses; b) Satisfy all the requirement for the Coursework component in the Course or Courses and; c) Sit for the University examinations in the Courses or Courses A student shall not be allowed to accumulate more than five (5) retake courses at a time. In any case a student shall not be allowed to proceed to the next phase without clearing all retakes in the previous phase. d) Pre-requisite Conditions i) A final year student whose final Examination Results have already been approved by the relevant Faculty/Institute Board and has qualified for the Award of the Degree, shall not be permitted to retake any Course or Courses ii) When a student has retaken a course to improve his/her grade the better of the two Grades he/she has obtained in that Course shall be used in the computation of his/her Cumulative Grade Point Average (CGPA) iii) Whenever a Course or Courses has/have been retaken, the Academic Transcript shall indicate so accordingly. e) Progression Normal Progression Normal Progression shall occur when a student has passed the Assessments in all the Courses he/she had registered for in a particular Semester. Probationary Progress A student who has obtained the Cumulative Grade Point Average (CGPA) of less than 2.0 shall be placed on Probation. Such a student shall be allowed to progress to the next Semester/Academic Year in that phase if feasible but shall have to retake the Course(s) he/she had failed, and obtain at least the Pass Mark (50%) in the Course(s). 9 f) Certificate of Due Performance A student shall be responsible for keeping a record of all learning experience in a logbook, which should be duly signed by the student, clinical supervisor and tutor/ lecturer; for presentation to the Head of Department, before a Certificate Of Due Performance can be issued. Attendance of classroom, clinical and fieldwork shall constitute 20% of the Progressive Assessment (ITPA) mark the total of which is 40%. A candidate will be denied a Certificate of Due Performance in any course, if attendance and performance in class, clinicals and or practicals are deemed unsatisfactory. A candidate will be denied a Certificate of Due Performance for a course if on evaluation, the student’s performance in any of the three components below is deemed unsatisfactory viz: Attendance performance in class practicals. Such a candidate will not be allowed to sit the examinations for the course in question g) Absence from examination i) If the Faculty/ Institute Board found out that a student has no justifiable reason for having been absent from a particular examination, such a student shall receive a fail (F) Grade for the Course(s) he/she had not sat the examination in. The Course(s) in which the Fail (F) Grade was/were awarded shall also count in the calculation of the CGPA. ii) If the Faculty/Institute Board is satisfied that a student was absent from a final examination due to justifiable reasons(s) such as sickness or loss of a parent/guardian, then a Course Grade of ABS shall be assigned to that Course(s). The student shall be permitted to take the final examination when the Course would be next offered or at the next examination season if the Course coordinator concerned can make the appropriate arrangements for the examinations. h) Discontinuation a) When a student accumulates three consecutive probations based on CGPA he/she shall be discontinued. b) A student who failed to obtain at least the Pass Mark (50%) during the Third Assessment in the Same Course or Courses he/she had retaken shall be discontinued from his/her studies at the University. c) A student who has overstayed in an Academic Programme by more than Two (2) years shall be discontinued from his/her studies at the University. 13.0 SPECIFIC OUTCOMES On completion of the undergraduate medical education and training program, the graduate radiographer must have knowledge, skills and attitudes as outlined below. a) Knowledge outcomes The program must produce a radiographer who has essential knowledge necessary for diagnostic imaging or radiation therapy, including knowledge of: • Biomedical sciences as a foundation for clinical medicine • Psychological, social, environmental, spiritual and cultural factors that contribute to illness and disease of individuals, families and communities. • Principles of health promotion and disease prevention • A clinical reasoning process that leads to problem solving • Pathophysiology of common problems encountered in medical practice • The principles of rational therapeutics • Rational use and ordering of basic and special investigations • Common problems encountered in health care 10 • Health care problems encountered in primary, secondary and tertiary health care • Epidemiology and biostatistics • Health service management and administration • Ethical issues relevant to medical practice b) Skills outcomes The program must produce a radiographer who has essential skills that are required for medical practice, including the following: • Communication skills including: ! Language skills ! Computer skills ! Interviewing skills ! Writing skills ! Referral skills ! Team work • Clinical skills including: ! History taking ! Interpretation of radiological findings ! Making a comprehensive assessment based on illness and disease ! Formulation of a comprehensive and shared management plan c) Attitudinal /behaviour outcomes The program must produce a radiograph who has an appropriate attitude for medical practice, such as the following: • Commitment to the person rather than disease or special technique • Awareness of the subjective aspects of medicine, that is, sensitivity to feelings, thoughts, concerns and expectations of patients and also awareness of own values, attitudes and feelings • Ability to listen actively with empathy in order to appreciate the purpose and intentions of patients • Ability to build trust through being worthy of trust • Ability to negotiate agreements that honestly reflect interests of both radiographer and patient • Respect for cultural diversity and patients’ beliefs • Positive approach towards primary health care and community-based education and service • Understanding the general code of conduct of a radiographer towards patients • Appreciation of health as a human right • Understanding the radiographers’ responsibilities towards his colleagues and other members of the health care team 14.0 ASSESSMENT METHODS Formative and summative assessment shall be conducted through MCQs. Modified essays, short notes, Objective Structure Clinical Examination (OSCE), Objective Structure Practical Examination (OSPE) and Logbook Logbook A student shall be responsible for keeping a log book of her/his practical experiences for presentation to the Course coordinator before a Certificate of due Performance is issued. The number of cases for the logbook are indicated for each case. There shall be an assessment and feedback session for every student and tutor at the end of every tutorial session. 11 This will include: a) Continuous assessment during all the learning sessions. This permits immediate feedback. In addition Logbooks and case write-ups will be assessed. This will contribute 40% of the mark b) An end of the block examination consist of: • Individualized process assessment. • Modified essay questions. 12 15.0 Diagram to show Curriculum Map for Bachelor of Science in Medical Radiography 1st Year Semester I Semester II Recess Term Block 1 Block 2 FOM 1111 BMR 1113 FOM 1212 Introduction to Health Radiography of the Axial Cardiovascular & Professional Education Appendicular Skeleton, Respiratory systems & Ethics 3 Wks, 3 CU the chest & Abdomen 5 Wks, 5 CU 5 Wks, 5 CU BMR 1112 FOM 1114 Physics of Imaging & Principles of Nursing Ionizing Radiation & First Aid 5 Wks, 5 CU 2 Wks, 2 CU Block 3 FOM 1211 FOM 1213 Digestion, Nutrition Foundations of & Metabolism Behavioural 5 Wks, 5 CU Sciences 5 Wks, 5 CU FOM 1311 Introduction to Community Health I 4 Wks, 4 CU FOM 1312 Introduction to Community Health II 4 Wks, 4 CU 38 Wks 38 CU 2nd year Block 1 BMR 2111 FOM 2112 FOM 2113 BMR 2211 Pathology Reproductive Head Clinical Ultra for Radio& Urinary & Neck Sound of the graphers Abdomen 5 Wks, 5 CU 5 Wks, 5 CU 5 Wks,5 CU 5 wks, 5 CU Block 2 Block 3 FOM 2212 FOM 223 BMR 2214 BMR 2311 Neurolocomotor Community Equipment Pharmacology Diagnosis & maintenance for Radiographers Communication 5Wks, 5 CU BMR 3212 Special Radiological procedures & servicing 3 Wks, 3 CU 2 Wks 2 CU 3 CU, 3 Wks 5 Wks, 5 CU 38 Wks 38 CU 3rd Year Block 2 Block 1 BMR 3111 Radiographic Photography & Imaging Equipment 5 Wks, 5 CU BMR 3112 Radiation Protection & Public Health 5 Wks, 5 CU BMR 3114 Therapy Equipment & Technique I 5 Wks, 5 CU BMR 3113 Clinical CT & MRI 5 Wks 5 CU BMR 3211 Obstetric & Gynecological Ultrasound 5 Wks, 5CU BMR 3212 Ultrasound of Small parts, neonatal Brain & Echocardiography 5 Wks, 5 CU BMR 3213 Nuclear Medicine 5 Wks, 5 CU BMR 3215 Therapy Equipment & Technique II 5 Wks, 5 CU BMR 3216 Oncology & Radiobiology 5 Wks, 5 CU BMR 3217 Advanced Therapy Technique 5 Wks, 5 CU 30 Wks 30 CU 14 16.0. CURRICULUM IMPLEMENTATION STRUCTURE This depicts allocation of time to various curricula activities. The activities and their symbols are shown below: Clinical sessions are shown as clinical hours (Cl.H) Overview lectures and seminars are shown as LH (lecture hours) Skills laboratory activities, practicals and clinical exposure are shown as PH (practical hours) Tutorials sessions are shown as TH (tutorial hours) Self directed learning is shown as SH (self-study hours) 1 1 2 2 2 1 Clinical hour = 1 contact hour Lecture hour = 1 contact hour Tutorial hours = 1 contact hour Practical hours = 1 contact hour Self study hours = 1 contact hour Credit unit = 15 contact hours Year 1 Block 1 Semester I FOM 11 11 Introduction to Health Professionals Education & Ethics BMR 1112 Physics of Imaging & Ionizing Radiation Radiography of the Axial, Appendicular Skeleton, the Chest & Abdomen Principles of Nursing & First Aid BMR 1113 FOM 1114 Total Block 2 Semester II FOM 1212 FOM 1211 FOM 1213 Cardiovascular Respiratory Systems Digestion, Nutrition and Metabolism Foundations of Behavioural Sciences LH 3 Cl.H 5 TH 18 PH 12 SH 44 CH 45 CU 3 5 30 40 70 75 5 5 30 40 70 75 5 2 6 8 16 12 30 2 15 LH 5 5 5 Cl.H 15 15 15 TH 30 30 30 PH 20 20 20 SH 60 60 60 CH 75 75 75 CU 5 5 5 Total Block 3 Recess Term FOM 1311 Introduction to Community Health I FOM 1312 Introduction to Community Health II Total 15 LH 2 2 Cl.H 12 12 TH 24 24 PH 32 30 SH 36 36 CH 60 60 CU 4 4 8 15 Year 2 Block 1 Semester I BMR 2111 Pathology for Radiographers FOM 2112 FOM 2113 Total Reproductive & Urinary Head & Neck Block 2 Semester II BMR 2211 Clinical Ultra Sound of the Abdomen FOM 2212 FOM 2213 Neurolocomotor Community Diagnosis & Communication Equipment Maintenance & Service BMR 2214 LH 5 5 5 Cl.H LH 5 3 5 Cl.H Pharmacology for Radiographers BMR 2312 Special Radiological Procedures Year 3 Block 1 Semester I BMR 3111 BMR 3112 BMR 3113 Total Radiographic Photography & Imaging Equipment Radiation Protection & Public Health Clinical CT & MRI Block 2 Semester II BMR 3211 Obstetric & Gynaecological Ultrasound BMR 3212 Ultrasound of Small Parts, Neonatal Brain & Echocardiography Nuclear Medicine BMR 3213 Total Year 3 Block 1 Therapy Semester I BMR 3114 Therapy Equipment & Technique I BMR 3112 BMR 3113 Total Radiation Protection & Public Health Clinical CT & MRI PH 40 20 20 SH 70 70 70 CH 75 75 75 CU 5 5 5 15 TH 30 30 18 PH 40 20 12 SH 70 60 36 CH 75 75 45 CU 5 5 3 12 20 24 30 2 LH 3 5 TH 18 30 PH 30 40 SH 36 60 CH 45 75 CU 3 5 LH 5 TH 30 PH 40 SH 70 CH 75 CU 5 5 5 30 30 40 40 70 70 75 75 5 5 15 LH 5 5 TH 30 30 PH 40 40 SH 70 70 CH 75 75 CU 5 5 5 30 40 70 75 5 15 10 10 15 9 2 Block 3 Recess Term BMR 2311 TH 30 30 30 LH 5 5 5 TH 30 30 30 PH 40 40 40 SH 70 70 70 CH 75 75 75 CU 5 5 5 15 16 Block 2 Semester II BMR 3215 Therapy Equipment & Technique II BMR 3216 BMR 3217 Oncology & Radiobiology Advanced Therapy Technique LH 5 5 5 TH 30 30 30 PH 40 40 40 SH 70 70 70 CH 75 75 75 CU 5 5 5 17